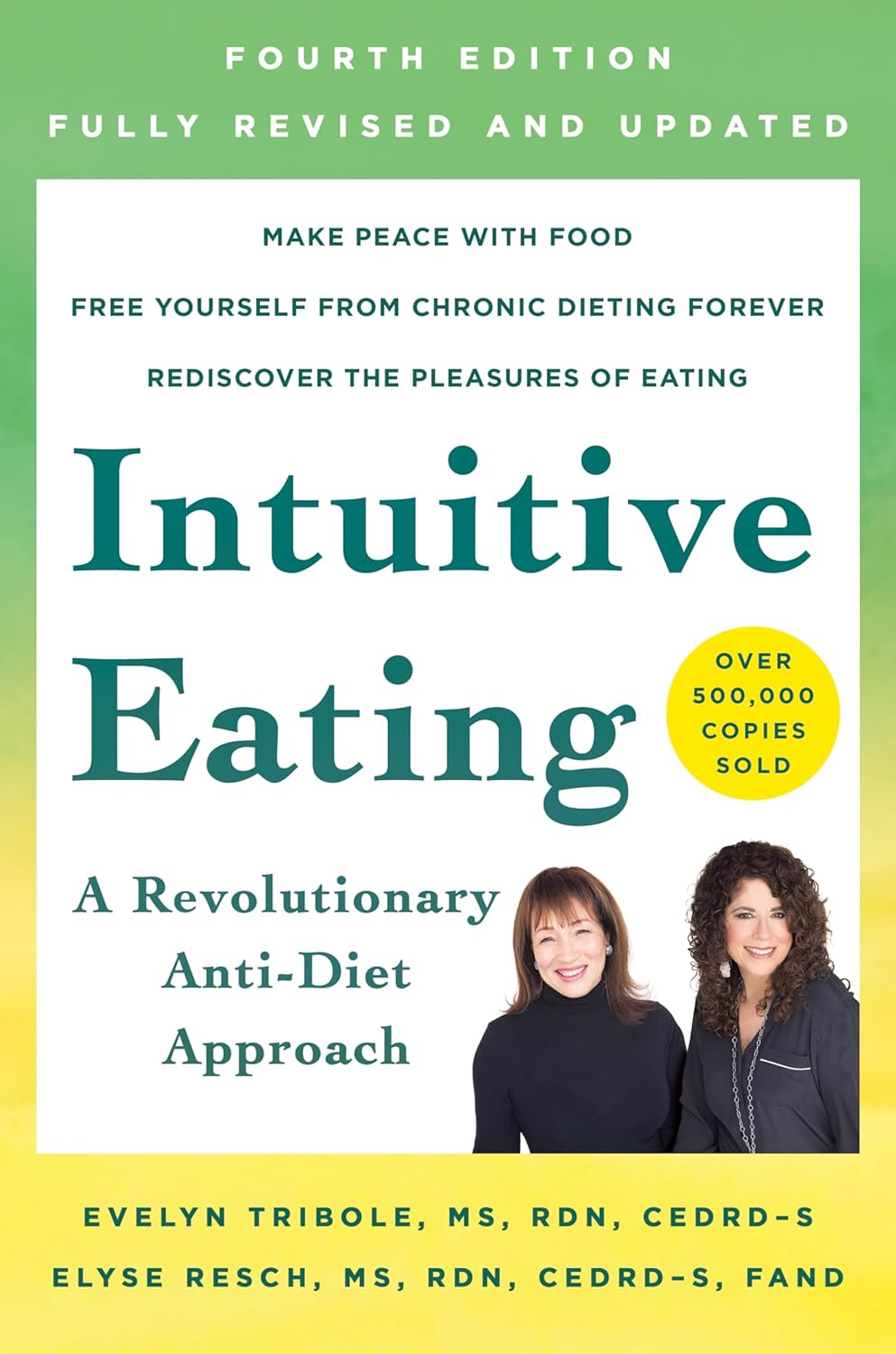
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Overcoming Tendonitis – by Dr. Steven Low & Dr. Frank Skretch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you assumed tendonitis to be an inflammatory condition, you’re not alone. However, it’s not; the “-itis” nomenclature is a misnomer, and while one can rarely go wrong with reducing chronic/systemic inflammation, it’s not the cure for tendonitis.
What, then, is tendonitis and what does cure it? It’s a non-inflammatory proliferation disorder, meaning, something is growing (or in this case, simply being replaced) in a way it shouldn’t. As to fixing it, that’s more complex.
This book does cover 20 interventions (sorted into “major” and “minor”), ranging from exercise therapies to surgery, with many things between. It also examines popular myths that do not help, such as rest, ice, heat, and analgesics.
The style of this book is hard science, but don’t worry, it explains everything along the way. It does however mean that if you’re not very accustomed to wading through scientific material, you can’t just dip into the middle of the book and be guaranteed to understand what’s going on. Indeed, before even getting to discussing tendonitis/tendinopathy, the first chapter is very reassuringly dedicated to “understanding the levels and classification of evidence in studies”, along with the assorted scales and guidelines of the Center for Evidence-Based Medicine.
The rest, however, is about the etiology, diagnosis, and treatment of tendonitis and tendinopathy more generally. One interesting thing is that, according to the abundant high-quality evidence presented in this book, what works for one body part’s tendonitis does not necessarily work for another body part, so we get quite a part-by-part rundown.
Bottom line: this book has a wealth of useful, applicable information about management of tendonitis, making it indispensable if you or a loved one suffer from such—but settle in, because it’s not a light read.
Click here to check out Overcoming Tendonitis, and overcome tendonitis!
Share This Post
-
What I Wish People Knew About Dementia – by Dr. Wendy Mitchell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hear a lot from doctors who work with dementia patients; sometimes we hear from carers too. In this case, the author spent 20 years working for the NHS, before being diagnosed with young-onset dementia, at the age of 58. Like many health industry workers who got a life-changing diagnosis, she quickly found it wasn’t fun being on the other side of things, and vowed to spend her time researching, and raising awareness about, dementia.
Many people assume that once a person has dementia, they’re basically “gone before they’re gone”, which can rapidly become a self-fulfilling prophecy as that person finds themself isolated and—though this word isn’t usually used—objectified. Talked over, viewed (and treated) more as a problem than a person. Cared for hopefully, but again, often more as a patient than a person. If doctors struggle to find the time for the human side of things with most patients most of the time, this is only accentuated when someone needs more time and patience than average.
Instead, Dr. Mitchell—an honorary doctorate, by the way, awarded for her research—writes about what it’s actually like to be a human with dementia. Everything from her senses, how she eats, the experience of eating in care homes, the process of boiling an egg… To relationships, how care changes them, to the challenges of living alone. And communication, confusion, criticism, the language used by professionals, or how things are misrepresented in popular media. She also talks about the shifting sense of self, and brings it all together with gritty optimism.
The style is deeply personal, yet lucid and clear. While dementia is most strongly associated with memory loss and communication problems, this hasn’t affected her ability to write well (7 years into her diagnosis, in case you were wondering).
Bottom line: if you’d like to read a first-person view of dementia, then this is an excellent opportunity to understand it from the view of, as the subtitle goes, someone who knows.
Click here to check out What I Wish People Knew About Dementia, and then know those things!
Share This Post
-
How Does Fat Actually Leave The Body? Where Does It Go?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fat loss is often misunderstood, with many believing it simply “vanishes” through exercise, is simply excreted in solid form in the bathroom, or materially disappears when converted for energy. However, the principle of conservation of mass plays out here, in that the mass in fat doesn’t disappear—it changes its arrangement:
In and out
Fat is composed of carbon, hydrogen, and oxygen atoms, with an example common form of fat in the body being C55H104O6. That’s a lot of Cs and Hs, and a few Os.
When fat leaves the body, it has been primarily converted into carbon dioxide (CO2) and water (H2O).
According to a 2014 study by the University of South Wales, 84% of the mass of fat exits the body as CO2 exhaled through breathing, while 16% leaves as water through sweat, urine, and other bodily fluids (all of which contain H2O).
You’ll notice there are a lot more Os going out, proportionally, than we originally had in the C55H104O6. For this reason, the process requires oxygen intake; for every 10 kilograms of fat burned, by simple mathematics the body needs around 29 kilograms of oxygen.
Physical activity plays a crucial role in fat loss. When the body exerts itself, it naturally switches to a higher oxygen metabolism necessary for fat breakdown. This effect is amplified during intermittent fasting, which boosts human growth hormone (HGH), a hormone that aids in fat metabolism.
However, simply hyperventilating won’t work; exercise is essential to activate these processes—otherwise it’s just a case of oxygen in, oxygen out, without involving the body’s chemical energy reserves.
Consequently, one of the best diet-and-exercise combinations for fat loss is intermittent fasting with high-intensity interval training.
And, as for what to eat, this video says raw vegan, but honestly, that’s not scientific consensus. However, a diet rich in unprocessed (or minimally processed) fruits and vegetables definitely is where it’s at, with the plant-heavy Mediterranean diet generally scoring highest—which can be further improved by skipping the mammals to make it pesco-Mediterranean. Current scientific consensus does not give any extra benefits for also omitting moderate consumption of fish and fermented dairy products, so include those if you want, or skip those if you prefer.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are You A Calorie-Burning Machine? (Calorie Mythbusting)
Take care!
Share This Post
Related Posts
-
Why do I need to take some medicines with food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever been instructed to take your medicine with food and wondered why? Perhaps you’ve wondered if you really need to?
There are varied reasons, and sometimes complex science and chemistry, behind why you may be advised to take a medicine with food.
To complicate matters, some similar medicines need to be taken differently. The antibiotic amoxicillin with clavulanic acid (sold as Amoxil Duo Forte), for example, is recommended to be taken with food, while amoxicillin alone (sold as Amoxil), can be taken with or without food.
Different brands of the same medicine may also have different recommendations when it comes to taking it with food.
Ron Lach/Pexels Food impacts drug absorption
Food can affect how fast and how much a drug is absorbed into the body in up to 40% of medicines taken orally.
When you have food in your stomach, the makeup of the digestive juices change. This includes things like the fluid volume, thickness, pH (which becomes less acidic with food), surface tension, movement and how much salt is in your bile. These changes can impair or enhance drug absorption.
Eating a meal also delays how fast the contents of the stomach move into the small intestine – this is known as gastric emptying. The small intestine has a large surface area and rich blood supply – and this is the primary site of drug absorption.
Eating a meal with medicine will delay its onset. Farhad/Pexels Eating a larger meal, or one with lots of fibre, delays gastric emptying more than a smaller meal. Sometimes, health professionals will advise you to take a medicine with food, to help your body absorb the drug more slowly.
But if a drug can be taken with or without food – such as paracetamol – and you want it to work faster, take it on an empty stomach.
Food can make medicines more tolerable
Have you ever taken a medicine on an empty stomach and felt nauseated soon after? Some medicines can cause stomach upsets.
Metformin, for example, is a drug that reduces blood glucose and treats type 2 diabetes and polycystic ovary syndrome. It commonly causes gastrointestinal symptoms, with one in four users affected. To combat these side effects, it is generally recommended to be taken with food.
The same advice is given for corticosteroids (such as prednisolone/prednisone) and certain antibiotics (such as doxycycline).
Taking some medicines with food makes them more tolerable and improves the chance you’ll take it for the duration it’s prescribed.
Can food make medicines safer?
Ibuprofen is one of the most widely used over-the-counter medicines, with around one in five Australians reporting use within a two-week period.
While effective for pain and inflammation, ibuprofen can impact the stomach by inhibiting protective prostaglandins, increasing the risk of bleeding, ulceration and perforation with long-term use.
But there isn’t enough research to show taking ibuprofen with food reduces this risk.
Prolonged use may also affect kidney function, particularly in those with pre-existing conditions or dehydration.
The Australian Medicines Handbook, which guides prescribers about medicine usage and dosage, advises taking ibuprofen (sold as Nurofen and Advil) with a glass of water – or with a meal if it upsets your stomach.
If it doesn’t upset your stomach, ibuprofen can be taken with water. Tbel Abuseridze/Unsplash A systematic review published in 2015 found food delays the transit of ibuprofen to the small intestine and absorption, which delays therapeutic effect and the time before pain relief. It also found taking short courses of ibuprofen without food reduced the need for additional doses.
To reduce the risk of ibuprofen causing damage to your stomach or kidneys, use the lowest effective dose for the shortest duration, stay hydrated and avoid taking other non-steroidal anti-inflammatory medicines at the same time.
For people who use ibuprofen for prolonged periods and are at higher risk of gastrointestinal side effects (such as people with a history of ulcers or older adults), your prescriber may start you on a proton pump inhibitor, a medicine that reduces stomach acid and protects the stomach lining.
How much food do you need?
When you need to take a medicine with food, how much is enough?
Sometimes a full glass of milk or a couple of crackers may be enough, for medicines such as prednisone/prednisolone.
However, most head-to-head studies that compare the effects of a medicine “with food” and without, usually use a heavy meal to define “with food”. So, a cracker may not be enough, particularly for those with a sensitive stomach. A more substantial meal that includes a mix of fat, protein and carbohydrates is generally advised.
Your health professional can advise you on which of your medicines need to be taken with food and how they interact with your digestive system.
Mary Bushell, Clinical Associate Professor in Pharmacy, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brothy Beans & Greens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Eat beans and greens”, we say, “but how”, you ask. Here’s how! Tasty, filling, and fulfilling, this dish is full of protein, fiber, vitamins, minerals, and assorted powerful phytochemicals.
You will need
- 2½ cups low-sodium vegetable stock
- 2 cans cannellini beans, drained and rinsed
- 1 cup kale, stems removed and roughly chopped
- 4 dried shiitake mushrooms
- 2 shallots, sliced
- ½ bulb garlic, crushed
- 1 tbsp white miso paste
- 1 tbsp nutritional yeast
- 1 tsp rosemary leaves
- 1 tsp thyme leaves
- 1 tsp black pepper, coarse ground
- ½ tsp red chili flakes
- Juice of ½ lemon
- Extra virgin olive oil
- Optional: your favorite crusty bread, perhaps using our Delicious Quinoa Avocado Bread recipe
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a skillet and fry the shallots for 2–3 minutes.
2) Add the nutritional yeast, garlic, herbs, and spices, and stir for another 1 minute.
3) Add the beans, vegetable stock, and mushrooms. Simmer for 10 minutes.
4) Add the miso paste, stirring well to dissolve and distribute evenly.
5) Add the kale until it begins to wilt, and remove the pot from the heat.
6) Add the lemon juice and stir.
7) Serve; we recommend enjoying it with crusty wholegrain bread.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Dr. Greger’s Daily Dozen ← beans and greens up top!
- The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eating Disorders: More Varied (And Prevalent) Than People Think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Disordered Eating Beyond The Stereotypes
Around 10% of Americans* have (or have had) an eating disorder. That might not seem like a high percentage, but that’s one in ten; do you know 10 people? If so, it might be a topic that’s near to you.
*Source: Social and economic cost of eating disorders in the United States of Americ
Our hope is that even if you yourself have never had such a problem in your life, today’s article will help arm you with knowledge. You never know who in your life might need your support.
Very misunderstood
Eating disorders are so widely misunderstood in so many ways that we nearly made this a Friday Mythbusting edition—but we preface those with a poll that we hope to be at least somewhat polarizing or provide a spectrum of belief. In this case, meanwhile, there’s a whole cluster of myths that cannot be summed up in one question. So, here we are doing a Psychology Sunday edition instead.
“Eating disorders aren’t that important”
Eating disorders are the second most deadly category of mental illness, second only to opioid addiction.
Anorexia specifically has the highest case mortality rate of any mental illness:
Source: National Association of Anorexia Nervosa & Associated Disorders: Eating Disorder Statistics
So please, if someone needs help with an eating disorder (including if it’s you), help them.
“Eating disorders are for angsty rebellious teens”
While there’s often an element of “this is the one thing I can control” to some eating disorders (including anorexia and bulimia), eating disorders very often present in early middle-age, very often amongst busy career-driven individuals using it as a coping mechanism to have a feeling of control in their hectic lives.
13% of women over 50 report current core eating disorder symptoms, and that is probably underreported.
Source: as above; scroll to near the bottom!
“Eating disorders are a female thing”
Nope. Officially, men represent around 25% of people diagnosed with eating disorders, but women are 5x more likely to get diagnosed, so you can do the math there. Women are also 1.5% more likely to receive treatment for it.
By the time men do get diagnosed, they’ve often done a lot more damage to their bodies because they, as well as other people, have overlooked the possibility of their eating being disordered, due to the stereotype of it being a female thing.
Source: as above again!
“Eating disorders are about body image”
They can be, but that’s far from the only kind!
Some can be about control of diet, not just for the sake of controlling one’s body, but purely for the sake of controlling the diet itself.
Still yet others can be not about body image or control, like “Avoidant/Restrictive Food Intake Disorder”, which in lay terms sometimes gets dismissed as “being a picky eater” or simply “losing one’s appetite”, but can be serious.
For example, a common presentation of the latter might be a person who is racked with guilt and/or anxiety, and simply stops eating, because either they don’t feel they deserve it, or “how can I eat at a time like this, when…?” but the time is an ongoing thing so their impromptu fast is too.
Still yet even more others might be about trying to regulate emotions by (in essence) self-medicating with food—not in the healthy “so eat some fruit and veg and nuts etc” sense, but in the “Binge-Eating Disorder” sense.
And that latter accounts for a lot of adults.
You can read more about these things here:
Psychology Today | Types of Eating Disorder ← it’s pop-science, but it’s a good overview
Take care! And if you have, or think you might have, an eating disorder, know that there are organizations that can and will offer help/support in a non-judgmental fashion. Here’s the ANAD’s eating disorder help resource page, for example.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: