Driving under the influence of marijuana: An explainer and research roundup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Update 1: On May 16, 2024, the U.S. Department of Justice sent a proposed rule to the Federal Register to downgrade marijuana from a Schedule I to a Schedule III drug. This is the first step in a lengthy approval process that starts with a 60-day comment period.
Update 2: Two recent research studies were added to the “Studies on marijuana and driving” section of this piece on July 18, 2024.
As marijuana use continues to rise and state-level marijuana legalization sweeps the U.S., researchers and policymakers are grappling with a growing public safety concern: marijuana-impaired driving.
As of April 2023, 38 U.S. states had legalized medical marijuana and 23 had legalized its recreational use, according to the National Conference of State Legislatures. Recreational or medical marijuana measures are on the ballot in seven states this year.
The issue of marijuana-impaired driving has not been an easy one to tackle because, unlike alcohol, which has well-established thresholds of impairment, the metrics for marijuana’s effects on driving remain rather elusive.
“We don’t have that kind of deep knowledge right now and it’s not because of lack of trying,” says Dr. Guohua Li, professor of epidemiology and the founding director of the Center for Injury Science and Prevention at Columbia University.
“Marijuana is very different from alcohol in important ways,” says Li, who has published several studies on marijuana and driving. “And one of them is that the effect of marijuana on cognitive functions and behaviors is much more unpredictable than alcohol. In general, alcohol is a depressant drug. But marijuana could act on the central nervous system as a depressant, a stimulant, and a hallucinogenic substance.”
Efforts to create a breathalyzer to measure the level of THC, the main psychoactive compound found in the marijuana plant, have largely failed, because “the THC molecule is much bigger than ethanol and its behavior after ingestion is very different from alcohol,” Li says.
Currently, the two most common methods used to measure THC concentration to identify impaired drivers are blood and saliva tests, although there’s ongoing debate about their reliability.
Marijuana, a term interchangeably used with cannabis, is the most commonly used federally illegal drug in the U.S.: 48.2 million people, or about 18% of Americans reported using it at least once in 2019, according to the latest available data from the Centers for Disease Control and Prevention. Worldwide, 2.5% of the population consumes marijuana, according to the World Health Organization.
Marijuana is legal in several countries, including Canada, where it was legalized in 2018. Despite state laws legalizing cannabis, it remains illegal at the federal level in the U.S.
As states grapple with the contentious issue of marijuana legalization, the debate is not just about public health, potential tax revenues and economic interests. At the heart of the discussion is also the U.S. criminal justice system.
Marijuana is shown to have medicinal qualities and, compared with substances like alcohol, tobacco, and opioids, it has relatively milder health risks. However, it’s not risk-free, a large body of research has shown.
Marijuana consumption can lead to immediate effects such as impaired muscle coordination and paranoia, as well as longer-term effects on mental health and cognitive functions — and addiction. As its use becomes more widespread, researchers are trying to better understand the potential hazards of marijuana, particularly for younger users whose brains are in critical stages of development.
Marijuana and driving
The use of marijuana among drivers, passengers and pedestrians has increased steadily over the past two decades, Li says.
Compared with the year 2000, the proportion of U.S. drivers on the road who are under the influence of marijuana has increased by several folds, between five to 10 times, based on toxicology testing of people who died in car crashes, Li says.
A 2022 report from the National Transportation Safety Board finds alcohol and cannabis are the two most commonly detected drugs among drivers arrested for impaired driving and fatally injured drivers. Most drivers who tested positive for cannabis also tested positive for another potentially impairing drug.
“Although cannabis and many other drugs have been shown to impair driving performance and are associated with increased crash risk, there is evidence that, relative to alcohol, awareness about the potential dangers of driving after using other drugs is lower,” according to the report.
Indeed, many U.S. adults perceive daily marijuana use or exposure to its smoke safer than tobacco, even though research finds otherwise.
Several studies have demonstrated marijuana’s impact on driving.
Marijuana use can reduce the drivers’ ability to pay attention, particularly when they are performing multiple tasks, research finds. It also slows reaction time and can impair coordination.
“The combination is that you potentially have people who are noticing hazards later, braking slower and potentially not even noticing hazards because of their inability to focus on competing things on the road,” says Dr. Daniel Myran, an assistant professor at the Department of Family Medicine and health services researcher at the University of Ottawa.
In a study published in September in JAMA Network Open, Myran and colleagues find that from 2010 to 2021 the rate of cannabis-involved traffic injuries that led to emergency department visits in Ontario, Canada, increased by 475%, from 0.18 per 1,000 traffic injury emergency department visits in 2010 to 1.01 visits in 2021.
To be sure, cannabis-involved traffic injuries made up a small fraction of all traffic injury-related visits to hospital emergency departments. Out of 947,604 traffic injury emergency department visits, 426 had documented cannabis involvement.
Myran cautions the increase shouldn’t be solely attributed to marijuana legalization. It captures changing societal attitudes toward marijuana and acceptance of cannabis use over time in the lead-up to legalization. In addition, it may reflect an increasing awareness among health care providers about cannabis-impaired driving, and they may be more likely to ask about cannabis use and document it in medical charts, he says.
“When you look at the 475% increase in cannabis involvement in traffic injuries, rather than saying legalizing cannabis has caused the roads to be unsafe and is a public health disaster, it’s that cannabis use appears to be growing as a risk for road traffic injuries and that there seem to be more cannabis impaired drivers on the road,” Myran says. “Legalization may have accelerated this trend. Faced with this increase, we need to think about what are public health measures and different policy interventions to reduce harms from cannabis-impaired driving.”
Setting a legal limit for marijuana-impaired driving
Setting a legal limit for marijuana-impaired driving has not been easy. Countries like Canada and some U.S. states have agreed upon a certain level of THC in blood, usually between 1 to 5 nanograms per milliliter. Still, some studies have found those limits to be weak indicators of cannabis-impaired driving.
When Canada legalized recreational marijuana in 2018, it also passed a law that made it illegal to drive with blood THC levels of more than 2 nanograms. The penalties are more severe for blood THC levels above 5 nanograms. The blood test is done at the police station for people who are pulled over and are deemed to be drug impaired.
In the U.S., five states — Ohio, Illinois, Montana, Washington and Nevada — have “per se laws,” which set a specific amount of THC in the driver’s blood as evidence of impaired driving, according to the National Conference of State Legislatures. That limit ranges between 2 and 5 nanograms of THC per milliliter of blood.
Colorado, meanwhile, has a “permissible inference law,” which states that it’s permissible to assume the driver was under the influence if their blood THC level is 5 nanograms per milliliter or higher, according to NCSL.
Twelve states, most which have legalized some form of marijuana of use, have zero tolerance laws for any amount of certain drugs, including THC, in the body.
The remaining states have “driving under the influence of drugs” laws. Among those states, Alabama and Michigan, have oral fluid roadside testing program to screen drivers for marijuana and other drugs, according to NCSL.
In May this year, the U.S. Department of Transportation published a final rule that allows employers to use saliva testing for commercially licensed drivers, including truck drivers. The rule, which went into effect in June, sets the THC limit in saliva at 4 nanograms.
Saliva tests can detect THC for 8 to 24 hours after use, but the tests are not perfect and can results in false positives, leading some scientists to argue against using them in randomly-selected drivers.
In a 2021 report, the U.S. National Institute of Justice, the research and development arm of the Department of Justice, concluded that THC levels in bodily fluids, including blood and saliva “were not reliable indicators of marijuana intoxication.”
Studies on marijuana and driving
Over the past two decades, many studies have shown marijuana use can impair driving. However, discussions about what’s the best way to measure the level of THC in blood or saliva are ongoing. Below, we highlight and summarize several recent studies that address the issue. The studies are listed in order of publication date. We also include a list of related studies and resources to inform your audiences.
State Driving Under the Influence of Drugs Laws
Alexandra N. Origenes, Sarah A. White, Emma E. McGinty and Jon S. Vernick. Journal of Law, Medicine & Ethics, July 2024.
Summary: As of January 2023, 33 states and D.C. had a driving under the influence of drugs law for at least one drug other than cannabis. Of those, 29 states and D.C. had a law specifically for driving under the influence of cannabis, in addition to a law for driving under the influence of other drugs. Four states had a driving under the influence of drug laws, excluding cannabis. Meanwhile, 17 states had no law for driving under the influence of drugs, including cannabis. “The 17 states lacking a DUID law that names specific drugs should consider enacting such a law. These states already have expressed their concern — through legislation — with drug-impaired driving. However, failure to name specific drugs is likely to make the laws more difficult to enforce. These laws may force courts and/or law enforcement to rely on potentially subjective indicators of impairment,” the authors write.
Associations between Adolescent Marijuana Use, Driving After Marijuana Use and Recreational Retail Sale in Colorado, USA
Lucas M. Neuroth, et al. Substance Use & Misuse, October 2023.
Summary: Researchers use data from four waves (2013, 2015, 2017 and 2019) of the Healthy Kids Colorado Survey, including 47,518 students 15 and older who indicated that they drove. They find 20.3% of students said that they had used marijuana in the past month and 10.5% said they had driven under the influence of marijuana. They find that the availability of recreational marijuana in stores was associated with an increased prevalence of using marijuana one to two times in the past month and driving under the influence of marijuana at least once. “Over the study period, one in ten high school age drivers engaged in [driving after marijuana use], which is concerning given the high risk of motor vehicle-related injury and death arising from impaired driving among adolescents,” the authors write.
Are Blood and Oral Fluid Δ9-tetrahydrocannabinol (THC) and Metabolite Concentrations Related to Impairment? A Meta-Regression Analysis
Danielle McCartney, et al. Neuroscience & Biobehavioral Reviews, March 2022.
Summary: Commonly used THC measurements may not be strong indicators of driving impairment. While there is a relationship between certain biomarkers like blood THC concentrations and impaired driving, this correlation is often weak. The study underscores the need for more nuanced and comprehensive research on this topic, especially as cannabis usage becomes more widespread and legally accepted.
The Effects of Cannabis and Alcohol on Driving Performance and Driver Behaviour: A Systematic Review and Meta-Analysis
Sarah M. Simmons, Jeff K. Caird, Frances Sterzer and Mark Asbridge. Addiction, January 2022.
Summary: This meta-analysis of experimental driving studies, including driving simulations, confirms that cannabis impairs driving performance, contrary to some beliefs that it might enhance driving abilities. Cannabis affects lateral control and speed — typically increasing lane excursions while reducing speed. The combination of alcohol and marijuana appears worse than either alone, challenging the idea that they cancel each other out.
Cannabis Legalization and Detection of Tetrahydrocannabinol in Injured Drivers
Jeffrey R. Brubacher, et al. The New England Journal of Medicine, January 2022.
Summary: Following the legalization of recreational marijuana in Canada, there was a notable increase in injured drivers testing positive for THC, especially among those 50 years of age or older. This rise in cannabis-related driving incidents occurred even with new traffic laws aiming to deter cannabis-impaired driving. This uptick began before legalization became official, possibly due to perceptions that cannabis use was soon-to-be legal or illegal but not enforced. The data suggests that while legalization has broad societal impacts, more comprehensive strategies are needed to deter driving under the influence of cannabis and raise public awareness about its risks.
Cannabis and Driving
Godfrey D. Pearlson, Michael C. Stevens and Deepak Cyril D’Souza. Frontiers in Psychiatry, September 2021.
Summary: Cannabis-impaired driving is a growing public health concern, and studies show that such drivers are more likely to be involved in car crashes, according to this review paper. Drivers are less affected by cannabis than they are by alcohol or cocaine, but the problem is expected to escalate with increasing cannabis legalization and use. Unlike alcohol, THC’s properties make it challenging to determine direct impairment levels from testing results. Current roadside tests lack precision in detecting genuine cannabis-impaired drivers, leading to potential wrongful convictions. Moreover, there is a pressing need for research on the combined effects of alcohol and cannabis on driving, as well as the impact of emerging popular forms of cannabis, like concentrates and edibles. The authors recommend public awareness campaigns about the dangers of driving under the influence of cannabis, similar to those against drunk driving, to address misconceptions. Policymakers should prioritize science-based decisions and encourage further research in this domain.
Demographic And Policy-Based Differences in Behaviors And Attitudes Towards Driving After Marijuana Use: An Analysis of the 2013–2017 Traffic Safety Culture Index
Marco H. Benedetti, et al. BMC Research Notes, June 2021.
Summary: The study, based on a U.S. survey, finds younger, low-income, low-education and male participants were more tolerant of driving after marijuana consumption. Notably, those in states that legalized medical marijuana reported driving after use more frequently, aligning with studies indicating a higher prevalence of THC detection in drivers from these states. Overall, while the majority perceive driving after marijuana use as dangerous, not all research agrees on its impairment effects. Existing studies highlight that marijuana impacts motor skills and executive functions, yet its direct correlation with crash risk remains debated, given the variations in individual tolerance and how long THC remains in the system.
Driving Under the Influence of Cannabis: A Framework for Future Policy
Robert M. Chow, et al.Anesthesia & Analgesia, June 2019.
Summary: The study presents a conceptual framework focusing on four main domains: legalization, driving under the influence of cannabis, driver impairment, and motor vehicle accidents. With the growing legalization of cannabis, there’s an anticipated rise in cannabis-impaired driving cases. The authors group marijuana users into infrequent users who show significant impairment with increased THC blood levels, chronic users with minimal impairment despite high THC levels, and those with consistent psychomotor deficits. Current challenges lie in the lack of standardized regulation for drivers influenced by cannabis, primarily because of state-to-state variability and the absence of a federal statutory limit for blood THC levels. European nations, however, have established thresholds for blood THC levels, ranging from 0.5 to 50.0 micrograms per liter depending on whether blood or blood serum are tested. The authors suggest the combined use of alcohol and THC blood tests with a psychomotor evaluation by a trained professional to determine impairment levels. The paper stresses the importance of creating a structured policy framework, given the rising acceptance and use of marijuana in society.
Additional research
Cannabis-Involved Traffic Injury Emergency Department Visits After Cannabis Legalization and Commercialization
Daniel T. Myran, et al. JAMA Network Open, September 2023.
Driving Performance and Cannabis Users’ Perception of Safety: A Randomized Clinical Trial
Thomas D. Marcotte, et al. JAMA Psychiatry, January 2022.
Medicinal Cannabis and Driving: The Intersection of Health and Road Safety Policy
Daniel Perkins, et al. International Journal of Drug Policy, November 2021.
Prevalence of Marijuana Use Among Trauma Patients Before and After Legalization of Medical Marijuana: The Arizona Experience
Michael Levine, et al. Substance Abuse, July 2021.
Self-Reported Driving After Marijuana Use in Association With Medical And Recreational Marijuana Policies
Marco H. Benedetti, et al. International Journal of Drug Policy, June 2021.
Cannabis and Driving Ability
Eric L. Sevigny. Current Opinion in Psychology, April 2021.
The Failings of per se Limits to Detect Cannabis-Induced Driving Impairment: Results from a Simulated Driving Study
Thomas R. Arkell, et al. Traffic Injury Prevention, February 2021.
Risky Driving Behaviors of Drivers Who Use Alcohol and Cannabis
Tara Kelley-Baker, et al. Transportation Research Record, January 2021.
Direct and Indirect Effects of Marijuana Use on the Risk of Fatal 2-Vehicle Crash Initiation
Stanford Chihuri and Guohua Li. Injury Epidemiology, September 2020
Cannabis-Impaired Driving: Evidence and the Role of Toxicology Testing
Edward C. Wood and Robert L. Dupont. Cannabis in Medicine, July 2020.
Association of Recreational Cannabis Laws in Colorado and Washington State With Changes in Traffic Fatalities, 2005-2017
Julian Santaella-Tenorio, et al. JAMA Internal Medicine, June 2020.
Marijuana Decriminalization, Medical Marijuana Laws, and Fatal Traffic Crashes in US Cities, 2010–2017
Amanda Cook, Gregory Leung and Rhet A. Smith. American Journal of Public Health, February 2020.
Cannabis Use in Older Drivers in Colorado: The LongROAD Study
Carolyn G. DiGuiseppi, et al. Accident Analysis & Prevention, November 2019.
Crash Fatality Rates After Recreational Marijuana Legalization in Washington and Colorado
Jayson D. Aydelotte, et al. American Journal of Public Health, August 2017.
Marijuana-Impaired Driving: A Report to Congress
National Highway Traffic Safety Administration, July 2017
Interaction of Marijuana And Alcohol on Fatal Motor Vehicle Crash Risk: A Case–Control Study
Stanford Chihuri, Guohua Li and Qixuan Chen. Injury Epidemiology, March 2017.
US Traffic Fatalities, 1985–2014, and Their Relationship to Medical Marijuana Laws
Julian Santaella-Tenorio, et al. American Journal of Public Health, February 2017.
Delays in DUI Blood Testing: Impact on Cannabis DUI Assessments
Ed Wood, Ashley Brooks-Russell and Phillip Drum. Traffic Injury Prevention, June 2015.
Establishing Legal Limits for Driving Under the Influence of Marijuana
Kristin Wong, Joanne E. Brady and Guohua Li. Injury Epidemiology, October 2014.
Cannabis Effects on Driving Skills
Rebecca L. Hartman and Marilyn A. Huestis. Clinical Chemistry, March 2014.
Acute Cannabis Consumption And Motor Vehicle Collision Risk: Systematic Review of Observational Studies and Meta-Analysis
Mark Asbridge, Jill A. Hayden and Jennifer L. Cartwright. The BMJ, February 2012.
Resources for your audiences
The following resources include explainers from federal agencies and national organizations. You’re free to use images and graphics from federal agencies.
- CDC’s main marijuana page.
- CDC’s marijuana data and statistics.
- Marijuana Drug Facts from the National Institute on Drug Abuse.
- Health Effects of Marijuana from the CDC.
- Learn About Marijuana Risks from the Substance Abuse and Mental Health Services Administration.
- Marijuana and Lung Health from the American Lung Association.
- Substance Use Disorder 101 from the U.S. Department of Health & Human Services.
- What You Need To Know About Marijuana Use and Driving from the CDC.
- Does marijuana use affect driving? from the National Institute on Drug Abuse.
- Drug-Impaired Driving from the National Highway Traffic Safety Administration.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oranges vs Lemons – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing oranges to lemons, we picked the oranges.
Why?
In the battle of these popular citrus fruits, there is a clear winner on the nutritional front.
Things were initially promising for lemons when looking at the macros—lemons have a little more fiber while oranges are slightly higher in carbs, but the differences are small and both are very healthy in this regard.
However, alas for this writer who prefers sour fruits to sweet ones (I’m sweet enough already), the micronutrient profiles tell a different story:
In terms of vitamins, oranges have more of vitamins A, B1, B2, B3, B5, B9, E, and choline. In contrast, lemons have a (very) little more vitamin B6. You might be wondering about vitamin C, since both fruits are famous for that—they’re equal on vitamin C. But, with that stack we listed above, oranges clearly win the vitamin category easily.
As for minerals, oranges boast more calcium, copper, magnesium, potassium, selenium, and zinc, while lemons have more iron, manganese, and phosphorus.
Technically lemons also have more sodium, but the numbers are truly miniscule (by coincidence, we discover upon grabbing a calculator, you’d need to eat approximately your own bodyweight in whole lemons to get to the RDA of sodium—and that’s to reach the RDA, not the upper healthy limit) so we’ll overlook the tiny sodium difference as irrelevant. Which means, while closer than the vitamins category, oranges win on minerals with a 6:3 lead over lemons.
Both fruits offer generous helpings of flavonoids and other polyphenols such as naringenin and hesperidin, which have anti-inflammatory properties and more specifically can also reduce allergy symptoms (unless, of course, you are allergic to citrus fruits, which is a relatively rare but extant allergy).
In short: as ever, enjoy both; diversity is great for the health. But if you want to maximize the nutrients you get, it’s oranges.
Want to learn more?
You might like to read:
Lemons vs Limes – Which is Healthier?
Take care!
Share This Post
-
Plant-Based Alternatives for Meat Recipes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How about providing a plant-based alternative when you post meat-based recipes? I appreciate how much you advocate for veggie diets and think offering an alternative with your recipes would support that❞
Glad you’re enjoying! And yes, we do usually do that. But: pardon, we missed one (the Tuna Steak with Protein Salad) because it’d be more than a simple this-for-that substitution, we didn’t already have an alternative recipe up (as with the salmon recipes such as the Chili Hot-Bedded Salmon and Thai Green Curry Salmon Burgers).
Our recipes, by the way, will tend towards being vegan, vegetarian, or at least pescatarian. This is for several reasons:
- Good science suggests the best diet for general purpose good health is one that is mostly plants, with optional moderate amounts of fermented dairy products, fish, and/or eggs.
- Your writer here (it’s me, hi) has been vegan for many years, transitioning to such via pescatarianism and ovo-lacto vegetarianism, and so the skill of cooking meat is least fresh in my memory, meaning I’d not be confident writing about that, especially as cooking meat has the gravest health consequences for messing it up.
Note on biases: notwithstanding this writer being vegan, we at 10almonds are committed to reporting the science as it stands with no agenda besides good health. Hence, there will continue to be unbiased information about animal products’ health considerations, positive as well as negative.
See also: Do We Need Animal Products To Be Healthy?
…as well as, of course, some animal-based classics from our archives including:
We Are Such Stuff As Fish Are Made Of & Eggs: All Things In Moderation?
Finishing with one for the vegans though, you might enjoy:
Which Plant Milk? We Compare 6 Of The Most Popular
Some previous articles you might enjoy meanwhile:
- Pinpointing The Usefulness Of Acupuncture
- Science-Based Alternative Pain Relief
- Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
- What Does Lion’s Mane Actually Do, Anyway?
Take care!
Share This Post
-
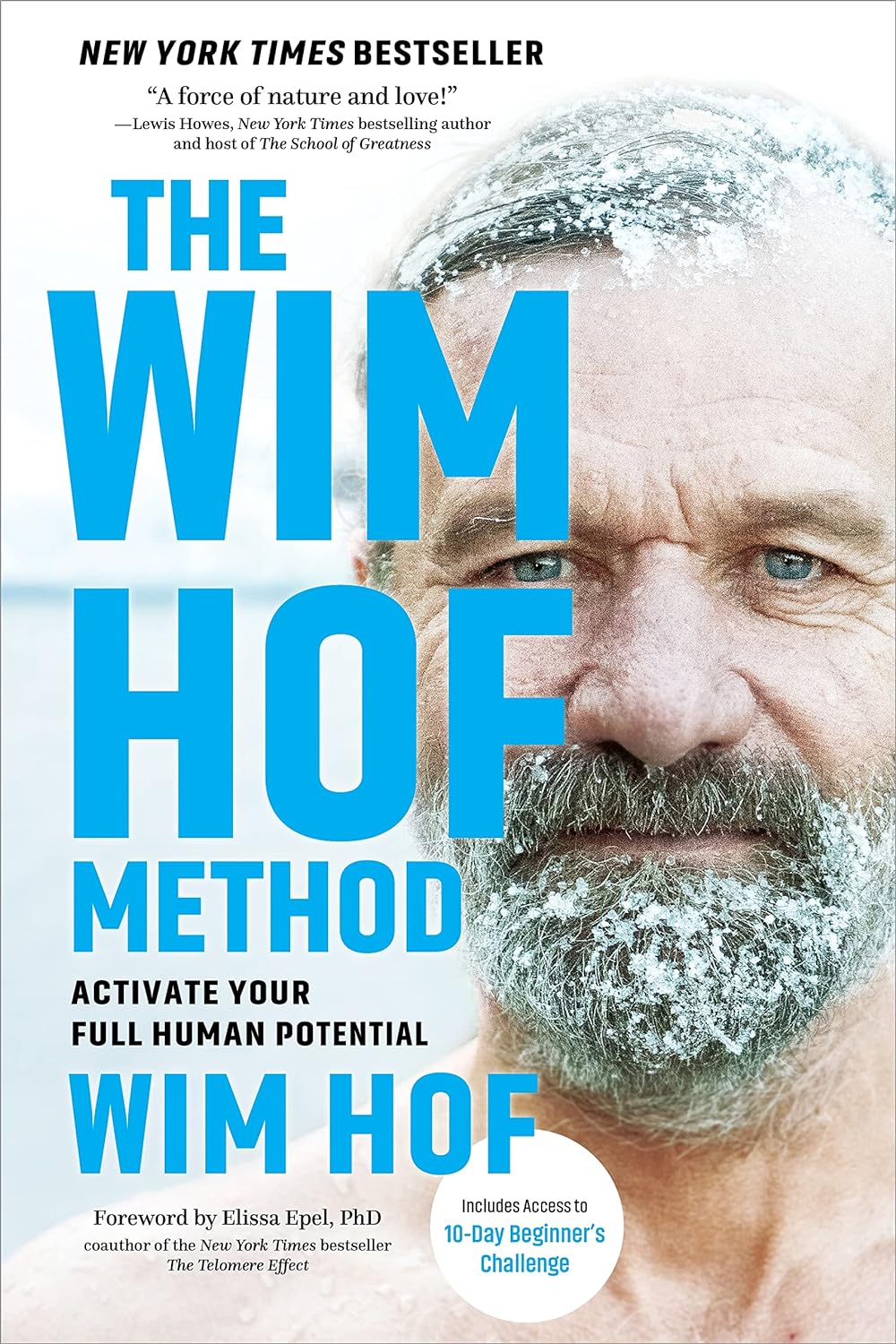
The Wim Hof Method – by Wim Hof
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Wednesday’s main feature, we wrote about the Wim Hof Method, and/but only scratched the surface. Such is the downside of being a super-condensed newsletter! However, it does give us the opportunity to feature the book:
The Wim Hof Method is definitely loudly trumpeted as “up there” with Atomic Habits or How Not To Die in the category of “life-changing” books. Why?
Firstly, it’s a very motivational book. Hof is a big proponent of the notion “if you think you can or you think you can’t, you’re right” idea, practises what he preaches, and makes clear he’s not special.
Secondly, it’s backed up with science. While it’s not a science-heavy book and that’s not the main focus, there are references to studies. Where physiological explanations are given for how certain things work, those explanations are sound. There’s no pseudoscience here, which is especially important for a book of this genre!
What does the book have that our article didn’t? A good few things:
- More about Hof’s own background and where it’s taken him. This is generally not a reason people buy books (unless they are biographies), but it’s interesting nonetheless.
- A lot more advice, data, and information about Cold Therapy and how it can (and, he argues convincingly, should) be built into your life.
- A lot about breathing exercises that we just didn’t cover at all in our article, but is actually an important part of the Wim Hof Method.
- More about stepping through the psychological barriers that can hold us back.
Bottom line: this book offers benefits that stretch into many areas of life, from some simple habits that can be built.
Share This Post
Related Posts
-
Cherries vs Blackberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to blackberries, we picked the blackberries.
Why?
In terms of macros, cherries have more carbs while blackberries have more protein and fiber. The protein of course is a tiny amount and an even tinier difference, and/but it’s worth noting that the fiber isn’t, and blackberries have more than 3x the fiber. So, a win for blackberries in this category.
In the category of vitamins, cherries have more of vitamins A, B1, B2, and B6, while blackberries have more of vitamins B3, B5, B9, C, E, K, and choline. Another win for blackberries.
When it comes to minerals, cherries have a tiny bit more potassium, while blackberries have considerably more calcium, copper, iron, magnesium, manganese, phosphorus, selenium, and zinc. Another easy win for blackberries.
Both fruits have abundant antioxidants, but as many are different, and comparison between them becomes more subjective than we have room for here.
In short, enjoy either or both, but we say blackberries win overall on macro- and micronutrients!
Want to learn more?
You might like to read:
Cherries’ Very Healthy Wealth Of Benefits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Codependent No More – by Melody Beattie
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book review, not a book summary, but first let’s quickly cover a common misconception, because the word “codependent” gets misused a lot in popular parlance:
- What codependence isn’t: “we depend on each other and must do everything together”
- What codependence is:“person 1 has a dependency on a substance (or perhaps a behavior, such as gambling); person 2 is trying to look after person 1, and so has developed a secondary relationship with the substance/behavior. Person 2 is now said to be codependent, because it becomes all-consuming for them too, even if they’re not using the substance/behavior directly”
Funny how often it happens that the reality is more complex than the perception, isn’t it?
Melody Beattie unravels all this for us. We get a compassionate and insightful look at how we can look after ourselves, while looking after another. Perhaps most importantly: how and where to draw a line of what we can and cannot do/change for them.
Because when we love someone, of course we want to fight their battles with them, if not for them. But if we want to be their rock of strength, we can’t get lost in it too, and of course that hurts.
Beatty takes us through these ideas and more, for example:
- How to examine our own feelings even when it’s scary
- How to practice self-love and regain self-worth, while still caring for them
- How to stop being reactionary, step back, and act with purpose
If the book has any weak point, it’s that it repeatedly recommends 12-step programs, when in reality that’s just one option. But for those who wish to take another approach, this book does not require involvement in a 12-step program, so it’s not a barrier to usefulness.
Click here to check out Codependent No More and take care of yourself, too
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Dark Side Of Memory (And How To Make Your Life Better)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Stop Revisiting Those Memories
We’ve talked before about putting the brakes on negative thought spirals (and that’s a really useful technique, so if you weren’t with us yet for that one, we do recommend hopping back and reading it!).
We’ve also talked about optimizing memory, to include making moments unforgettable.
But what about the moments we’d rather forget?
First, a quick note: we have no pressing wish or need to re-traumatize any readers, so if you’ve a pressing reason to think your memories you’d rather forget are beyond the scope of a few hundred words “one quick trick” in a newsletter, feel free to skip this section today.
One more quick note: it is generally not considered healthy to repress important memories. Some things are best worked through consciously in therapy with a competent professional.
Today’s technique is more for things in the category of “do you really need to keep remembering that one time you did something embarrassing 20 years ago?”
That said… sometimes, even when it does come to the management of serious PTSD, therapy can (intentionally, reasonably) throw in the towel on processing all of something big, and instead seek to simply look at minimizing its effect on ongoing life. Again, that’s best undertaken with a well-trained professional, however.
For more trivial annoyances, meanwhile…
Two Steps To Forgetting
The first step:
You may remember that memories are tied to the senses, and the more senses are involved, the more easily and fully we remember a thing. To remember something, therefore, we make sure to pay full attention to all the sensory experience of the memory, bringing in all 5 senses if possible.
To forget, the reverse is true. Drain the memory of color, make it black and white, fuzzier, blurrier, smaller, further away, sterile, silent, gone.
You can make a habit of doing this automatically whenever your unwanted memory resurfaces.
The
secondmissing step:This is the second step, but it’s going to be a missing step. Memories, like paths in a forest, are easier to access the more often we access them. A memory we visit every day will have a well-worn path, easy to follow. A memory we haven’t visited for decades will have an overgrown, sometimes nearly impossible-to-find path.
To labor the metaphor a little: if your memory has literal steps leading to it, we’re going to remove one of the steps now, to make it very difficult to access accidentally. Don’t worry, you can always put the step back later if you want to.
Let’s say you want to forget something that happened once upon a time in a certain workplace. Rather than wait for the memory in question to come up, we’re going to apply the first step that we just learned, to the entire workplace.
So, in this example, you’d make the memory of that workplace drained of color, made black and white, fuzzier, blurrier, smaller, further away, sterile, silent, gone.
Then, you’d make a habit of doing that whenever that workplace nearly comes to mind.
The result? You’re unlikely to accidentally access a memory that occurred in that workplace, if even mentally wandering to the workplace itself causes it to shrivel up and disappear like paper in fire.
Important reminder
The above psychological technique is to psychological trauma what painkillers are to physical pain. It can ease the symptom, while masking the cause. If it’s something serious, we recommend enlisting the help of a professional, rather than “self-medicating” in this fashion.
If it’s just a small annoying thing, though, sometimes it’s easier to just be able to refrain from prodding and poking it daily, forget about it, and enjoy life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: