Improve Your Insulin Sensitivity!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about blood sugar management, for example:
10 Ways To Balance Blood Sugars ← this one really is the most solid foundation possible; if you do nothing else, do these 10 things!
And as for why we care:
Good (Or Bad) Health Starts With Your Blood
…because the same things that cause type 2 diabetes, go on to cause many other woes, with particularly strong comorbidities in the case of Alzheimer’s disease and other dementias, as well as heart disease of various kinds, and a long long laundry list of immune dysfunctions / inflammatory disorders in general.
In short, if you can’t keep your blood sugars even, the rest of your health will fall like so many dominoes.
Getting a baseline
Are you counting steps? Counting calories? Monitoring your sleep? Heart rate zones? These all have their merits:
- Steps: One More Resource Against Osteoporosis!
- Calories: Is Cutting Calories The Key To Healthy Long Life?
- Sleep: A Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
- Heart Rate Zones: Heart Rate Zones, Oxalates, & More
But something far fewer people do unless they have diabetes or are very enthusiastic about personal health, is to track blood sugars:
Here’s how: Track Your Blood Sugars For Better Personalized Health
And for understanding some things to watch out for when using a continuous glucose monitor:
Continuous Glucose Monitors Without Diabetes: Pros & Cons
Writer’s anecdote: I decided to give one a try for a few months, and so far it has been informative, albeit unexciting. It seems that with my diet (mostly whole-foods plant based, though I do have a wholegrain wheat product about twice per week (usually: flatbread once, pasta once) which is… Well, we could argue it’s whole-food plant based, but let’s be honest, it’s a little processed), my blood sugars don’t really have spikes at all; the graph looks more like gently rolling low hills (which is good). However! Even so, by experimenting with it, I can see for myself what differences different foods/interventions make to my blood sugars, which is helpful, and it also improves my motivation for intermittent fasting. It also means that if I think “hmm, my energy levels are feeling low; I need a snack” I can touch my phone to my arm and find out if that is really the reason (so far, it hasn’t been). I expect that as I monitor my blood sugars continuously and look at the data frequently, I’ll start to get a much more intuitive feel for my own blood sugars, in much the same way I can generally intuit my hormone levels correctly after years of taking-and-testing.
So much for blood sugars. Now, what about insulin?
Step Zero
If taking care of blood sugars is step one, then taking care of insulin is step zero.
Often’s it’s viewed the other way around: we try to keep our blood sugars balanced, to reduce the need for our bodies to produce so much insulin that it gets worn out. And that’s good and fine, but…
To quote what we wrote when reviewing “Why We Get Sick” last month:
❝Dr. Bikman makes the case that while indeed hyper- or hypoglycemia bring their problems, mostly these are symptoms rather than causes, and the real culprit is insulin resistance, and this is important for two main reasons:
- Insulin resistance occurs well before the other symptoms set in (which means: it is the thing that truly needs to be nipped in the bud; if your fasting blood sugars are rising, then you missed “nipping it in the bud” likely by a decade or more)
- Insulin resistance causes more problems than “mere” hyperglycemia (the most commonly-known result of insulin resistance) does, so again, it really needs to be considered separately from blood sugar management.
This latter, Dr. Bikman goes into in great detail, linking insulin resistance (even if blood sugar levels are normal) to all manner of diseases (hence the title).
You may be wondering: how can blood sugar levels be normal, if we have insulin resistance?
And the answer is that for as long as it is still able, your pancreas will just faithfully crank out more and more insulin to deal with the blood sugar levels that would otherwise be steadily rising. Since people measure blood sugar levels much more regularly than anyone checks for actual insulin levels, this means that one can be insulin resistant for years without knowing it, until finally the pancreas is no longer able to keep up with the demand—then that’s when people finally notice.❞
You can read the full book review here:
Now, testing for insulin is not so quick, easy, or accessible as testing for glucose, but it can be worthwhile to order such a test—because, as discussed, your insulin levels could be high even while your blood sugars are still normal, and it won’t be until the pancreas finally reaches breaking point that your blood sugars show it.
So, knowing your insulin levels can help you intervene before your pancreas reaches that breaking point.
We can’t advise on local services available for ordering blood tests (because they will vary depending on location), but a simple Google search should suffice to show what’s available in your region.
Once you know your insulin levels (or even if you don’t, but simply take the principled position that improving insulin sensitivity will be good regardless), you can set about managing them.
Insulin sensitivity is important, because the better it is (higher insulin sensitivity), the less insulin the pancreas has to make to tidy up the same amount of glucose into places that are good for it to go—which is good. In contrast, the worse it is (higher insulin resistance), the more insulin the pancreas has to make to do the same blood sugar management. Which is bad.
What to do about it
We imagine you will already be eating in a way that is conducive to avoiding or reversing type 2 diabetes, but for anyone who wants a refresher,
See: How To Prevent And Reverse Type 2 Diabetes
…which yes, as well as meaning eating/avoiding certain foods, does recommend intermittent fasting. For anyone who wants a primer on that,
See: Intermittent Fasting: Methods & Benefits
There are also drugs you may want to consider:
Metformin Without Diabetes, For Weight-Loss & More
And “nutraceuticals” that sound like drugs, for example:
Glutathione’s Benefits: The Usual And The Unique ← the good news is, it’s found in several common foods
You may have heard the hype about “nature’s Ozempic”, and berberine isn’t exactly that (works in mostly different ways), but its benefits do include improving insulin sensitivity:
Berberine For Metabolic Health
Lastly, while eating for blood sugar management is all well and good, do be aware that some things affect insulin levels without increased blood sugar levels. So even if you’re using a CGM, you may go blissfully unaware of an insulin spike, because there was no glucose spike on the graph—and in contrast, there could even be a dip in blood sugar levels, if you consumed something that increased insulin levels without providing glucose at the same time, making you think “I should have some carbs”, which visually on the graph would even out your blood sugars, but invisibly, would worsen the already-extant insulin spike.
Read more about this: Strange Things Happening In The Islets Of Langerhans: When Carbs, Proteins, & Fats Switch Metabolic Roles
Now, since you probably can’t test your insulin at a moment’s notice, the way to watch out for this is “hmm, I ate some protein/fats (delete as applicable) without carbs and my blood sugars dipped; I know what’s going on here”.
Want to know more?
We heartily recommend the “Why We Get Sick” book we linked above, as this focuses on insulin resistance/sensitivity itself!
However, a very good general primer on blood sugar management (and thus, by extension, at least moderately good insulin management), is:
Glucose Revolution: The Life-Changing Power of Balancing Your Blood Sugar – by Jessie Inchauspé
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
State Regulators Know Health Insurance Directories Are Full of Wrong Information. They’re Doing Little to Fix It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: America’s Mental Barrier:How Insurers Interfere With Mental Health Care
- Extensive Errors: Many states have sought to make insurers clean up their health plans’ provider directories over the past decade. But the errors are still widespread.
- Paltry Penalties: Most state insurance agencies haven’t issued a fine for provider directory errors since 2019. When companies have been penalized, the fines have been small and sporadic.
- Ghostbusters: Experts said that stricter regulations and stronger fines are needed to protect insurance customers from these errors, which are at the heart of so-called ghost networks.
These highlights were written by the reporters and editors who worked on this story.
To uncover the truth about a pernicious insurance industry practice, staffers with the New York state attorney general’s office decided to tell a series of lies.
So, over the course of 2022 and 2023, they dialed hundreds of mental health providers in the directories of more than a dozen insurance plans. Some staffers pretended to call on behalf of a depressed relative. Others posed as parents asking about their struggling teenager.
They wanted to know two key things about the supposedly in-network providers: Do you accept insurance? And are you accepting new patients?
The more the staffers called, the more they realized that the providers listed either no longer accepted insurance or had stopped seeing new patients. That is, if they heard back from the providers at all.
In a report published last December, the office described rampant evidence of these “ghost networks,” where health plans list providers who supposedly accept that insurance but who are not actually available to patients. The report found that 86% of the listed mental health providers who staffers had called were “unreachable, not in-network, or not accepting new patients.” Even though insurers are required to publish accurate directories, New York Attorney General Letitia James’ office didn’t find evidence that the state’s own insurance regulators had fined any insurers for their errors.
Shortly after taking office in 2021, Gov. Kathy Hochul vowed to combat provider directory misinformation, so there seemed to be a clear path to confronting ghost networks.
Yet nearly a year after the publication of James’ report, nothing has changed. Regulators can’t point to a single penalty levied for ghost networks. And while a spokesperson for New York state’s Department of Financial Services has said that “nation-leading consumer protections” are in the works, provider directories in the state are still rife with errors.
A similar pattern of errors and lax enforcement is happening in other states as well.
In Arizona, regulators called hundreds of mental health providers listed in the networks of the state’s most popular individual health plans. They couldn’t schedule visits with nearly 2 out of every 5 providers they called. None of those companies have been fined for their errors.
In Massachusetts, the state attorney general investigated alleged efforts by insurers to restrict their customers’ mental health benefits. The insurers agreed to audit their mental health provider listings but were largely allowed to police themselves. Insurance regulators have not fined the companies for their errors.
In California, regulators received hundreds of complaints about provider listings after one of the nation’s first ghost network regulations took effect in 2016. But under the new law, they have actually scaled back on fining insurers. Since 2016, just one plan was fined — a $7,500 penalty — for posting inaccurate listings for mental health providers.
ProPublica reached out to every state insurance commission to see what they have done to curb rampant directory errors. As part of the country’s complex patchwork of regulations, these agencies oversee plans that employers purchase from an insurer and that individuals buy on exchanges. (Federal agencies typically oversee plans that employers self-fund or that are funded by Medicare.)
Spokespeople for the state agencies told ProPublica that their “many actions” resulted in “significant accountability.” But ProPublica found that the actual actions taken so far do not match the regulators’ rhetoric.
“One of the primary reasons insurance commissions exist is to hold companies accountable for what they are advertising in their contracts,” said Dr. Robert Trestman, a leading American Psychiatric Association expert who has testified about ghost networks to the U.S. Senate Committee on Finance. “They’re not doing their job. If they were, we would not have an ongoing problem.”
Most states haven’t fined a single company for publishing directory errors since 2019. When they do, the penalties have been small and sporadic. In an average year, fewer than a dozen fines are issued by insurance regulators for directory errors, according to information obtained by ProPublica from almost every one of those agencies. All those fines together represent a fraction of 1% of the billions of dollars in profits made by the industry’s largest companies. Health insurance experts told ProPublica that the companies treat the fines as a “cost of doing business.”
Insurers acknowledge that errors happen. Providers move. They retire. Their open appointments get booked by other patients. The industry’s top trade group, AHIP, has told lawmakers that companies contact providers to verify that their listings are accurate. The trade group also has stated that errors could be corrected faster if the providers did a better job updating their listings.
But providers have told us that’s bogus. Even when they formally drop out of a network, they’re not always removed from the insurer’s lists.
The harms from ghost networks are real. ProPublica reported on how Ravi Coutinho, a 36-year-old entrepreneur from Arizona, had struggled for months to access the mental health and addiction treatment that was covered by his health plan. After nearly two dozen calls to the insurer and multiple hospitalizations, he couldn’t find a therapist. Last spring, he died, likely due to complications from excessive drinking.
Health insurance experts said that, unless agencies can crack down and issue bigger fines, insurers will keep selling error-ridden plans.
“You can have all the strong laws on the books,” said David Lloyd, chief policy officer with the mental health advocacy group Inseparable. “But if they’re not being enforced, then it’s kind of all for nothing.”
The problem with ghost networks isn’t one of awareness. States, federal agencies, researchers and advocates have documented them time and again for years. But regulators have resisted penalizing insurers for not fixing them.
Two years ago, the Arizona Department of Insurance and Financial Institutions began to probe the directories used by five large insurers for plans that they sold on the individual market. Regulators wanted to find out if they could schedule an appointment with mental health providers listed as accepting new patients, so their staff called 580 providers in those companies’ directories.
Thirty-seven percent of the calls did not lead to an appointment getting scheduled.
Even though this secret-shopper survey found errors at a lower rate than what had been found in New York, health insurance experts who reviewed Arizona’s published findings said that the results were still concerning.
Ghost network regulations are intended to keep provider listings as close to error-free as possible. While the experts don’t expect any insurer to have a perfect directory, they said that double-digit error rates can be harmful to customers.
Arizona’s regulators seemed to agree. In a January 2023 report, they wrote that a patient could be clinging to the “last few threads of hope, which could erode if they receive no response from a provider (or cannot easily make an appointment).”
Secret-shopper surveys are considered one of the best ways to unmask errors. But states have limited funding, which restricts how often they can conduct that sort of investigation. Michigan, for its part, mostly searches for inaccuracies as part of an annual review of a health plan. Nevada investigates errors primarily if someone files a complaint. Christine Khaikin, a senior health policy attorney for the nonprofit advocacy group Legal Action Center, said fewer surveys means higher odds that errors go undetected.
Some regulators, upon learning that insurers may not be following the law, still take a hands-off approach with their enforcement. Oregon’s Department of Consumer and Business Services, for instance, conducts spot checks of provider networks to see if those listings are accurate. If they find errors, insurers are asked to fix the problem. The department hasn’t issued a fine for directory errors since 2019. A spokesperson said the agency doesn’t keep track of how frequently it finds network directory errors.
Dave Jones, a former insurance commissioner in California, said some commissioners fear that stricter enforcement could drive companies out of their states, leaving their constituents with fewer plans to choose from.
Even so, staffers at the Arizona Department of Insurance and Financial Institutions wrote in the report that there “needs to be accountability from insurers” for the errors in their directories. That never happened, and the agency concealed the identities of the companies in the report. A department spokesperson declined to provide the insurers’ names to ProPublica and did not answer questions about the report.
Since January 2023, Arizonans have submitted dozens of complaints to the department that were related to provider networks. The spokesperson would not say how many were found to be substantiated, but the department was able to get insurers to address some of the problems, documents obtained through an open records request show.
According to the department’s online database of enforcement actions, not a single one of those companies has been fined.
Sometimes, when state insurance regulators fail to act, attorneys general or federal regulators intervene in their stead. But even then, the extra enforcers haven’t addressed the underlying problem.
For years, the Massachusetts Division of Insurance didn’t fine any company for ghost networks, so the state attorney general’s office began to investigate whether insurers had deceived consumers by publishing inaccurate directories. Among the errors identified: One plan had providers listed as accepting new patients but no actual appointments were available for months; another listed a single provider more than 10 times at different offices.
In February 2020, Maura Healey, who was then the Massachusetts attorney general, announced settlements with some of the state’s largest health plans. No insurer admitted wrongdoing. The companies, which together collect billions in premiums each year, paid a total of $910,000. They promised to remove providers who left their networks within 30 days of learning about that decision. Healey declared that the settlements would lead to “unprecedented changes to help ensure patients don’t have to struggle to find behavioral health services.”
But experts who reviewed the settlements for ProPublica identified a critical shortcoming. While the insurers had promised to audit directories multiple times a year, the companies did not have to report those findings to the attorney general’s office. Spokespeople for Healey and the attorney general’s office declined to answer questions about the experts’ assessments of the settlements.
After the settlements were finalized, Healey became the governor of Massachusetts and has been responsible for overseeing the state’s insurance division since she took office in January 2023. Her administration’s regulators haven’t brought any fines over ghost networks.
Healey’s spokesperson declined to answer questions and referred ProPublica to responses from the state’s insurance division. A division spokesperson said the state has taken steps to strengthen its provider directory regulations and streamline how information about in-network providers gets collected. Starting next year, the spokesperson said that the division “will consider penalties” against any insurer whose “provider directory is found to be materially noncompliant.”
States that don’t have ghost network laws have seen federal regulators step in to monitor directory errors.
In late 2020, Congress passed the No Surprises Act, which aimed to cut down on the prevalence of surprise medical bills from providers outside of a patient’s insurance network. Since then, the Centers for Medicare and Medicaid Services, which oversees the two large public health insurance programs, has reached out to every state to see which ones could handle enforcement of the federal ghost network regulations.
At least 15 states responded that they lacked the ability to enforce the new regulation. So CMS is now tasked with watching out for errors in directories used by millions of insurance customers in those states.
Julie Brookhart, a spokesperson for CMS, told ProPublica that the agency takes enforcement of the directory error regulations “very seriously.” She said CMS has received a “small number” of provider directory complaints, which the agency is in the process of investigating. If it finds a violation, Brookhart said regulators “will take appropriate enforcement action.”
But since the requirement went into effect in January 2022, CMS hasn’t fined any insurer for errors. Brookhart said that CMS intends to develop further guidelines with other federal agencies. Until that happens, Brookhart said that insurers are expected to make “good-faith” attempts to follow the federal provider directory rules.
Last year, five California lawmakers proposed a bill that sought to get rid of ghost networks around the state. If it passed, AB 236 would limit the number of errors allowed in a directory — creating a cap of 5% of all providers listed — and raise penalties for violations. California would become home to one of the nation’s toughest ghost network regulations.
The state had already passed one of America’s first such regulations in 2015, requiring insurers to post directories online and correct inaccuracies on a weekly basis.
Since the law went into effect in 2016, insurance customers have filed hundreds of complaints with the California Department of Managed Health Care, which oversees health plans for nearly 30 million enrollees statewide.
Lawyers also have uncovered extensive evidence of directory errors. When San Diego’s city attorney, Mara Elliott, sued several insurers over publishing inaccurate directories in 2021, she based the claims on directory error data collected by the companies themselves. Citing that data, the lawsuits noted that error rates for the insurers’ psychiatrist listings were between 26% and 83% in 2018 and 2019. The insurers denied the accusations and convinced a judge to dismiss the suits on technical grounds. A panel of California appeals court judges recently reversed those decisions; the cases are pending.
The companies have continued to send that data to the DMHC each year — but the state has not used it to examine ghost networks. California is among the states that typically waits for a complaint to be filed before it investigates errors.
“The industry doesn’t take the regulatory penalties seriously because they’re so low,” Elliott told ProPublica. “It’s probably worth it to take the risk and see if they get caught.”
California’s limited enforcement has resulted in limited fines. Over the past eight years, the DMHC has issued just $82,500 in fines for directory errors involving providers of any kind. That’s less than one-fifth of the fines issued in the two years before the regulation went into effect.
A spokesperson for the DMHC said its regulators continue “to hold health plans accountable” for violating ghost network regulations. Since 2018, the DMHC has discovered scores of problems with provider directories and pushed health plans to correct the errors. The spokesperson said that the department’s oversight has also helped some customers get reimbursed for out-of-network costs incurred due to directory errors.
“A lower fine total does not equate to a scaling back on enforcement,” the spokesperson said.
Dr. Joaquin Arambula, one of the state Assembly members who co-sponsored AB 236, disagreed. He told ProPublica that California’s current ghost network regulation is “not effectively being enforced.” After clearing the state Assembly this past winter, his bill, along with several others that address mental health issues, was suddenly tabled this summer. The roadblock came from a surprising source: the administration of the state’s Democratic governor.
Officials with the DMHC, whose director was appointed by Gov. Gavin Newsom, estimated that more than $15 million in extra funding would be needed to carry out the bill’s requirements over the next five years. State lawmakers accused officials of inflating the costs. The DMHC’s spokesperson said that the estimate was accurate and based on the department’s “real experience” overseeing health plans.
Arambula and his co-sponsors hope that their colleagues will reconsider the measure during next year’s session. Sitting before state lawmakers in Sacramento this year, a therapist named Sarah Soroken told the story of a patient who had called 50 mental health providers in her insurer’s directory. None of them could see her. Only after the patient attempted suicide did she get the care she’d sought.
“We would be negligent,” Soroken told the lawmakers, “if we didn’t do everything in our power to ensure patients get the health care they need.”
Paige Pfleger of WPLN/Nashville Public Radio contributed reporting.
Share This Post
-
“Skinny Fat” Explained (& How To Fix It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Skinny fat” is a term you may have seen floating around social media. It describes people who have a low body weight but a high body fat percentage, often resulting in flabby appearance despite being within a weight range considered healthy. Many try dieting and exercising, only to find that neither work.
This video explains what’s going wrong, and how to fix it:
Diet & exercise won’t work if it’s not right
This problem occurs because common weight-loss approaches, such as restrictive dieting and excessive cardio, fail to improve body composition:
- Restrictive dieting reduces both fat and lean mass, keeping the body fat percentage unchanged
- Cardio burns some calories but the underlying metabolic issue hasn’t meaningfully changed, so any loss will be temporary (and most of any immediate loss will be water weight, anyway)
The key to overcoming skinny fat is resistance training. Lifting weights or doing bodyweight exercises helps build muscle, which not only lowers body fat percentage (by simple mathematics; add more muscle and the percentages of other things must go down even if the total amount is the same) and improves overall definition, which is something most people consider nice. However, the real value here is that it actually addresses the underlying metabolic issue—because muscle costs calories to maintain, one’s basal metabolic rate will now be faster, even when you’re sleeping.
This then becomes… Not quite a self-sustaining system, because you do have to still eat well and continue to do resistance training, but your body will be doing most of the work for you, and you’ll find it’s a lot easier to maintain a healthy body composition than to get one in the first place, for exactly the metabolic reason we described.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Visceral Belly Fat & How To Lose It ← this is a different, but adjacent issue (and very important for avoiding metabolic disease risks)
Take care!
Share This Post
-
Celery vs Radish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to radish, we picked the celery.
Why?
It was very close! And yes, surprising, we know. Generally speaking, the more colorful/pigmented an edible plant is, the healthier it is. Celery is just one of those weird exceptions (as is cauliflower, by the way).
Macros-wise, these two are pretty much the same—95% water, with just enough other stuff to hold them together. The proportions of “other stuff” are also pretty much equal.
In the category of vitamins, celery has more vitamin K while radish has more vitamin C; the other vitamins are pretty close to equal. We’ll call this one a minor win for celery, as vitamin K is found in fewer foods than vitamin C.
When it comes to minerals, celery has more calcium, manganese, phosphorus, and potassium, while radish has more copper, iron, selenium, and zinc. We’ll call this a minor win for radish, as the margins are a little wider for its minerals.
So, that makes the score 1–1 so far.
Both plants have an assortment of polyphenols, of which, when we add up the averages, celery comes out on top by some way. Celery also comes out on top when we do a head-to-head of the top flavonoid of each; celery has 5.15mg/100g of apigenin to radish’s 0.63mg/100g kaempferol.
Which means, both are great healthy foods, but celery wins the day.
Want to learn more?
You might like to read:
Celery vs Cucumber – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Broccoli vs Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cabbage, we picked the broccoli.
Why?
Here we go once again pitting two different cultivars of the same species (Brassica oleracea) against each other, and/but once again, there is one that comes out as nutritionally best.
In terms of macros, broccoli has more protein, carbs, and fiber, while they are both low glycemic index foods. The differences are small though, so it’s fairest to call this category a tie.
When it comes to vitamins, broccoli has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while cabbage is not higher in any vitamins. It should be noted that cabbage is still good for these, especially vitamins C and K, but broccoli is simply better.
In the category of minerals, broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while cabbage is not higher in any minerals. Again though, cabbage is still good, especially in calcium, iron, and manganese, but again, broccoli is simply better.
Of course, enjoy either or both! But if you want the nutritionally densest option, it’s broccoli.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Want to sleep longer? Adding mini-bursts of exercise to your evening routine can help – new study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercising before bed has long been discouraged as the body doesn’t have time to wind down before the lights go out.
But new research has found breaking up a quiet, sedentary evening of watching television with short bursts of resistance exercise can lead to longer periods of sleep.
Adults spend almost one third of the 24-hour day sleeping. But the quality and length of sleep can affect long-term health. Sleeping too little or waking often in the night is associated with an increased risk of heart disease and diabetes.
Physical activity during the day can help improve sleep. However, current recommendations discourage intense exercise before going to bed as it can increase a person’s heart rate and core temperature, which can ultimately disrupt sleep.
Nighttime habits
For many, the longest period of uninterrupted sitting happens at home in the evening. People also usually consume their largest meal during this time (or snack throughout the evening).
Insulin (the hormone that helps to remove sugar from the blood stream) tends to be at a lower level in the evening than in the morning.
Together these factors promote elevated blood sugar levels, which over the long term can be bad for a person’s health.
Our previous research found interrupting evening sitting every 30 minutes with three minutes of resistance exercise reduces the amount of sugar in the bloodstream after eating a meal.
But because sleep guidelines currently discourage exercising in the hours before going to sleep, we wanted to know if frequently performing these short bursts of light activity in the evening would affect sleep.
Activity breaks for better sleep
In our latest research, we asked 30 adults to complete two sessions based in a laboratory.
During one session the adults sat continuously for a four-hour period while watching streaming services. During the other session, they interrupted sitting by performing three minutes of body-weight resistance exercises (squats, calf raises and hip extensions) every 30 minutes.
After these sessions, participants went home to their normal life routines. Their sleep that evening was measured using a wrist monitor.
Our research found the quality of sleep (measured by how many times they woke in the night and the length of these awakenings) was the same after the two sessions. But the night after the participants did the exercise “activity breaks” they slept for almost 30 minutes longer.
Identifying the biological reasons for the extended sleep in our study requires further research.
But regardless of the reason, if activity breaks can extend sleep duration, then getting up and moving at regular intervals in the evening is likely to have clear health benefits.
Time to revisit guidelines
These results add to earlier work suggesting current sleep guidelines, which discourage evening exercise before bed, may need to be reviewed.
As the activity breaks were performed in a highly controlled laboratory environment, future research should explore how activity breaks performed in real life affect peoples sleep.
We selected simple, body-weight exercises to use in this study as they don’t require people to interrupt the show they may be watching, and don’t require a large space or equipment.
If people wanted to incorporate activity breaks in their own evening routines, they could probably get the same benefit from other types of exercise. For example, marching on the spot, walking up and down stairs, or even dancing in the living room.
The key is to frequently interrupt evening sitting time, with a little bit of whole-body movement at regular intervals.
In the long run, performing activity breaks may improve health by improving sleep and post-meal blood sugar levels. The most important thing is to get up frequently and move the body, in a way the works best for a person’s individual household.
Jennifer Gale, PhD candidate, Department of Human Nutrition, University of Otago and Meredith Peddie, Senior Lecturer, Department of Human Nutrition, University of Otago
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
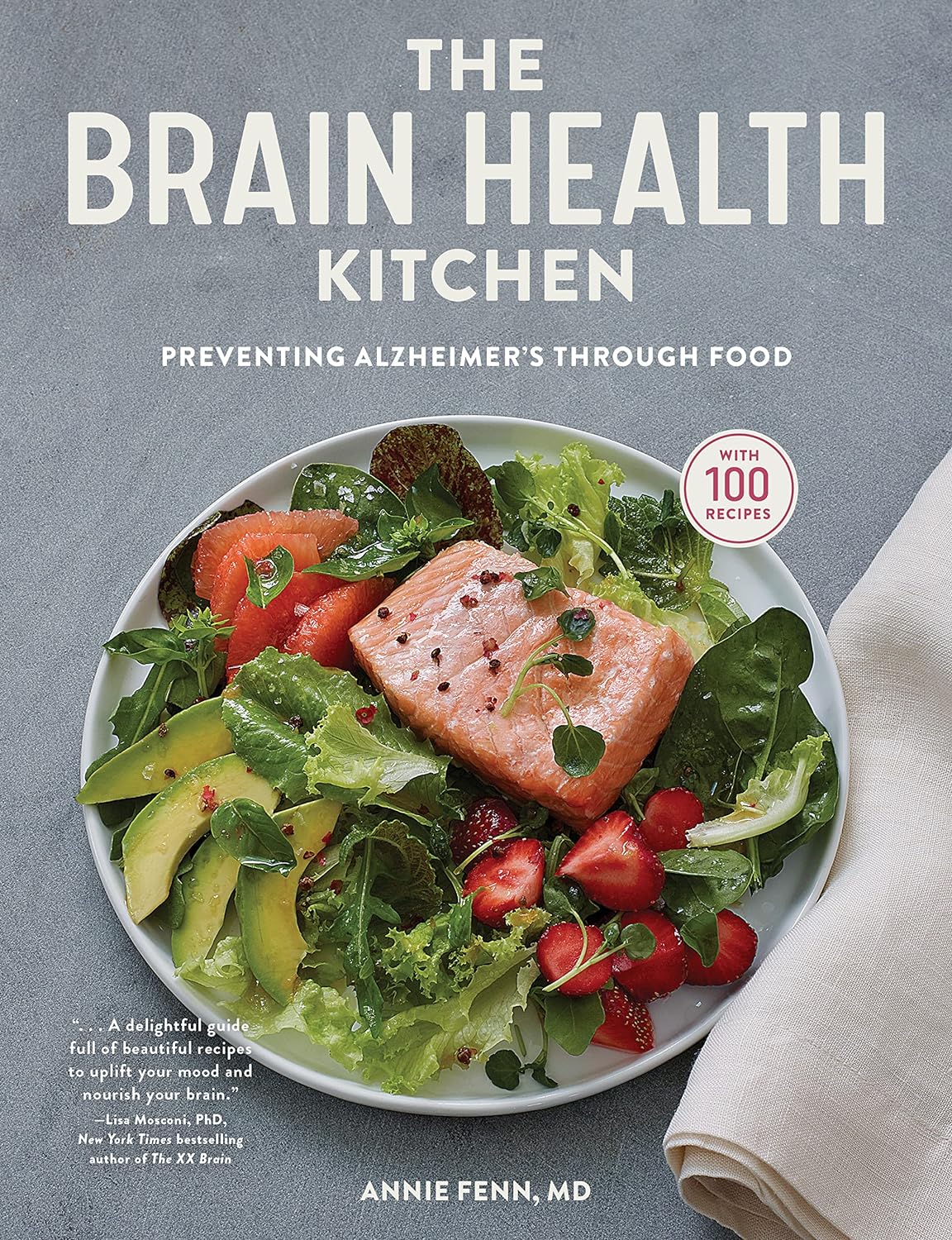
The Brain Health Kitchen – by Dr. Annie Fenn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a cookbook built around the MIND diet, which we talked about in our “Four Ways To Upgrade The Mediterranean Diet” article.
As such, it’s a top-tier gold-standard diet to be following for brain health, and having it as a book of recipes makes actually eating this way a lot easier!
The book does talk about the science first before getting to the recipes, so don’t worry, you won’t have to reverse engineer the dietary guidelines from the recipes; everything is explained well.
The recipes (of which there are 100) are diverse enough to be interesting without being so complicated as to be difficult. The ingredients are largely nutritional powerhouses, and most if not all can be found in your nearest reasonable-sized supermarket. Also, the recipes are (as you might reasonably expect), very plant-forward, but not entirely plant-based (as you might have guessed from the salmon on the front cover).
Bottom line: if you’d like to eat more healthily for your brain, but are a little stumped on what to do with the four ingredients you remember are brain-healthy, this book will help expand your horizons—not to mention your culinary repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: