Why Some People Get Sick More (And How To Not Be One Of Them)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
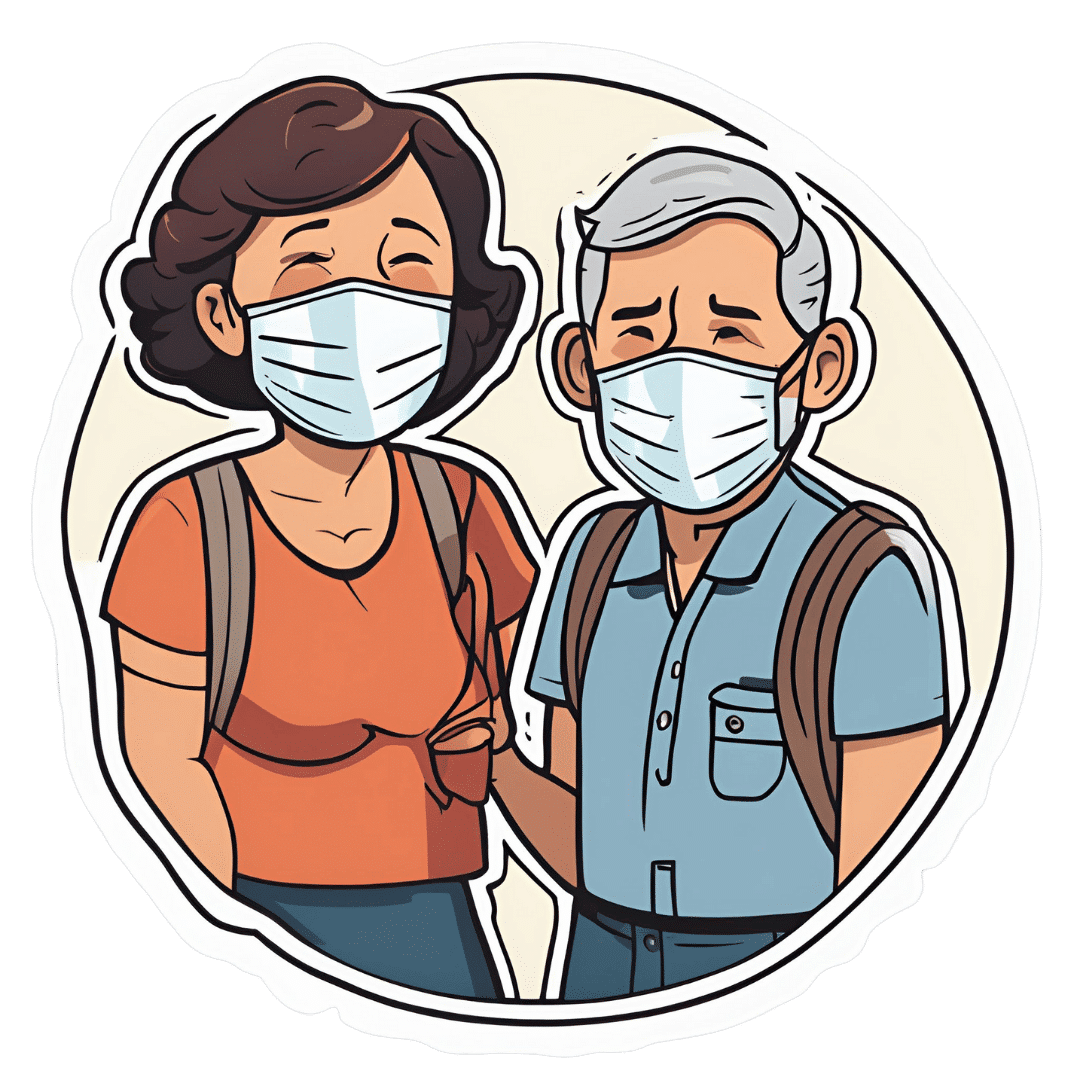
Some people have never yet had COVID (so far so good, this writer included); others are on their third bout already; others have not been so lucky and are no longer with us to share their stories.
Obviously, even the healthiest and/or most careful person can get sick, and it would be folly to be complacent and think “I’m not a person who gets sick; that happens to other people”.
Nor is COVID the only thing out there to worry about; there’s always the latest outbreak-du-jour of something, and there are always the perennials such as cold and flu—which are also not to be underestimated, because both weaken us to other things, and flu has killed very many, from the 50,000,000+ in the 1918 pandemic, to the 700,000ish that it kills each year nowadays.
And then there are the combination viruses:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
So, why are some people more susceptible?
Firstly, some people are simply immunocompromised. This means for example that:
- perhaps they have an inflammatory/autoimmune disease of some kind (e.g. lupus, rheumatoid arthritis, type 1 diabetes), or…
- perhaps they are taking immunosuppressants for some reason (e.g. because they had an organ transplant), or…
- perhaps they have a primary infection that leaves them vulnerable to secondary infections. Most infections will do this to some degree or another, but some are worse for it than others; untreated HIV is a clear example. The HIV itself may not kill people, but (if untreated) the resultant AIDS will leave a person open to being killed by almost any passing opportunistic pathogen. Pneumonia of various kinds being high on the list, but it could even be something as simple as the common cold, without a working immune system to fight it.
See also: How To Prevent (Or Reduce) Inflammation
And for that matter, since pneumonia is a very common last-nail-in-the-coffin secondary infection (especially: older people going into hospital with one thing, getting a secondary infection and ultimately dying as a result), it’s particularly important to avoid that, so…
See also: Pneumonia: What We Can & Can’t Do About It
Secondly, some people are not immunocompromised per the usual definition of the word, but their immune system is, arguably, compromised.
Cortisol, the stress hormone, is an immunosuppressant. We need cortisol to live, but we only need it in small bursts here and there (such as when we are waking up the morning). When high cortisol levels become chronic, so too does cortisol’s immunosuppressant effect.
Top things that cause elevated cortisol levels include:
- Stress
- Alcohol
- Smoking
Thus, the keys here are to 1) not smoke 2) not drink, ideally, or at least keep consumption low, but honestly even one drink will elevate cortisol levels, so it’s better not to, and 3) manage stress.
See also: Lower Your Cortisol! (Here’s Why & How)
Other modifiable factors
Being aware of infection risk and taking steps to reduce it (e.g. avoiding being with many people in confined indoor places, masking as appropriate, handwashing frequently) is a good preventative strategy, along with of course getting any recommended vaccines as they come available.
What if they fail? How can we boost the immune system?
We talked about not sabotaging the immune system, but what about actively boosting it? The answer is yes, we certainly can (barring serious medical reasons why not), as there are some very important lifestyle factors too:
Beyond Supplements: The Real Immune-Boosters!
One final last-line thing…
Since if we do get an infection, it’s better to know sooner rather than later… A recent study shows that wearable activity trackers can (if we pay attention to the right things) help predict disease, including highlighting COVID status (positive or negative) about as accurately (88% accuracy) as rapid screening tests. Here’s a pop-science article about it:
Wearable activity trackers show promise in detecting early signals of disease
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From immunotherapy to mRNA vaccines – the latest science on melanoma treatment explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More than 16,000 Australians will be diagnosed with melanoma each year. Most of these will be caught early, and can be cured by surgery.
However, for patients with advanced or metastatic melanoma, which has spread from the skin to other organs, the outlook was bleak until the advent of targeted therapies (that attack specific cancer traits) and immune therapies (that leverage the immune system). Over the past decade, these treatments have seen a significant climb in the number of advanced melanoma patients surviving for at least five years after diagnosis, from less than 10% in 2011 to around 50% in 2021.
While this is great news, there are still many melanoma patients who cannot be treated effectively with current therapies. Researchers have developed two exciting new therapies that are being evaluated in clinical trials for advanced melanoma patients. Both involve the use of immunotherapy at different times and in different ways.
The first results from these trials are now being shared publicly, offering insight into the future of melanoma treatment.
Svitlana Hulko/Shutterstock Immunotherapy before surgery
Immunotherapy works by boosting the power of a patient’s immune system to help kill cancer cells. One type of immunotherapy uses something called “immune checkpoint inhibitors”.
Immune cells carry “immune checkpoint” proteins, which control their activity. Cancer cells can interact with these checkpoints to turn off immune cells and hide from the immune system. Immune checkpoint inhibitors block this interaction and help keep the immune system activated to fight the cancer.
Results from an ongoing phase 3 trial using immune checkpoint inhibitors were recently published in the New England Journal of Medicine.
This trial used two types of immune checkpoint inhibitors: nivolumab, which blocks an immune checkpoint called PD-1, and ipilimumab, which blocks CTLA-4.
More than 16,000 Australians are diagnosed with melanoma each year. Delovely Pics/Shutterstock Some 423 patients (including many from Australia) were enrolled in the trial, and participants were randomly assigned to one of two groups.
The first group had surgery to remove their melanoma, and were then given immunotherapy (nivolumab) to help kill any remaining cancer cells. Giving a systemic (whole body) therapy such as immunotherapy after surgery is a standard way of treating melanoma. The second group received immunotherapy first (nivolumab plus ipilimumab) and then underwent surgery. This is a new approach to treating these cancers.
Based on previous observations, the researchers had predicted that giving patients immunotherapy while the whole tumour was still present would activate the tumour-fighting abilities of the patient’s immune system much better than giving it once the tumour had been removed.
Sure enough, 12 months after starting therapy, 83.7% of patients who received immunotherapy before surgery remained cancer-free, compared to 57.2% in the control group who received immunotherapy after surgery.
Based on these results, Australian of the year Georgina Long – who co-led the trial with Christian Blank from The Netherlands Cancer Institute – has suggested this method of immunotherapy before surgery should be considered a new standard of treatment for higher risk stage 3 melanoma. She also said a similar strategy should be evaluated for other cancers.
The promising results of this phase 3 trial suggest we might see this combination treatment being used in Australian hospitals within the next few years.
mRNA vaccines
Another emerging form of melanoma therapy is the post-surgery combination of a different checkpoint inhibitor (pembrolizumab, which blocks PD-1), with a messenger RNA vaccine (mRNA-4157).
While checkpoint inhibitors like pembrolizumab have been around for more than a decade, mRNA vaccines like mRNA-4157 are a newer phenomenon. You might be familiar with mRNA vaccines though, as the biotechnology companies Pfizer-BioNTech and Moderna released COVID vaccines based on mRNA technology.
mRNA-4157 works basically the same way – the mRNA is injected into the patient and produces antigens, which are small proteins that train the body’s immune system to attack a disease (in this case, cancer, and for COVID, the virus).
However, mRNA-4157 is unique – literally. It’s a type of personalised medicine, where the mRNA is created specifically to match a patient’s cancer. First, the patient’s tumour is genetically sequenced to figure out what antigens will best help the immune system to recognise their cancer. Then a patient-specific version of mRNA-4157 is created that produces those antigens.
The latest results of a three-year, phase 2 clinical trial which combined pembrolizumab and mRNA-4157 were announced this past week. Overall, 2.5 years after starting the trial, 74.8% of patients treated with immunotherapy combined with mRNA-4157 post-surgery remained cancer-free, compared to 55.6% of those treated with immunotherapy alone. These were patients who were suffering from high-risk, late-stage forms of melanoma, who generally have poor outcomes.
It’s worth noting these results have not yet been published in peer-reviewed journals. They’re available as company announcements, and were also presented at some cancer conferences in the United States.
Based on the results of this trial, the combination of pembrolizumab and the vaccine progressed to a phase 3 trial in 2023, with the first patients being enrolled in Australia. But the final results of this trial are not expected until 2029.
It is hoped this mRNA-based anti-cancer vaccine will blaze a trail for vaccines targeting other types of cancer, not just melanoma, particularly in combination with checkpoint inhibitors to help stimulate the immune system.
Despite these ongoing advances in melanoma treatment, the best way to fight cancer is still prevention which, in the case of melanoma, means protecting yourself from UV exposure wherever possible.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research) and John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Goji Berries: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are Goji Berries Really A Superfood?
Goji berries are popularly considered a superfood, and sold for everything from anti-aging effects, to exciting benefits* that would get this email directed to your spam folder if we described them.
*We searched so you don’t have to: there doesn’t seem to be much research to back [that claim that we can’t mention], but we did find one paper on its “invigorating” benefits for elderly male rats. We prefer to stick to human studies where we can!
So how does the science stack up for the more mainstream claims?
Antioxidant effects
First and most obvious for this fruit that’s full of helpful polysaccharides, carotenoids, phenolic acids, and flavonoids, yes, they really do have strong antioxidant properties:
Immune benefits
Things that are antioxidant are generally also anti-inflammatory, and often have knock-on benefits for the immune system. That appears to be the case here.
For example, in this small-but-statistically-significant study (n=60) in healthy adults (aged 55–72 years)
❝The GoChi group showed a statistically significant increase in the number of lymphocytes and levels of interleukin-2 and immunoglobulin G compared to pre-intervention and the placebo group, whereas the number of CD4, CD8, and natural killer cells or levels of interleukin-4 and immunoglobulin A were not significantly altered. The placebo group showed no significant changes in any immune measures.
Whereas the GoChi group showed a significant increase in general feelings of well-being, such as fatigue and sleep, and showed a tendency for increased short-term memory and focus between pre- and post-intervention, the placebo group showed no significant positive changes in these measures.❞
“GoChi” here is a brand name for goji berries, and it’s not clear from the abstract whether the company funded the study:
Here’s another study, this time n=150, and ages 65–70 years old. This time it’s with a different brand (“Lacto-Wolfberry”, a milk-with-goji supplement drink) and it’s also unclear whether the company funded the study. However, taking the data at face value:
❝In conclusion, long-term dietary supplementation with Lacto-Wolfberry in elderly subjects enhances their capacity to respond to antigenic challenge without overaffecting their immune system, supporting a contribution to reinforcing immune defense in this population. ❞
In other words: it allowed those who took it to get measurably more benefit from the flu vaccinations that they received, without any ill effects.
Anticancer potential
This one’s less contentious (the immune benefits seemed very credible; we’d just like to see more transparent research to say for sure), so in the more clearly-evidenced case against cancer we’ll just drop a few quick studies, clipped for brevity:
- Goji berry (Lycium barbarum) inhibits the proliferation, adhesion, and migration of oral cancer cells
- A closer look at immunomodulatory properties of goji berries extract in human colon cancer cells
- Lycium barbarum polysaccharides induce apoptosis in human prostate cancer cells and inhibits prostate cancer growth
- Identification of goji berry cyclic peptides and anticervical carcinoma activity
- Antiproliferative effects of Lycium barbarum’s (goji berry) fractions on breast cancer Cell Lines
You get the idea: it helps!
Bonus benefit for the eyes
Goji berries also help against age-related macular degeneration. The research for this is in large part secondary, i.e. goji berries contain things x, y, and z, and then separate studies say that those things help against age-related macular degeneration.
We did find some goji-specific studies though! One of them was for our old friends the “Lacto-Wolfberry” people and again, wasn’t very transparent, so we’ll not take up extra time/space with that one here.
Instead, here’s a much clearer, transparent, and well-referenced study with no conflicts of interest, that found:
❝Overall, daily supplementation with Goji berry for 90d improves MPOD by increasing serum Z levels rather than serum L levels in early AMD patients. Goji berry may be an effective therapeutic intervention for preventing the progression of early AMD.❞
- MPOD = Macular Pigment Optical Density, a standard diagnostic tool for age-related macular degeneration
- AMD = Age-related Macular Degeneration
(that whole paper is very compelling reading, if you have time)
If you want a quicker read, we offer:
How To Avoid Age-Related Macular Degeneration
and also…
Where to get goji berries?
You can probably find them at your local health food store, if not the supermarket. However, if you’d like to buy them online, here’s an example product on Amazon for your convenience
Enjoy!
Share This Post
-
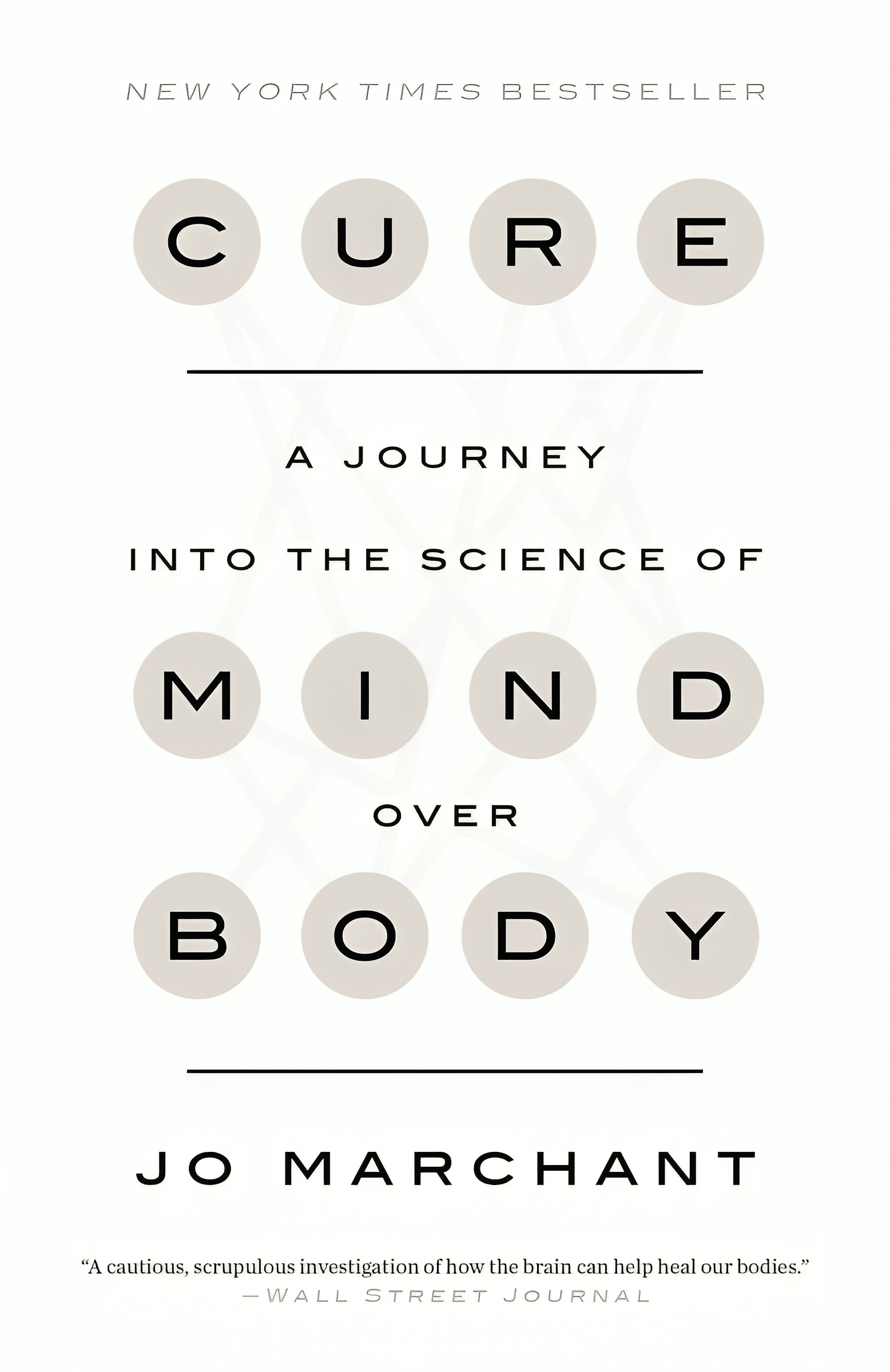
Cure – by Dr. Jo Marchant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here, “a journey into the science of mind over body”, prompts an immediate question: is this book actually about science?
And yes, yes it is. It’s not about “positive energy” or “tapping into your divine essence” or anysuch. It’s about science, and scientific studies.
The author’s PhD is in genetics and medical microbiology, not metaphysics or something.
For those of us who read a lot of clinical studies about a lot of things (hi, regular researcher/writer here), we’re very used to placebo being used as a control in medical science.
“This drug performed no better than placebo” is generally considered a disappointing statement… But what if the placebo was already having a profound effect? Shouldn’t that be worthy of note too?
Dr. Marchant looks at more than just drugs, though, and also looks into the science (complete with EEGs and such) of hypnosis and virtual reality.
The writing style here is very accessible without skimping on science. This is to be expected; Dr. Marchant also has an MSc in science communication, and spent a time as senior editor of New Scientist magazine.
This isn’t a how-to book, but there are some practical takeaways too, specific things we can do to augment (or avoid sabotaging) any medications we take, for example.
Bottom line: placebo effect (and its evil twin, the nocebo effect) has a profound impact on all of us whether we want it or not, so we might as well learn about how it works and how to leverage it. This book gives a very good, hard science grounding.
Click here to check out “Cure” and get the most out of whatever you take (or do) for your health!
Share This Post
Related Posts
-
What the Health – by Kip Andersen, Keegan Kuhn, & Eunice Wong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book from the makers of the famous documentary of the same name. Which means that yes, they are journalists not scientists, but they got input from very many scientists, doctors, nutritionists, and so forth, for a very reliable result.
It’s worth noting however that while a lot of the book is about the health hazards of a lot of the “Standard American Diet”, or “SAD” as it is appropriately abbreviated, a lot is also about how various industries
bribelobby the government to either push, or give them leeway to push, their products over healthier ones. So, there’s a lot about what would amount to corruption if it weren’t tied up in legalese that makes it just “lobbying” rather than bribery.The style is mostly narrative, albeit with very many citations adding up to 50 pages of references. There’s also a recipe section, which is… fairly basic, and despite getting a shoutout in the subtitle, the recipes are certainly not the real meat of the book.
The recipes themselves are entirely plant-based, and de facto vegan.
Bottom line: this one’s more of a polemic against industry malfeasance than it is a textbook of nutrition science, but there is enough information in here that it could have been the textbook if it wanted to, changing only the style and not the content.
Click here to check out What The Health, and make informed choices about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Black Forest Chia Pudding
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This pudding tastes so decadent, it’s hard to believe it’s so healthy, but it is! Not only is it delicious, it’s also packed with nutrients including protein, carbohydrates, healthy fats (including omega-3s), fiber, vitamins, minerals, and assorted antioxidant polyphenols. Perfect dessert or breakfast!
You will need
- 1½ cups pitted fresh or thawed-from-frozen cherries
- ½ cup mashed banana
- 3 tbsp unsweetened cocoa powder
- 2 tbsp chia seeds, ground
- Optional: 2 pitted dates, soaked in hot water for 10 minutes and then drained (include these if you prefer a sweeter pudding)
- Garnish: a few almonds, and/or berries, and/or cherries and/or cacao nibs
Method
(we suggest you read everything at least once before doing anything)
1) Blend the ingredients except for the chia seeds and the garnish, with ½ cup of water, until completely smooth
2) Divide into two small bowls or glass jars
3) Add 1 tbsp ground chia seeds to each, and stir until evenly distributed
4) Add the garnish and refrigerate overnight or at least for some hours. There’s plenty of wiggle-room here, so make it at your convenience and serve at your leisure.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Cherries’ Very Healthy Wealth Of Benefits!
- If You’re Not Taking Chia, You’re Missing Out
- Cacao vs Carob – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When And Why Do We Pick Up Our Phones?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The School of Life’s Alain de Botton makes the argument that—if we pay attention, if we keep track—there’s an understory to why we pick up our phones:
It’s not about information
Yes, our phones (or rather, the apps therein) are designed to addict us, to draw us back, to keep us scrolling and never let us go. We indeed seek out information like our ancestors once sought out berries; searching, encouraged by a small discovery, looking for more. The neurochemistry is similar.
But when we look at the “when” of picking up our phones, de Botton says, it tells a different story:
We pick them up not to find out what’s going on with the world, but rather specifically to not find out what’s going with ourselves. We pick them up to white out some anxiety we don’t want to examine, a line of thought we don’t want to go down, memories we don’t want to consider, futures we do not want to have to worry about.
And of course, phones do have a great educational potential, are an immensely powerful tool for accessing knowledge of many kinds—if only we can remain truly conscious while using them, and not take them as the new “opiate of the masses”.
De Botton bids us, when next we pick up our phone. ask a brave question:
“If I weren’t allowed to consult my phone right now, what might I need to think about?”
As for where from there? There’s more in the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Making Social Media Work For Your Mental Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: