Knitting helps Tom Daley switch off. Its mental health benefits are not just for Olympians
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olympian Tom Daley is the most decorated diver in Britain’s history. He is also an avid knitter. At the Paris 2024 Olympics Daley added a fifth medal to his collection – and caught the world’s attention knitting a bright blue “Paris 24” jumper while travelling to the games and in the stands.
At the Tokyo Olympics, where Daley was first spotted knitting, he explained its positive impact on his mental health.
It just turned into my mindfulness, my meditation, my calm and my way to escape the stresses of everyday life and, in particular, going to an Olympics.
The mental health benefits of knitting are well established. So why is someone famous like Daley knitting in public still so surprising?

Knitting is gendered
Knitting is usually associated with women – especially older women – as a hobby done at home. In a large international survey of knitting, 99% of respondents identified as female.
But the history of yarn crafts and gender is more tangled. In Europe in the middle ages, knitting guilds were exclusive and reserved for men. They were part of a respected Europe-wide trade addressing a demand for knitted products that could not be satisfied by domestic workers alone.
The industrial revolution made the production of clothed goods cheaper and faster than hand-knitting. Knitting and other needle crafts became a leisure activity for women, done in the private sphere of the home.
World Wars I and II turned the spotlight back on knitting as a “patriotic duty”, but it was still largely taken up by women.
During COVID lockdowns, knitting saw another resurgence. But knitting still most often makes headlines when men – especially famous men like Daley or actor Ryan Gosling – do it.
Men who knit are often seen as subverting the stereotype it’s an activity for older women.
Knitting the stress away
Knitting can produce a sense of pride and accomplishment. But for an elite sportsperson like Daley – whose accomplishments already include four gold medals and one silver – its benefits lie elsewhere.
Olympics-level sport relies on perfect scores and world records. When it comes to knitting, many of the mental health benefits are associated with the process, rather than the end result.
Daley says knitting is the “one thing” that allows him to switch off completely, describing it as “my therapy”. https://www.youtube.com/embed/6wwXGOki–c?wmode=transparent&start=0
The Olympian says he could
knit for hours on end, honestly. There’s something that’s so satisfying to me about just having that rhythm and that little “click-clack” of the knitting needles. There is not a day that goes by where I don’t knit.
Knitting can create a “flow” state through rhythmic, repetitive movements of the yarn and needle. Flow offers us a balance between challenge, accessibility and a sense of control.
It’s been shown to have benefits relieving stress in high-pressure jobs beyond elite sport. Among surgeons, knitting has been found to improve wellbeing as well as manual dexterity, crucial to their role.
For other health professionals – including oncology nurses and mental health workers – knitting has helped to reduce “compassion fatigue” and burnout. Participants described the soothing noise of their knitting needles. They developed and strengthened team bonds through collective knitting practices. https://www.youtube.com/embed/dTTJjD_q2Ik?wmode=transparent&start=0 A Swiss psychiatrist says for those with trauma, knitting yarn can be like “knitting the two halves” of the brain “back together”.
Another study showed knitting in primary school may boost children’s executive function. That includes the ability to pay attention, remember relevant details and block out distractions.
As a regular creative practice, it has also been used in the treatment of grief, depression and subduing intrusive thoughts, as well countering chronic pain and cognitive decline.
Knitting is a community
The evidence for the benefits of knitting is often based on self-reporting. These studies tend to produce consistent results and involve large population samples.
This may point to another benefit of knitting: its social aspect.
Knitting and other yarn crafts can be done alone, and usually require simple materials. But they also provide a chance to socialise by bringing people together around a common interest, which can help reduce loneliness.
The free needle craft database and social network Ravelry contains more than one million patterns, contributed by users. “Yarn bombing” projects aim to engage the community and beautify public places by covering objects such as benches and stop signs with wool.
The interest in Daley’s knitting online videos have formed a community of their own.
In them he shows the process of making the jumper, not just the finished product. That includes where he “went wrong” and had to unwind his work.
His pride in the finished product – a little bit wonky, but “made with love” – can be a refreshing antidote to the flawless achievements often on display at the Olympics.
Michelle O’Shea, Senior Lecturer, School of Business, Western Sydney University and Gabrielle Weidemann, Associate Professor in Psychological Science, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Here’s Looking At Ya!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Main Feature Should Take You Two Minutes (and 18 Seconds) To Read*
*Or at least, that’s what we’re told by this software that checks things for readability!
There’s a problem nobody wants to talk about when it comes to speed-reading
If you’re not very conscientious in your method, information does get lost. Especially, anything over 500 words per minute is almost certainly skimming and not true speed-reading.
One of the reasons information gets lost is because of a weird and wonderful feature of our eyes and brain: saccades.
Basically, our eyes can either collect visual information or they can move; they can’t do both at once. And as you may know, our eyes are almost always moving. So why aren’t we blind most of the time?
We actually are.
Did you know: your eyes take two upside-down 2D images and your brain presents you one 3D image the right way around instead? You probably did know that. So: it’s a bit like that.
Your brain takes a series of snapshots from whenever your eyes weren’t moving, and mentally fills in the blanks for you, just like a studio animation. We have a “frame rate” of about 60 frames per second, by the way—that’s why many computer monitors use that frequency. Lower frequencies can result in a noticeable flicker, and higher frequencies are wasted on us mere mortals!
Our eyes do some super-speedy movements called saccades (up to 500º per second! Happily no, our eyes don’t rotate 500º, but that’s the “per second” rate) and our brain fills in the gaps with its best guesses. The more you push it, the more it’ll guess wrong.
We’re not making this up, by the way! See for yourself:
Eye Movements In Reading And Information Processing: 20 Years Of Research
Fortunately, it is possible to use your eyes in a way that reduces the brain’s need to guess. That also means it has more processing power left over to guess correctly when it does need to.
Yes, There’s An App For That
Actually there are a few! But we’re going to recommend Spreeder as a top-tier option, with very rapid improvement right from day one.
It works by presenting the text with a single unmoving focal point. This is the opposite of traditional speed-reading methods that involve a rapidly moving pacer (such as your finger on the page, or a dot on the screen).
This unmoving focal point (while the words move instead) greatly reduces the number of saccades needed, and so a lot less information is lost to optical illusions and guesswork.
Try Spreeder (any platform) Here Now!
If you find that easy to use and would like something with a few more features, you might like another app that works on the same principle: Spritz.
It can take a bit more getting-used-to, but allows for greater integrations with all your favourite content in the long-run:
Check Out Spritz: Android App / iOS App / Free Chrome Extension
Lastly, if you don’t want any of those fancy apps and would just like to read more quickly and easily with less eye-strain, Beeline has you covered.
For free, unless you want to unlock some premium features!
How Beeline works is by adding a color gradient to text on websites and in documents. This makes it a lot easier for the eye to track without going off-piste, skipping a line, or re-reading the same bit again, etc.
Share This Post
-
Calm Your Mind with Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From the author of This Is Your Brain On Food, the psychiatrist-chef (literally, she is a Harvard-trained psychiatrist and an award-winning chef) is back with a more specific work, this time aimed squarely at what it says in the title; how to calm your mind with food.
You may be wondering: does this mean comfort-eating? And, well, not in the sense that term’s usually used. There will be eating and comfort will occur, but the process involves an abundance of nutrients, a minimization of health-deleterious ingredients, and a “for every chemical its task” approach. In other words, very much “nutraceuticals”, as our diet.
On which note: as we’ve come to expect from Dr. Naidoo, we see a lot of hard science presented simply and clearly, with neither undue sensationalization nor unnecessary jargon. We learn about the brain, the gut, relevant biology and chemistry, and build up from understanding ingredients to dietary patterns to having a whole meal plan, complete with recipes.
You may further be wondering: how much does it add that we couldn’t get from the previous book? And the answer is, not necessarily a huge amount, especially if you’re fairly comfortable taking ideas and creating your own path forwards using them. If, on the other hand, you’re a little anxious about doing that (as someone perusing this book may well be), then Dr. Naidoo will cheerfully lead you by the hand through what you need to know and do.
Bottom line: if not being compared to her previous book, this is a great standalone book with a lot of very valuable content. However, the previous book is a tough act to follow! So… All in all we’d recommend this more to people who want to indeed “calm your mind with food”, who haven’t read the other book, as this one will be more specialized for you.
Click here to check out Calm Your Mind With Food, and do just that!
Share This Post
-
Intermittent Fasting, Intermittently?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Have you come across any research on alternate-day intermittent fasting—specifically switching between one day of 16:8 fasting and the next day of regular eating patterns? I’m curious if there are any benefits or drawbacks to this alternating approach, or if the benefits mainly come from consistent intermittent fasting?❞
Short and unhelpful answer: no
Longer and hopefully more helpful answer:
As you probably know, usually people going for approaches based on the above terms either
- practise 16:8 fasting (fast for 16 hours each day, eat during an 8-hour window) or
- practise alternate-day fasting (fast for 24 hours, eat whenever for 24 hours, repeat)
…which latter scored the best results in this large meta-analysis of studies:
There is also the (popular) less extreme version of alternate-day fasting, sometimes called “eat stop eat”, which is not a very helpful description because that describes almost any kind of eating/fasting, but it usually refers to “once per week, take a day off from eating”.
You can read more about each of these (and some other variants), here:
Intermittent Fasting: What’s The Truth?
What you are describing (doing 16:8 fasting on alternate days, eating whenever on the other days) is essentially: intermittent fasting, just with one 16-hour fast per 48 hours instead of per the usual 24 hours.
See also: International consensus on fasting terminology ← the section on the terms “STF & PF” covers why this gets nudged back under the regular IF umbrella
Good news: this means there is a lot of literature into the acute (i.e., occurring the same day, not long-term)* benefits of 16:8 IF, and that means that you will be getting those benefits, every second day.
You remember that meta-analysis we posted above? While it isn’t mentioned in the conclusion (which only praised complete alternate-day fasting producing the best outcomes overall), sifting through the results data discovers that time-restricted eating (which is what you are doing, by these classifications) was the only fasting method to significantly reduce fasting blood glucose levels.
(However, no significant differences were observed between any IF form and the reference (continuous energy restriction, CER, i.e. calorie-controlled) diets in fasting insulin and HbA1c levels)
*This is still good news in the long-term though, because getting those benefits every second day is better than getting those benefits on no days, and this will have a long-term impact on your healthy longevity, just like how it is better to exercise every second day than it is to exercise no days, or better to abstain from alcohol every second day than it is to abstain on no days, etc.
In short, by doing IF every second day, you are still giving your organs a break sometimes, and that’s good.
All the same, if it would be convenient and practical for you, we would encourage you to consider either the complete alternate-day fasting (which, according to a lot of data, gives the best results overall),or time-restricted eating (TRE) every day (which, according to a lot of data, gives the best fasting blood sugar levels).
You could also improve the TRE days by shifting to 20:4 (i.e., 20 hours fasting and 4 hours eating), this giving your organs a longer break on those days.
Want to learn more?
For a much more comprehensive discussion of the strengths and weaknesses of different approaches to intermitted fasting, check out:
Enjoy!
Share This Post
Related Posts
-
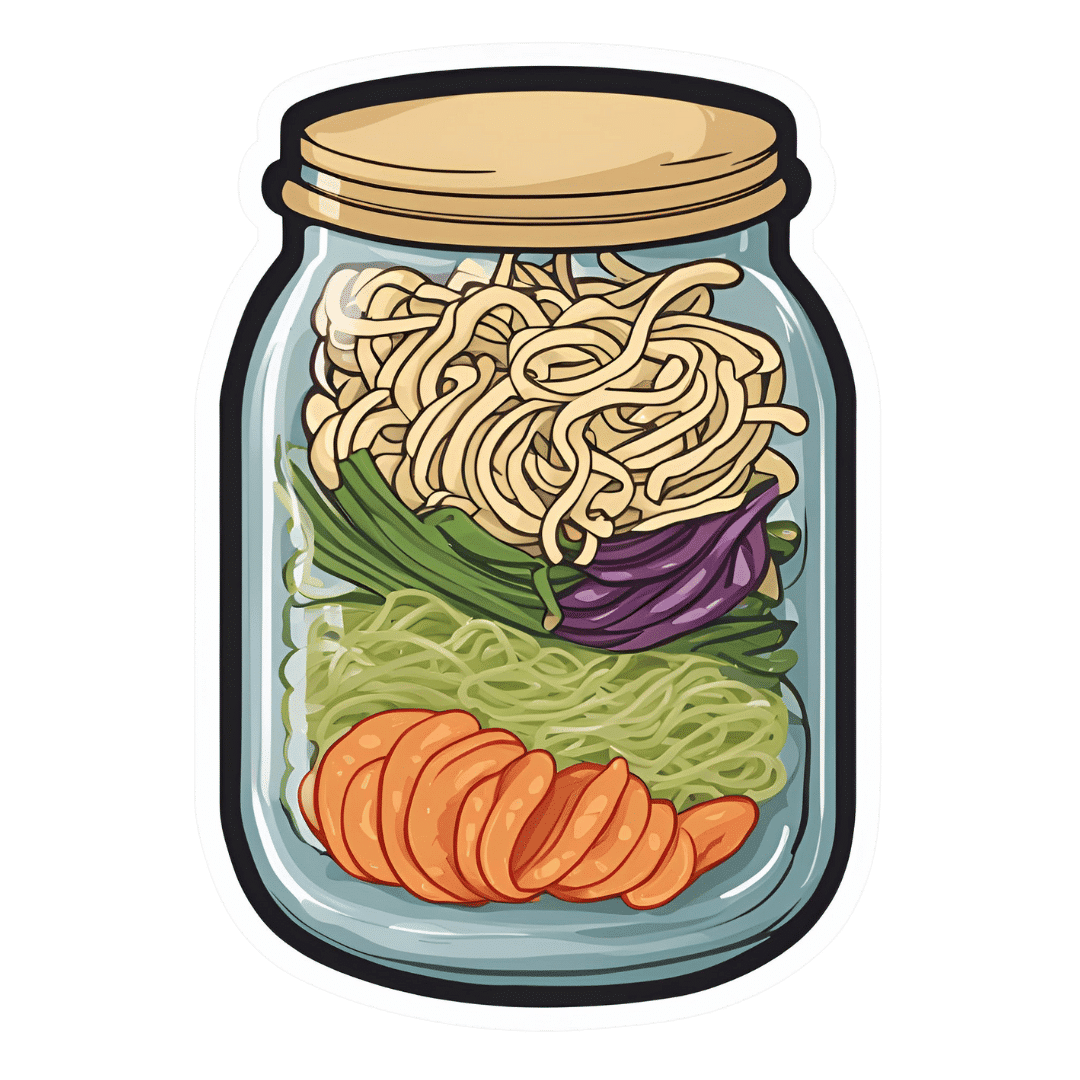
Gut-Positive Pot Noodles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Everything we consume either improves our health a little or worsens it. Pot noodles aren’t generally the healthiest foods, but these ones sure are! There’s quite a range of fiber in this, including the soluble fiber of the noodles themselves (which are, in fact, mostly fiber and water). As a bonus, the glucomannan in the noodles promotes feelings of fullness, notwithstanding its negligible carb count. Of course, the protein in the edamame beans also counts for satiety!
You will need
- ½ cup konjac noodles (also called shirataki), tossed in 1 tsp avocado oil (or sesame oil, if you don’t have avocado)
- 2 oz mangetout, thinly sliced
- 1 oz edamame beans
- ¼ carrot, grated
- 2 baby sweetcorn, cut in half lengthways
- 1 scallion, finely diced
- 1 heaped tsp crunchy peanut butter (omit if allergic)
- 1 tsp miso paste
- 1 tsp chili oil
- 1 tsp black pepper, coarse ground
- 1 tsp peeled-and-grated ginger
Method
(we suggest you read everything at least once before doing anything)
1) Layer a heat-resistant jar (mason jars are usually quite resistant to temperature changes) with the noodles and vegetables.
2) Combine the peanut butter, miso paste, and chili oil, black pepper, and ginger in a small bowl. Pour this dressing over the layered vegetables and noodles, and screw the lid on. Refrigerate until needed.
3) Add hot water to the jar and stir, to serve. If you prefer the vegetables to be more cooked, you can microwave (without the lid!) for a minute or two.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- 10 Ways To Balance Blood Sugars ← today’s recipe makes a perfect high-fiber, low-carb starter, per the hacks here
- Capsaicin For Weight Loss And Against Inflammation
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Ginger Does A Lot More Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are You Flourishing? (There’s a Scale)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What does it mean, to flourish? And how can you do it more?
In 2009, psychologists Diener et al developed the “Flourishing Scale”, or as it was more prosaically called originally, “Subjective Wellness Scale”. The name was changed later, as it was noted that it went beyond what was typically considered mere “wellness”.
This scale was so useful, that colleagues scrambled to see if they could improve on it, such as with PERMA (2012), which looked at:
- Positive emotion
- Engagement
- positive Relationships
- Meaning
- Accomplishment/Achievement
While popular (despite the tenuous acronym, it is a very good list of things to foster in your life), this was studied and measured scientifically and found to not be an improvement on the Flourishing Scale / SWS, so we’re going to stick to the original version for now.
We couldn’t find an interactive online quiz for the scale though (apart from this NY Times one, which is paywalled for NYT subscribers, so enjoy if you’re a NYT subscriber!), so here’s the source material, still hosted on the website of the (now deceased, as of a couple of years ago) author:
Flourishing Scale (FS) ← it’s an eight-question, ranked choice scale
How did you score? And…
What are the keys to flourishing more?
According to Jeffrey Davis M.A., of Tracking Wonder, there are five key attributes that we must develop and/or maintain:
The ability to direct and re-direct your attention
This isn’t just a task-related thing.This is about your mind itself. For example, the ability to recognize what your emotions are telling you, thank them for the message, and then set them aside. Or the ability to cut through negative thought spirals! How often have you worried about future events that didn’t transpire, or twisted yourself in knots over a past event that you can’t change?
Action: check out our previous article “The Off-Button For Your Brain” ← this is a technique for switching off racing thoughts, and it’s really good
Want more? We also did this:
The tendency to shape your time with intention and for impact
Time is an incredibly precious asset. How you use it is a very personal choice. You don’t have to maximize productivity (though you can if you want), but for example there’s a difference between:
- Deciding to spend an hour watching a TV show you really enjoy
- Wondering what’s on TV, browsing aimlessly, watching listlessly, just a distraction
In the former case, you are enjoying your time. Literally: you are experiencing joy during your time.
In the latter case, to borrow from Jim Steinman, “you were only killing time and it’ll kill you right back”!
Action: do a time audit for a week, and see where your time really goes, rather than where you expect or hope for it to go. Use this information to plan your next week more intentionally. Repeat as and when it seems like it might be useful!
The practice of constant improvement
Fun fact: you are good enough already. And you can also improve. You don’t have to, but improving in the areas that are meaningful to you can really add up over time. This could be becoming excellent at something for which already have a passion… It could also be brushing up something that you feel might be holding you back.
Action: do a quick SWOT* self-assessment. Then plan your next step from there!
*Strengths, Weaknesses, Opportunities, Threats. What are yours?
The ability to communicate and listen to others
A lot of this is about feedback. Giving and receiving feedback are often amongst the hardest things we do in the category of communication… Especially if the feedback is negative. How to decide what to disregard as baseless criticism, and what to take on board (and try not to take it personally), or the other way around, how to present negative feedback in a way that won’t trigger defensiveness.
Action: check out our previous article “Save Time With Better Communication” for some tips that really make relationships (of any kind) so much easier.
The commitment to positive experiences
Many things in life are not fun. Often, we know in advance that they will not be fun. The key here is the ability to make the most of a bad situation, and seek out better situations by your actions. Not like a lost person in a desert seeks water, but like a chess player who employs a general strategy to make tactical advantages more likely to appear.
Action: think about something you have to do but don’t want to. How could it be made more fun? Or failing that, how could it be made at least more comfortable?
See also: Working Smarter < Working Brighter!
Want to read more?
Check out: What Is Flourishing in Positive Psychology? (+8 Tips & PDF)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
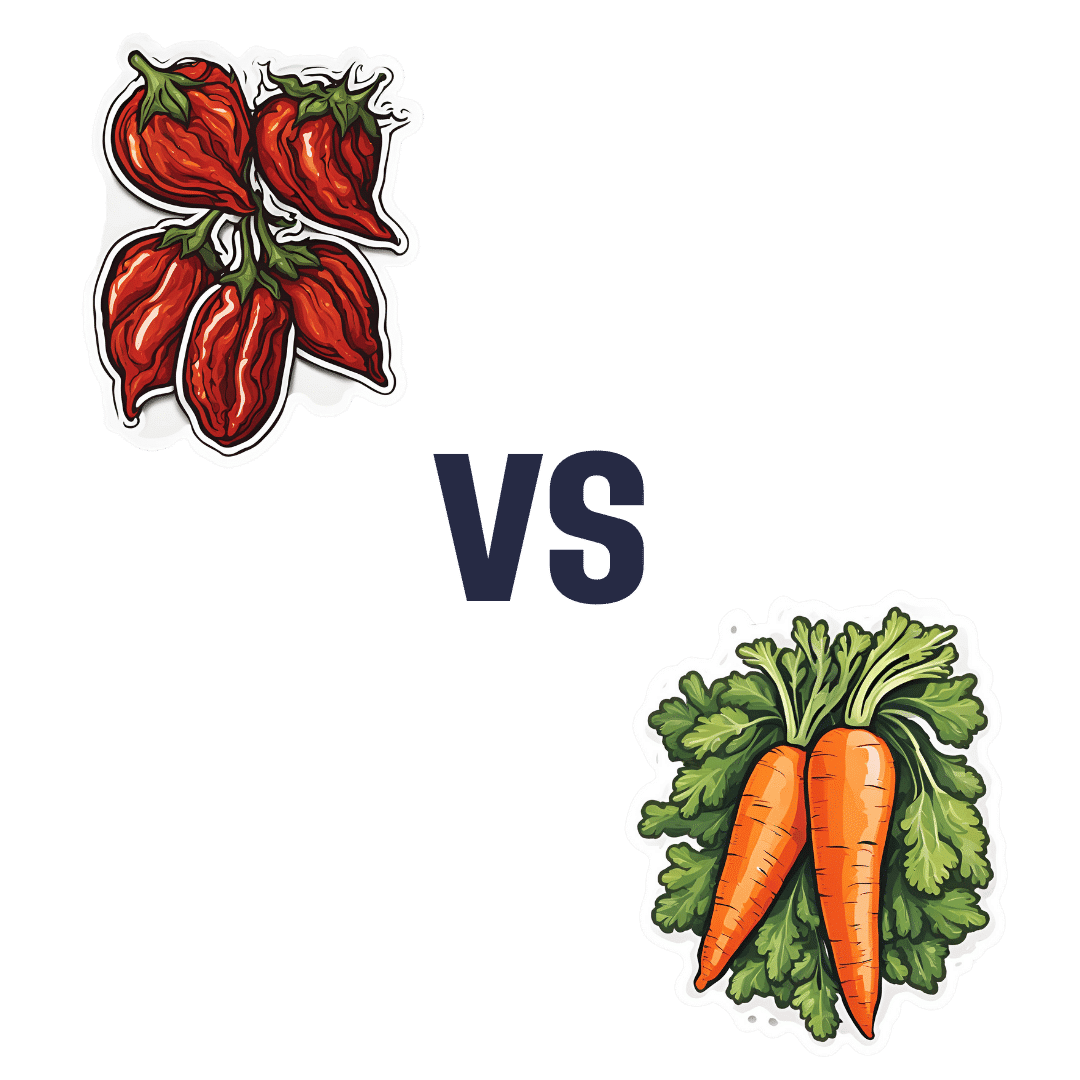
Sun-Dried Tomatoes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sun-dried tomatoes to carrots, we picked the sun-dried tomatoes.
Why?
After tomatoes lost to carrots yesterday, it turns out that sun-drying them is enough to turn the nutritional tables!
This time, it’s the sun-dried tomatoes that have more carbs and fiber, as well as the nominally lower glycemic index (although obviously, carrots are also just fine in this regard; nobody is getting metabolic disease from eating carrots). Still, by the numbers, a win for sun-dried tomatoes.
In terms of vitamins, the fact that they have less water-weight means that proportionally, gram for gram, sun-dried tomatoes have more of vitamins B1, B2, B3, B5, B6, B9, C, E, K, and choline, while carrots still have more vitamin A. An easy win for sun-dried tomatoes on the whole, though.
When it comes to minerals, sun-dried tomatoes have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while carrots are not higher in any mineral.
Looking at polyphenols, sun-dried tomatoes have more, including a good healthy dose of quercetin; they also have more lycopene, not technically a polyphenol by virtue of its chemical structure (it’s a carotenoid), but a powerful phytochemical nonetheless. And, the lycopene content is higher in sun-dried tomatoes (compared to raw tomatoes) not just because of the loss of water-weight making a proportional difference, but also because the process itself improves the lycopene content, much like cooking does.
All in all, a clear and overwhelming win for sun-dried tomatoes.
Just watch out, as this is about the sun-dried tomatoes themselves; if you get them packed in vegetable oil, as is common, it’ll be a very different nutritional profile!
Want to learn more?
You might like to read:
Tomatoes vs Carrots – Which is Healthier? ← see the difference!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: