Is there anything good about menopause? Yep, here are 4 things to look forward to
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause is having a bit of a moment, with less stigma and more awareness about the changes it can bring.
A recent senate inquiry recommended public education about perimenopause and menopause, more affordable treatments and flexible work arrangements.
But like many things in life the experiences of menopause are on a continuum. While some women find it challenging and require support, others experience some physical and emotional benefits. These are rarely reported – but we can learn from the research available and, importantly, from people’s lived experiences.
Here are four changes to look forward to once you reach menopause.

1. No more periods or related issues
Menopause is considered “complete” 12 months after the final period of a woman (or person assigned female at birth) who previously menstruated.
Perhaps unsurprisingly, the benefit at the top of the list is no more periods (unless you are taking hormone therapy and still have your womb). This can be particularly beneficial for women who have had to manage erratic, unpredictable and heavy bleeding.
At last, you don’t need to keep sanitary protection in every bag “just in case”. No more planning where the bathroom is or having to take extra clothes. And you’ll save money by not purchasing sanitary products.
There is also good news for women who have had heavy bleeding due to uterine fibroids – common benign gynaecological tumours that affect up to 80% of women. The evidence suggests hormonal changes (for women not taking hormone therapy) can lead to a reduction in the size of fibroids and relieve symptoms.
Women who suffer from menstrual migraine may experience an improvement in migraines post-menopause as their hormonal fluctuations begin to settle – but the timeframe for this remains unclear.
For some women, no more periods also means more participation in social activities from which they may have been excluded due to periods. For example, religious activities or food preparation in some cultures.
2. Getting your body and your groove back
Throughout their reproductive lives, women in heterosexual relationships are usually the ones expected to be proactive about preventing pregnancy.
Some post-menopausal women describe a re-emergence of their sexuality and a sense of sexual freedom that they had not previously experienced (despite contraceptive availability) as there is no longer a risk of pregnancy.
A participant in my research into women’s experiences of menopause described the joy of no longer being child-bearing age:
I’ve got a body back for me, you know, coz I can’t get pregnant, not that I haven’t enjoyed having [children] and things like that and it was a decision to get pregnant but I feel like, ooh my body isn’t for anybody now but me, people, you know?
For women who have chosen to be child-free there may also be a sense of freedom from social expectations. People will likely stop asking them when they are planning to have children.
3. A new chapter and a time to focus on yourself
Another participant described menopause as an unexpected “acceleration point” for change.
Women told us they were more accepting of themselves and their needs rather than being focused on the needs of other people. Researchers have previously tracked this shift from “living for others” to “a life of one’s own”.
Some women find the strength of emotions at this time a challenge, whereas others find their potency can facilitate liberation – enabling them to speak their minds or be more assertive than at any other time in their lives.
4. Increased self-confidence
A new sense of liberation can fuel increased self-confidence at menopause. This has been reported in studies based on in-depth interviews with women.
Confidence boosts can coincide with changes in career and sometimes in relationships as priorities and self-advocacy transform.
Life on the other side
It can be hard to think about what is good about menopause, particularly if you are having challenges during perimenopause – but these can get better with time.
In cultures where women are valued as they become older, women describe themselves as positively contributing to the community. They find they gain power and respect as they age.
We need to work towards more positive societal attitudes on this front. Our bodies change across the lifespan and are remarkable at every stage, including menopause.
Yvonne Middlewick, Nurse, Lecturer & Director of Post-graduate Studies in the School of Nursing and Midwifery, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Meditations for Mortals – by Oliver Burkeman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this author’s “Four Thousand Weeks”, but for those who might have used a lot of those four thousand weeks already, and would like to consider things within a smaller timeframe for now, this work is a 28-day daily reader.
Now, daily readers are usually 366 days, but the chapters here are not the single page chapters that 366-page daily readers usually have. So, expect to invest a little more time per day (say, about 6 pages for each daily chapter).
Burkeman does not start the way we might expect, by telling us to take the time to smell the roses. Instead, he starts by examining the mistakes that most of us make most of the time, often due to unexamined assumptions about the world and how it works. Simply put, we’ve often received bad lessons in life (usually not explicitly, but rather, from our environments), and it takes some unpacking first to deal with that.
Nor is the book systems-based, as many books that get filed under “time management” may be, but rather, is simply principles-based. This is a strength, because principles are a lot easier to keep to than systems.
The writing style is direct and conversational, and neither overly familiar nor overly academic. It strikes a very comfortably readable balance.
Bottom line: if you’d like to get the most out of your days, this book can definitely help improve things a lot.
Click here to check out Meditations For Mortals, and live fulfilling days!
Share This Post
-
How To Boost Your Memory Immediately (Without Supplements)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Boost Your Memory (Without Supplements)
While we do recommend having a good diet and taking advantage of various supplements that have been found to help memory, that only gets so much mileage. With that in mind…
First, how good is your memory? Take This 2-Minute Online Test
Now, that was a test of short term memory, which tends to be the most impactful in our everyday life.
It’s the difference between “I remember the address of the house where I grew up” (long-term memory) and “what did I come to this room to do?” (short-term memory / working memory)
First tip:
When you want to remember something, take a moment to notice the details. You can’t have a madeleine moment years later if you wolfed down the madeleines so urgently they barely touched the sides.
This goes for more than just food, of course. And when facing the prospect of age-related memory loss in particular, people tend to be afraid not of forgetting their PIN code, but their cherished memories of loved ones. So… Cherish them, now! You’ll struggle to cherish them later if you don’t cherish them now. Notice the little details as though you were a painter looking at a scene for painting. Involve more senses than just sight, too!
If it’s important, relive it. Relive it now, relive it tomorrow. Rehearsal is important to memory, and each time you relive a memory, the deeper it gets written into your long-term memory until it becomes indelible to all but literal brain damage.
Second tip:
Tell the story of it to someone else. Or imagine telling it to someone else! (You brain can’t tell the difference)
And you know how it goes… Once you’ve told a story a few times, you’ll never forget it later. Isn’t your life a story worth telling?
Many people approach memory like they’re studying for a test. Don’t. Approach it like you’re preparing to tell a story, or give a performance. We are storytelling creatures at heart, whether or not we realize it.
What do you do when you find yourself in a room and wonder why you went there? (We’ve all been there!) You might look around for clues, but if that doesn’t immediately serve, your fallback will be retracing your steps. Literally, physically, if needs be, but at least mentally. The story of how you got there is easier to remember than the smallest bit of pure information.
What about when there’s no real story to tell, but we still need to remember something?
Make up a story. Did you ever play the game “My granny went to market” as a child?
If not, it’s a collaborative memory game in which players take turns adding items to a list, “My granny went to market and bought eggs”, My granny went to market and bought eggs and milk”, “my granny went to market and bought eggs and milk and flour” (is she making a cake?), “my granny went to market and bought eggs and milk and flour and shoe polish” (what image came to mind? Use that) “my granny went to market and bought eggs and milk and flour and shoe polish and tea” (continue building the story in your head), and so on.
When we actually go shopping, if we don’t have a written list we may rely on the simple story of “what I’m going to cook for dinner” and walking ourselves through that story to ensure we get the things we need.
This is because our memory thrives (and depends!) on connections. Literal synapse connections in the brain, and conceptual contextual connections in your mind. The more connections, the better the memory.
Now imagine a story: “I went to Stonehenge, but in the background was a twin-peaked mountain blue. I packed a red suitcase, placing a conch shell inside it, when suddenly I heard a trombone, and…” Ring any bells? These are example items from the memory test earlier, though of course you may have seen different things in a different order.
So next time you want to remember things, don’t study as though for a test. Prepare to tell a story!
Try going through the test again, but this time, ignore their instructions because we’re going to use the test differently than intended (we’re rebels like that). Don’t rush, and don’t worry about the score this time (or even whether or not you saw a given image previously), but instead, build a story as you go. We’re willing to bet that after it, you can probably recite most of the images you saw in their correct order with fair confidence.
Here’s the link again: Take The Same Test, But This Time Make It Story-Worthy!
Again, ignore what it says about your score this time, because we weren’t doing that this time around. Instead, list the things you saw.
What you were just able to list was the result of you doing story-telling with random zero-context images while under time pressure.
Imagine what you can do with actual meaningful memories of your ongoing life, people you meet, conversations you have!
Just… Take the time to smell the roses, then rehearse the story you’ll tell about them. That memory will swiftly become as strong as any memory can be, and quickly get worked into your long-term memory for the rest of your days.
Share This Post
-
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Share This Post
Related Posts
-
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Bone density is a concern for a lot of people past a certain age, and it can lead to an endless juggling of vitamin and mineral supplements to try to get the right balance. Sachiaki Takamiya advocates for a natural diet- and exercise-based approach instead, showing good results with his Okinawan-influenced Blue Zones diet and lifestyle.
As a caveat, he has not gone through menopause, so this video does completely overlook the implications of that. Nevertheless, even if some of us must get our hormones from a bottle these days, this diet and exercise approach is a very good foundation and the advice here is important for all—we can take all the estrogen we need and still have weak bones if our diet and exercise aren’t there as needed.
From strength to strength
Sachiaki Takamiya’s bone density wasn’t bad the previous year, but this year it is better, hitting 123.4%. This is important information, because it’s easier to achieve an n% increase (for any given value of n) if your starting point is lower. For example, a 50% increase from 1g is 1.5g (so, 0.5g difference), whereas a 50% increase from 20g is 30g (so, a 10g difference). Since his starting value was high, this makes his 21% rise particularly noteworthy—and mean that a reader with a lower starting value will most likely see even better gains, if implementing this protocol.
You may be wondering: isn’t a bone mass density of 123.4% about 23.4% more than we want it? And the answer is that the 100% value is taken from an average peak bone mass in young adults, so having it at 100% is fine, and having it a bit higher is still better—it just means he’s outclassing healthy young adults, less likely to break a bone if he falls, etc.
As for what he ate: he focused on getting calcium and magnesium, as well as vitamins D and K2, all from food sources. Key foods included small fish (sardines, niosi, jaco), nattō, mushrooms, and seaweed (nori, wakame, hijiki). In particular, he emphasizes nattō’s benefits for bones, as well as for the gut, heart, and brain.
As for his exercise: he did weight-bearing exercise and resistance training—including calisthenics and yoga, as well as sport, and simply walking and running. His weekly routine looked like this:
- Monday: heart rate zone 2 jogging (45 min)
- Tuesday: bodyweight HIIT and flexibility (20 min)
- Wednesday: heart rate zone 2 jogging (60 min)
- Thursday: bodyweight HIIT and flexibility (40 min)
- Friday: heart rate zone 2 jogging (45 min)
- Saturday: bodyweight HIIT and flexibility (20 min)
…as well as social sports (e.g. tennis, amongst others), and additional activities such as gardening, and cycling for groceries.
For more on all of the above (this is a very information-dense video), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Vit D + Calcium: Too Much Of A Good Thing?
- The Bare-Bones Truth About Osteoporosis
- Which Osteoporosis Medication, If Any, Is Right For You?
- How To Do HIIT (Without Wrecking Your Body)
- The Five Pillars Of Blue Zone Longevity
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to be kind to yourself (without going to a day spa)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I have to be hard on myself,” Sarah told me in a recent telehealth psychology session. “I would never reach my potential if I was kind and let myself off the hook.”
I could empathise with this fear of self-compassion from clients such as Sarah (not her real name). From a young age, we are taught to be kind to others, but self-kindness is never mentioned.
Instead, we are taught success hinges on self-sacrifice. And we need a healthy inner critic to bully us forward into becoming increasingly better versions of ourselves.
But research shows there doesn’t have to be a trade-off between self-compassion and success.
Self-compassion can help you reach your potential, while supporting you to face the inevitable stumbles and setbacks along the way.
What is self-compassion?
Self-compassion has three key ingredients.
1. Self-kindness
This involves treating yourself with the same kindness you would extend towards a good friend – via your thoughts, feelings and actions – especially during life’s difficult moments.
For instance, if you find yourself fixating on a minor mistake you made at work, self-kindness might involve taking a ten-minute walk to shift focus, and reminding yourself it is OK to make mistakes sometimes, before moving on with your day.
2. Mindfulness
In this context, mindfulness involves being aware of your own experience of stress or suffering, rather than repressing or avoiding your feelings, or over-identifying with them.
Basically, you must see your stress with a clear (mindful) perspective before you can respond with kindness. If we avoid or are consumed by our suffering, we lose perspective.
3. Common humanity
Common humanity involves recognising our own experience of suffering as something that unites us as being human.
For instance, a sleep-deprived parent waking up (for the fourth time) to feed their newborn might choose to think about all the other parents around the world doing exactly the same thing – as opposed to feeling isolated and alone.
It’s not about day spas, or booking a manicure
When Sarah voiced her fear that self-compassion would prevent her success, I explained self-compassion is distinct from self-indulgence.
“So is self-compassion just about booking in more mani/pedis?” Sarah asked.
Not really, I explained. A one-off trip to a day spa is unlikely to transform your mental health.
Instead, self-compassion is a flexible psychological resilience factor that shapes our thoughts, feelings and actions.
It’s associated with a suite of benefits to our wellbeing, relationships and health.
A one-off trip to a day spa is unlikely to transform your mental health.
baranq/ShutterstockWhat does the science say?
Over the past 20 years, we’ve learned self-compassionate people enjoy a wide range of benefits. They tend to be happier and have fewer psychological symptoms of distress.
Those high on self-compassion persevere following a failure. They say they are more motivated to overcome a personal weakness than those low on self-compassion, who are more likely to give up.
So rather than feeling trapped by your inadequacies, self-compassion encourages a growth mindset, helping you reach your potential.
However, self-compassion is not a panacea. It will not change your life circumstances or somehow make life “easy”. It is based on the premise that life is hard, and provides practical tools to cope.
It’s a factor in healthy ageing
I research menopause and healthy ageing and am especially interested in the value of self-compassion through menopause and in the second half of life.
Because self-compassion becomes important during life’s challenges, it can help people navigate physical symptoms (for instance, menopausal hot flushes), life transitions such as divorce, and promote healthy ageing.
I’ve also teamed up with researchers at Autism Spectrum Australia to explore self-compassion in autistic adults.
We found autistic adults report significantly lower levels of self-compassion than neurotypical adults. So we developed an online self-compassion training program for this at-risk population.
Three tips for self-compassion
You can learn self-compassion with these three exercises.
1. What would you say to a friend?
Think back to the last time you made a mistake. What did you say to yourself?
If you notice you’re treating yourself more like an enemy than a friend, don’t beat yourself up about it. Instead, try to think about what you might tell a friend, and direct that same friendly language towards yourself.
2. Harness the power of touch
Soothing human touch activates the parasympathetic “relaxation” branch of our nervous system and counteracts the fight or flight response.
Specifically, self-soothing touch (for instance, by placing both hands on your heart, stroking your forearm or giving yourself a hug) reduces cortisol responses to psychosocial stress.
Yes, hugging yourself can help.
http://krakenimages.com/Shutterstock3. What do I need right now?
Sometimes, it can be hard to figure out exactly what self-compassion looks like in a given moment. The question “what do I need right now” helps clarify your true needs.
For example, when I was 37 weeks pregnant, I woke up bolt awake one morning at 3am.
Rather than beating myself up about it, or fretting about not getting enough sleep, I gently placed my hands on my heart and took a few deep breaths. By asking myself “what do I need right now?” it became clear that listening to a gentle podcast/meditation fitted the bill (even though I wanted to addictively scroll my phone).
Lydia Brown, Senior Lecturer in Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kidney Beans or Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
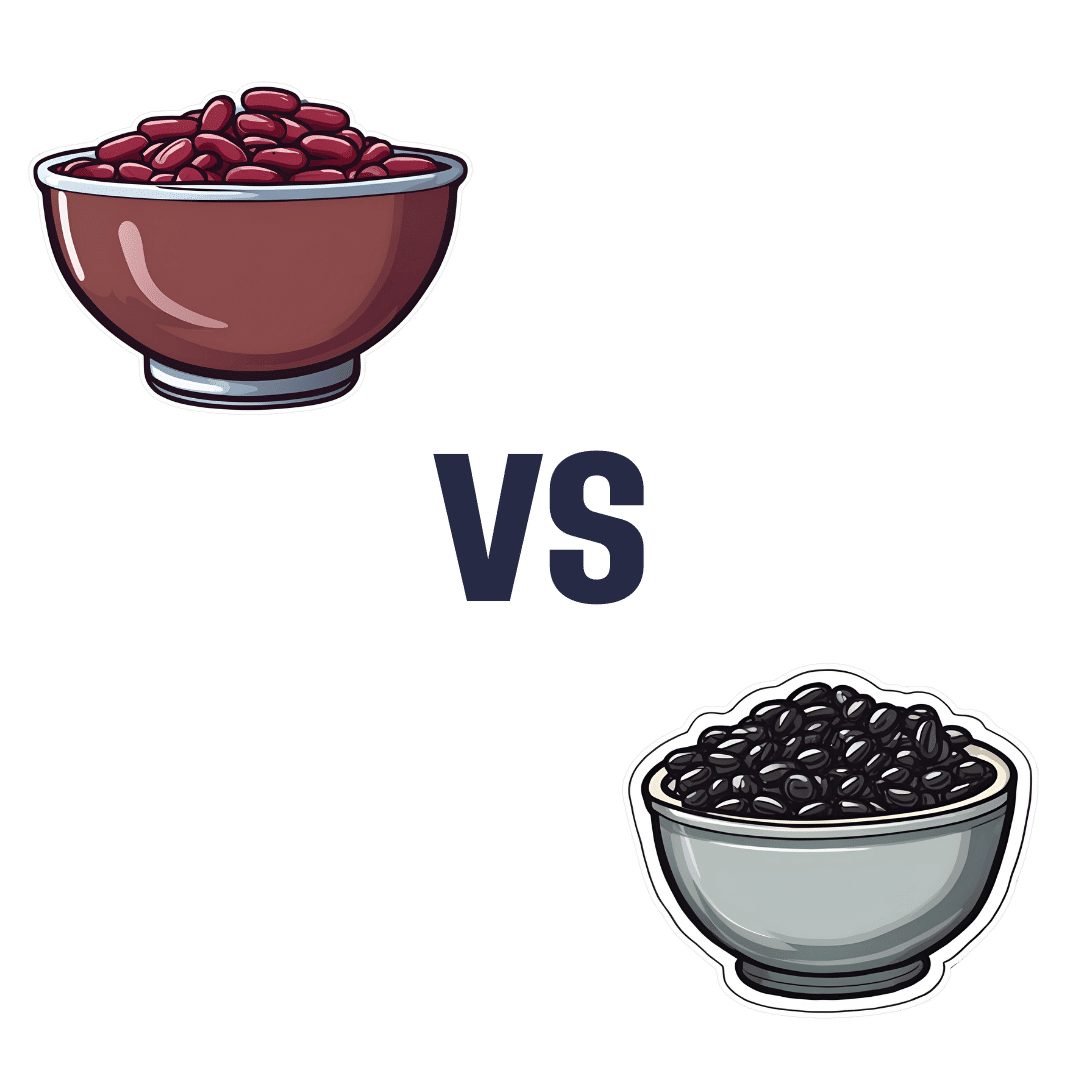
When comparing kidney beans to black beans, we picked the black beans.
Why?
First, do note that black beans are also known as turtle beans, or if one wants to hedge one’s bets, black turtle beans. It’s all the same bean. As a small linguistic note, kidney beans are known as “red beans” in many languages, so we could have called this “red beans vs black beans”, but that wouldn’t have landed so well with our largely anglophone readership. So, kidney beans vs black beans it is!
They’re certainly both great, and this is a close one today…
In terms of macros, they’re equal on protein and black beans have more carbs and/but also more fiber. So far, so equal—or rather, if one pulls ahead of the other here, it’s a matter of subjective priorities.
In the category of vitamins, they’re equal on vitamins B2, B3, and choline, while kidney beans have more of vitamins B6, B9, C, and K, and black beans have more of vitamins A, B1, B5, and E. In other words, the two beans are still tied with a 4:4 split, unless we want to take into account that that vitamin E difference is that black beans have 29x more vitamin E, in which case, black beans move ahead.
When it comes to minerals, finally the winner becomes apparent; while kidney beans have a little more manganese and zinc, on the other hand black beans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium. However, it should be noted that honestly, the margins aren’t huge here and kidney beans are almost as good for all of these minerals.
In short, black beans win the day, but kidney beans are very close behind, so enjoy whichever you prefer, or better yet, both! They go great together in tacos, burritos, or similar, by the way.
Want to learn more?
You might like to read:
- Kidney Beans vs Fava Beans – Which is Healthier?
- Chickpeas vs Black Beans – Which is Healthier?
- Bold Beans – by Amelia Christie-Miller ← this is a recipe book; if you’re looking to incorporate more beans into your diet and want to make it good, this cookbook can lead the way!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: