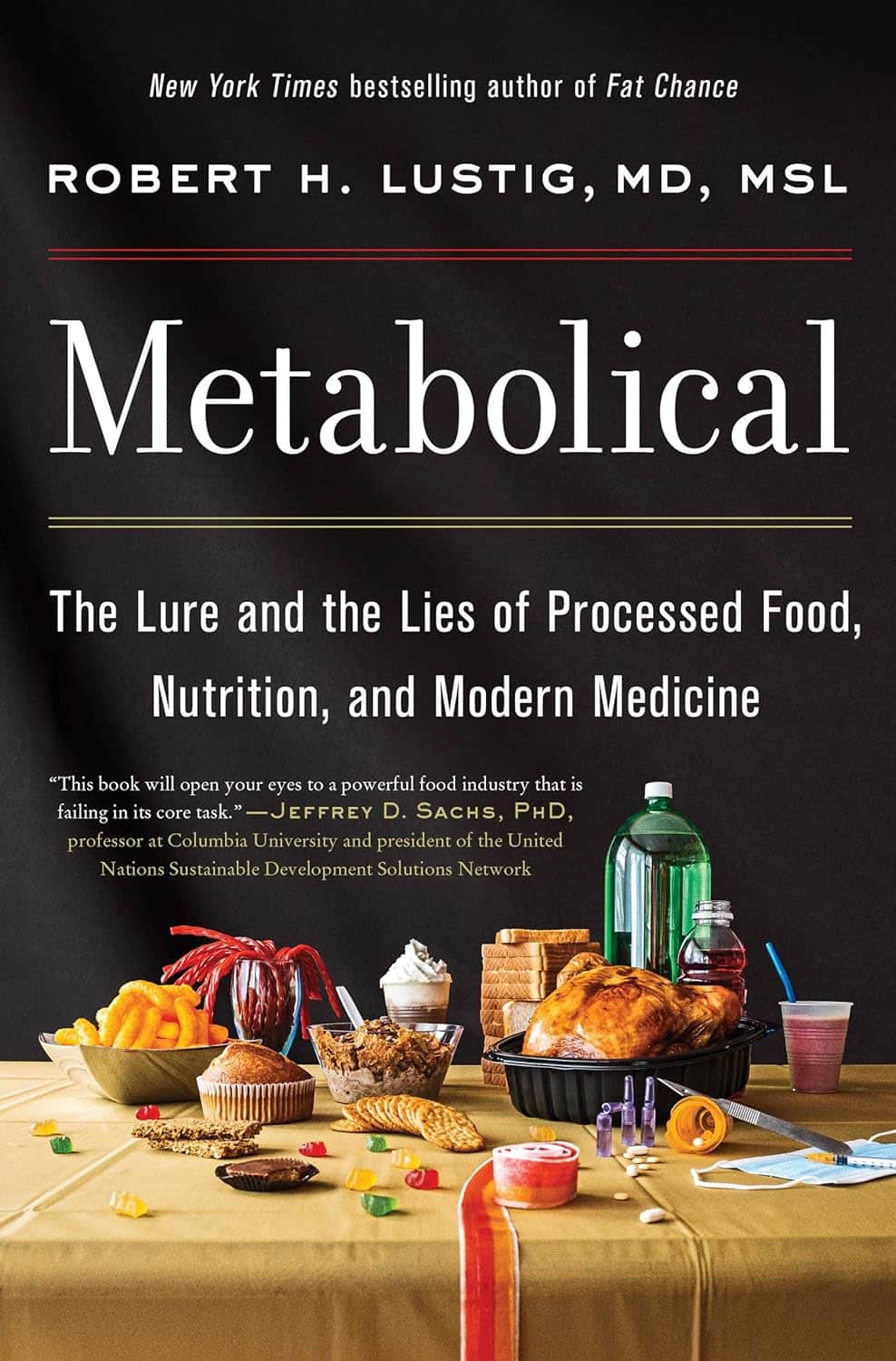
Metabolical – by Dr. Robert Lustig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of this book itself is not novel: processed food is bad, food giants lie to us, and eating better makes us less prone to disease (especially metabolic disease).
What this book does offer that’s less commonly found is a comprehensive guide, a walkthrough of each relevant what and why and how, with plenty of good science and practical real-world examples.
In terms of unique selling points, perhaps the greatest strength of this book is its focus on two things in particular that affect many aspects of health: looking after our liver, and looking after our gut.
The style is… A little dramatic perhaps, but that’s just the style; there’s no hyperbole, he is stating well-established scientific facts.
Bottom line: very much of chronic disease would be a lot less diseasey if we all ate with these aspects of our health in mind. This book’s a comprehensive guide to that.
Click here to check out Metabolical, and let food be thy medicine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Water Fluoridation, Atheroma, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I watched a documentary recently on Fluoride in our drinking water & the dangers of it. Why are we poisoning our water?❞
This is a great question, and it certainly is controversial. It sounds like the documentary you watched was predominantly or entirely negative, but there’s a lot of science to back both sides of this, and it’s not even that the science is contradictory (it’s not). It’s that what differs is people’s opinions about whether benefiting one thing is worth creating a risk to another, and that means looking at:
- What is the risk associated with taking no action (error of omission)?
- What is the risk associated with taking an action (error of commission)?
The whole topic is worth a main feature, but to summarize a few key points:
- Water fluoridation is considered good for the prevention of dental cavities
- Water fluoridation aims to deliver fluoride and doses far below dangerous levels
- This requires working on consumer averages, though
- ”Where do we put the safety margins?” is to some extent a subjective question, in terms of trading off one aspect of health for another
- Too much fluoride can also be bad for the teeth (at least cosmetically, creating little white* spots)
- Detractors of fluoride tend to mostly be worried about neurological harm
- However, the doses in public water supplies are almost certainly far below the levels required to cause this harm.
- That said, again this is working on consumer averages, though.
- However, the doses in public water supplies are almost certainly far below the levels required to cause this harm.
- A good guide is: watch your teeth! Those white* spots will be “the canary in the coal mine” of more serious harm that could potentially come from higher levels due to overconsumption of fluorine.
*Teeth are not supposed to be pure white. The “Hollywood smile” is a lie. Teeth are supposed to be a slightly off-white, ivory color. Anything whiter than that is adding something else that shouldn’t be there, or stripping something off that should be there.
❝How does your diet change clean out your arteries of the bad cholesterol?❞
There’s good news and bad news here, and they can both be delivered with a one-word reply:
Slowly.
Or rather: what’s being cleaned out is mostly not the LDL (bad) cholesterol, but rather, the result of that.
When our diet is bad for cardiovascular health, our arteries get fatty deposits on their walls. Cholesterol gets stuck here too, but that’s not the main physical problem.
Our body’s natural defenses come into action and try to clean it up, but they (for example macrophages, a kind of white blood cell that consumes invaders and then dies, before being recycled by the next part of the system) often get stuck and become part of the buildup (called atheroma), which can lead to atherosclerosis and (if calcium levels are high) hardening of the arteries, which is the worst end of this.
This can then require medical attention, precisely because the body can’t remove it very well—especially if you are still maintaining a heart-unhealthy diet, thus continuing to add to the mess.
However, if it is not too bad yet, yes, a dietary change alone will reverse this process. Without new material being added to the arterial walls, the body’s continual process of rejuvenation will eventually fix it, given time (free from things making it worse) and resources.
In fact, your arteries can be one of the quickest places for your body to make something better or worse, because the blood is the means by which the body moves most things (good or bad) around the body.
All the more reason to take extra care of it, since everything else depends on it!
You might also like our previous main feature:
Share This Post
-
Running: Getting Started – by Jeff Galloway
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, running is surely one of the easiest sports to get into, for most people. You put one foot in front of the other, repeat, and pick up the pace.
However, many people do not succeed. They head out of the door (perhaps on January the first), push themselves a little, experience runner’s high, think “this is great”, and the next day wake up with some minor aches and no motivation. This book is here to help you bypass that stage.
Jeff Galloway has quite a series of books, but the others seem derivative of this one. So, what makes this one special?
It’s quite comprehensive; it covers (as the title promises) getting started, setting yourself up for success, finding what level your ability is at safely rather than guessing and overdoing it, and building up from there.
He also talks about what kit you’ll want; this isn’t just about shoes, but even “what to wear when the weather’s not good” and so forth; he additionally shares advice about diet, exercise on non-running days, body maintenance (stretching and strengthening), troubleshooting aches and pains, and running well into one’s later years.
Bottom line: if you’d like to take up running but it seems intimidating (perhaps for reasons you can’t quite pin down), this book will take care of all those things, and indeed get you “up and running”.
Click here to check out Running: Getting Started, and get started!
Share This Post
-
The Menopause Manifesto – by Dr. Jen Gunter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From the subtitle, you may wonder: with facts and feminism? Is this book about biology or sociology?
And the answer is: both. It’s about biology, principally, but without ignoring the context. We do indeed “live in a society”, and that affects everything from our healthcare options to what is expected of us as women.
So, as a warning: if you dislike science and/or feminism, you won’t like this book.
Dr. Jen Gunter, herself a gynaecologist, is here to arm us with science-based facts, to demystify an important part of life that is commonly glossed over.
She talks first about the what/why/when/how of menopause, and then delivers practical advice. She also talks about the many things we can (and can’t!) usefully do about symptoms we might not want, and how to look after our health overall in the context of menopause. We learn what natural remedies do or don’t work and/or can be actively harmful, and we learn the ins and outs of different hormone therapy options too.
Bottom line: no matter whether you are pre-, peri-, or post-menopausal, this is the no-BS guide you’ve been looking for. Same goes if you’re none of the above but spend any amount of time close to someone who is.
Share This Post
Related Posts
-
Superfood Kale & Dill Pâté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us could do with eating more greens a lot of the time, but it’s not always easy to include them. This kale and dill pâté brings a healthy dose of green in luxurious style, along with abundant phytochemicals and more!
You will need
- 2 handfuls kale, stalks removed
- 1 cup soft cheese (you can use our Healthy Plant-Based Cream Cheese recipe if you like)
- 2 tbsp fresh dill, chopped
- 1 tsp capers
- 1 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Steam the kale for about 5 minutes or until wilted and soft. Run under cold water to halt the cooking process.
2) Combine all the ingredients, including the kale you just blanched, in a food processor and blitz to make a smooth pâté.
3) Serve with oatcakes or vegetable sticks, or keep in the fridge to enjoy it later:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Everyone You Don’t Like Is A Narcissist
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how psychiatry tends to name disorders after how they affect other people, rather than how they affect the bearer, and this is most exemplified when it comes to personality disorders. For example:
“You have a deep insecurity about never being good enough, and you constantly mess up in your attempt to overcompensate? You may have Evil Bastard Disorder!”
“You have a crippling fear of abandonment and that you are fundamentally unloveable, so you do all you can to try to keep people close? You must have Manipulative Bitch Disorder!”
See also: Miss Diagnosis: Anxiety, ADHD, & Women
Antisocial DiagnosesThese days, it is easy to find on YouTube countless videos of how to spot a narcissist, with a list of key traits that all mysteriously describe exactly the exes of everyone in the comments.
And these days it is mostly “narcissist”, because “psychopath” and “sociopath” have fallen out of popular favor a bit:
- perhaps for coming across as overly sensationalized, and thus lacking credibility
- perhaps because “Narcissistic Personality Disorder (NPD)” exists in the DSM-5 (the US’s latest “Diagnostic and Statistical Manual of Mental Disorders”), while psychopathy and sociopathy are not mentioned as existing.
You may be wondering: what do “psychopathy” and “sociopathy” mean?
And the answer is: they mean whatever the speaker wants them to mean. Their definitions and differences/similarities have been vigorously debated by clinicians and lay enthusiasts alike for long enough that the scientific world has pretty much given up on them and moved on.
Stigma vs pathology
Because of the popular media (and social media) representation of NPD, it is easy to armchair diagnose one’s relative/ex/neighbor/in-law/boss/etc as being a narcissist, because the focus is on “narcissists do these bad things that are mean to people”.
If the focus were instead on “narcissists have cripplingly low self-esteem, and are desperate to not show weakness in a world they have learned is harsh and predatory”, then there may not be so many armchair diagnoses—or at the very least, the labels may be attached with a little more compassion, the same way we might with other mental health issues such as depression.
Not that those with depression get an easy time of it socially either—society’s response is generally some manner of “aren’t you better yet, stop being lazy”—but at the very least, depressed people are not typically viewed with hatred.
A quick aside: if you or someone you know is struggling with depression, here are some things that actually help:
The Mental Health First-Aid You’ll Hopefully Never Need
The disorder is not the problem
Maybe your relative, ex, neighbor, etc really is clinically diagnosable as a narcissist. There are still two important things to bear in mind:
- After centuries of diagnosing people with mental health maladies that we now know don’t exist per se (madness, hysteria, etc), and in recent decades countless revisions to the DSM and similar tomes, thank goodness we now have the final and perfect set of definitions that surely won’t be re-written in the next few years or so ← this is irony; it will absolutely be re-written numerous times yet because of course it’s still not a magically perfect descriptor of the broad spectrum of human nature
- The disorder is not the problem; the way they treat (or have treated) you is the problem.
For example, let’s take a key thing generally attributed to narcissists: a lack of empathy
Now, empathy can be divided into:
- affective empathy: the ability to feel what other people are feeling
- cognitive empathy: the ability to intellectually understand what other people are feeling (akin to sympathy, which is the same but with the requisite of having experienced the thing in question oneself)
A narcissist (as well as various other people without NPD) will typically have negligible affective empathy, and their cognitive empathy may be a little sluggish too.
Sluggish = it may take them a beat longer than most people, to realize what an external signifier of emotions means, or correctly guess how something will be felt by others. This can result in gravely misspeaking (or inappropriately emoting), after failing to adequately quickly “read the room” in terms of what would be a socially appropriate response. To save face, they may then either deny/minimize the thing they just said/did, or double-down on it and go on [what for them feels like] the counterattack.
As to why this shutting off of empathy happens: they have learned that the world is painful, and that people are sources of pain, and so—to avoid further pain—have closed themselves off to that, often at a very early age. This will also apply to themselves; narcissists typically have negligible self-empathy too, which is why they will commonly make self-destructive decisions, even while trying to put themselves first.
Important note on how this impacts other people: the “Golden Rule” of “treat others as you would wish to be treated” becomes intangible, as they have no more knowledge of their own emotional needs than they do of anyone else’s, so cannot make that comparison.
Consider: if instead of being blind to empathy, they were colorblind… You would probably not berate them for buying green apples when you asked for red. They were simply incapable of seeing that, and consequently made a mistake. So it is when it’s a part of the brain that’s not working normally.
So… Since the behavior does adversely affect other people, what can be done about it? Even if “hate them for it and call for their eradication from the face of the Earth” is not a reasonable (or compassionate) option, what is?
Take the bull by the horns
Above all, and despite all appearances, a narcissist’s deepest desire is simply to be accepted as good enough. If you throw them a life-ring in that regard, they will generally take it.
So, communicate (gently, because a perceived attack will trigger defensiveness instead, and possibly a counterattack, neither of which are useful to anyone) what behavior is causing a problem and why, and ask them to do an alternative thing instead.
And, this is important, the alternative thing has to be something they are capable of doing. Not merely something that you feel they should be capable of doing, but that they are actually capable of doing.
- So not: “be a bit more sensitive!” because that is like asking the colorblind person to “be a bit more observant about colors”; they are simply not capable of it and it is folly to expect it of them, because no matter how hard they try, they can’t.
- But rather: “it upsets me when you joke about xyz; I know that probably doesn’t make sense to you and that’s ok, it doesn’t have to. I am asking, however, if you will please simply refrain from joking about xyz. Would you do that for me?”
Presented with such, it’s much more likely that the narcissist will drop their previous attempt to be good enough (by joking, because everyone loves someone with a sense of humor, right?) for a new, different attempt to be good enough (by showing “behold, look, I am a good person and doing the thing you asked, of which I am capable”).
That’s just one example, but the same methodology can be applied to most things.
For tricks pertaining to how to communicate such things without causing undue resistance, see:
Seriously Useful Communication Skills
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tight hamstrings are often not actually due to hamstring issues, but rather, are often being limited by the sciatic nerve. This video offers a home test to determine if the sciatic nerve is causing mobility problems (and how to improve it, if so):
The Connection
Try this test:
- Sit down with a slumped posture.
- Extend one leg with the ankle flexed.
- Note any stretching or pulling sensation behind the knee or in the calf.
- Bring your head down to your chest
If this increases the sensation, it likely indicates sciatic nerve involvement.
If only the hamstrings are tight, head movement won’t change the stretch sensation.
This is because the nervous system is a continuous structure, so head movement can affect nerve tension throughout the body. While this can cause problems, it can also be integral in the solution. Here are two ways:
- Flossing method: sit with “poor” slumped posture, extend the knee, keep the ankle flexed, and lift the head to relieve nerve tension. This movement helps the sciatic nerve slide without stretching it.
- Even easier method: lie on your back, grab behind the knee, and extend the leg while extending the neck. This position avoids compression in the gluteal area, making it suitable for severely compromised nerves. Perform the movement without significant stretching or pain.
In both cases: move gently to avoid straining the nerve, which can worsen muscle tension. Do 10 repetitions per leg, multiple times a day; after a week, increase to 20 reps.
A word of caution: speak with your doctor before trying these exercises if you have underlying neurological diseases, cut or infected nerves, or other severe conditions.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Exercises for Sciatica Pain Relief
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: