Hydroxyapatite Toothpaste – 6 Month Update
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A dental hygienist tried hydroxyapatite toothpaste for 6 months, and this is what she found:
The results are in
In few words: she took before-and-after photos, or rather, regular photos through the 6-month process.
What she was mostly looking for: tooth translucency, enamel imperfections, and stains.
What she found: a slight improvement within two months, though over the course of the six months, the photos were somewhat inconsistent—however, this may have more to do with the machinations of her camera, the ambient lighting, etc, than it has to do with the toothpaste. In an ideal world, she’d be able to do a density test with a laser on one side and a sensor on the other, but it seems her budget didn’t stretch to that. In terms of subjective improvement, she found that her teeth felt better, even if the visual change was not consistently apparent.
This is consistent with the idea that hydroxyapatite toothpaste can mineralize teeth throughout the tooth, not just from the outside in, due to the porous nature of the enamel. So, a lot of the change may have been on the inside.
Ultimately, she neither recommends nor discommends the toothpaste, and acknowledges that more time, up to a year, may be needed for more noticeable results.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Tooth Remineralization: How To Heal Your Teeth Naturally
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Mind-Gut Connection – by Dr. Emeran Mayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the mind-gut connection before, so what makes this one stand out?
Firstly, it’s a lot more comprehensive than the usual “please, we’re begging you, eat some fiber”.
And yes, of course that’s part of it. Prebiotics, probiotics, reduce fried and processed foods, reduce sugar/alcohol, reduce meat, and again, eat some greenery.
But where this book really comes into its own is looking more thoroughly at the gut microbiota and their function. Dr. Mayer goes well beyond “there are good and bad bacteria” and looks at the relationship each of them have with the body’s many hormones, and especially neurotransmitters like serotonin and dopamine.
He also looks at the two-way connection between brain and gut. Yes, our gut gives us “gut feelings”, but 10% of communication between the brain and gut is in the other direction; he explores what that means for us, too.
Finally, he does give a lot of practical advice, not just dietary but also behavioral, to make the most of our mind-gut connection and make it work for our health, rather than against it.
Bottom line: this is the best book on the brain-gut connection that this reviewer has read so far, and certainly the most useful if you already know about gut-healthy nutrition, and are looking to take your understanding to the next level.
Click here to check out The Mind-Gut Connection, and start making yours work for your benefit!
Share This Post
-
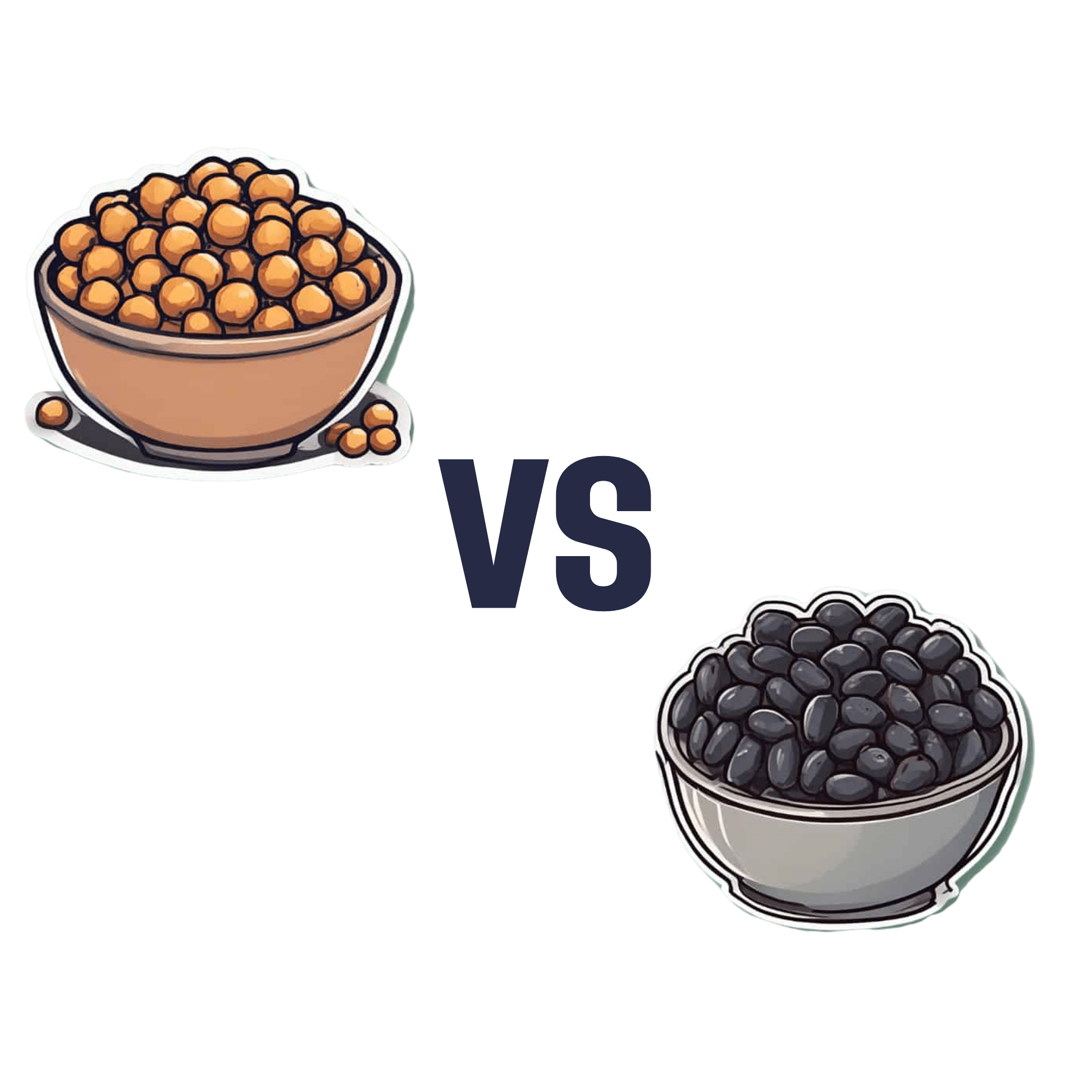
Chickpeas vs Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to black beans, we picked the black beans.
Why?
They’re both great! But we consider the nutritional profile of black beans to be better:
In terms of macros, black beans have a little more protein, while chickpeas have more carbohydrates. Generally speaking, people are not usually short of carbs in their diet, so we’ll go with the one with more protein. Black beans also have more fiber, which is important for heart health and more.
In the category of micronutrients, black beans have twice as much potassium and twice as much calcium, as well as twice as much magnesium. Chickpeas, meanwhile are better for manganese and slightly higher in B vitamins, but B vitamins are everywhere (especially vitamin B5, pantothenic acid; that’s literally where its name comes from, it means “from everywhere”), so we don’t consider that as much of a plus as the black beans doubling up on potassium, calcium, and magnesium.
So, do enjoy both, but if you’re going to pick, or lean more heavily on one, we recommend the black beans
Further reading
See also:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Easily Digestible Vegetarian Protein Sources
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
Enjoy!
Share This Post
-
The Sugar Alcohol That Reduces BMI!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inositol Does-It-Ol’!
First things first, a quick clarification up-front:
Myo-inositol or D-chiro-inositol?
We’re going to be talking about inositol today, which comes in numerous forms, but most importantly:
- Myo-inositol (myo-Ins)
- D-chiro-inositol (D-chiro-Ins)
These are both inositol, (a sugar alcohol!) and for our purposes today, the most relevant form is myo-inositol.
The studies we’ll look at today are either:
- just about myo-inositol, or
- about myo-inositol in the presence of d-chiro-inositol at a 40:1 ratio.
You have both in your body naturally; wherever supplementation is mentioned, it means supplementing with either:
- extra myo-inositol (because that’s the one the body more often needs more of), or
- both, at the 40:1 ratio that we mentioned above (because that’s one way to help balance an imbalanced ratio)
With that in mind…
Inositol against diabetes?
Inositol is known to:
- decrease insulin resistance
- increase insulin sensitivity
- have an important role in cell signaling
- have an important role in metabolism
The first two things there both mean that inositol is good against diabetes. It’s not “take this and you’re cured”, but:
- if you’re pre-diabetic it may help you avoid type 2 diabetes
- if you are diabetic (either type) it can help in the management of your diabetes.
It does this by allowing your body to make better use of insulin (regardless of whether that insulin is from your pancreas or from the pharmacy).
How does it do that? Research is still underway and there’s a lot we don’t know yet, but here’s one way, for example:
❝Evidence showed that inositol phosphates might enhance the browning of white adipocytes and directly improve insulin sensitivity through adipocytes❞
Read: Role of Inositols and Inositol Phosphates in Energy Metabolism
We mentioned its role in metabolism in a bullet-point above, and we didn’t just mean insulin sensitivity! There’s also…
Inositol for thyroid function?
The thyroid is one of the largest endocrine glands in the body, and it controls how quickly the body burns energy, makes proteins, and how sensitive the body should be to other hormones. So, it working correctly or not can have a big impact on everything from your mood to your weight to your energy levels.
How does inositol affect thyroid function?
- Inositol has an important role in thyroid function and dealing with autoimmune diseases.
- Inositol is essential to produce H2O2 (yes, really) required for the synthesis of thyroid hormones.
- Depletion of inositol may lead to the development of some thyroid diseases, such as hypothyroidism.
- Inositol supplementation seems to help in the management of thyroid diseases.
Read: The Role of Inositol in Thyroid Physiology and in Subclinical Hypothyroidism Management
Inositol for PCOS?
A systematic review published in the Journal of Gynecological Endocrinology noted:
- Inositol can restore spontaneous ovarian activity (and consequently fertility) in most patients with PCOS.
- Myo-inositol is a safe and effective treatment to improve:
- ovarian function
- healthy metabolism
- healthy hormonal balance
While very comprehensive (which is why we included it here), that review’s a little old, so…
Check out this cutting edge (Jan 2023) study whose title says it all:
Inositol for fertility?
Just last year, Mendoza et al published that inositol supplementation, together with antioxidants, vitamins, and minerals, could be an optimal strategy to improve female fertility.
This built from Gambiole and Forte’s work, which laid out how inositol is a safe compound for many issues related to fertility and pregnancy. In particular, several clinical trials demonstrated that:
- inositol can have therapeutic effects in infertile women
- inositol can also be useful as a preventive treatment during pregnancy
- inositol could prevent the onset of neural tube defects
- inositol also reduces the occurrence of gestational diabetes
Due to the safety and efficiency of inositol, it can take the place of many drugs that are contraindicated in pregnancy. Basically: take this, and you’ll need fewer other drugs. Always a win!
Read: Myo-Inositol as a Key Supporter of Fertility and Physiological Gestation
Inositol For Weight Loss
We promised you “this alcohol sugar can reduce your BMI”, and we weren’t making it up!
Zarezadeh et al conducited a very extensive systematic review, and found:
- Oral inositol supplementation has positive effect on BMI reduction.
- Inositol in the form of myo-inositol had the strongest effect on BMI reduction.
- Participants with PCOS and/or who were overweight, experienced the most significant improvement of all.
Want some inositol?
As ever, we don’t sell it (or anything else), but for your convenience, here’s myo-inositol and d-chiro-inositol at a 40:1 ratio, available on Amazon!
Share This Post
Related Posts
-
Pomegranate vs Apricot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to apricot, we picked the pomegranate.
Why?
Both are great! Top tier fruits. But ultimately, pomegranate does have more to offer:
In terms of macros, pomegranate has more protein, carbs, and fiber (and even a little healthy fat—it’s the seeds); the main deciding factor on macros for fruits is almost always the fiber, and that’s the case here, which is why we hand the win to pomegranates in this category.
In the category of vitamins, pomegranates have more of vitamins B1, B2, b5, B6, B7, B9, K, and choline, while apricots have more of vitamins A, B3, and E. A clear win for pomegranates here.
When it comes to minerals, pomegranate has more copper, calcium, magnesium, manganese, phosphorus, selenium, and zinc, while apricots boast just a little more calcium and iron. Another easy win for pomegranates.
Looking at polyphenols, apricots finally win a category, with greater overall polyphenol coverage.
Which is good, but not enough to overcome the other three categories all being in pomegranates’ favor—hence the overall win for pomegranates here!
Of course, the solution is to enjoy both! Diversity is good, for exactly such reasons as this.
Want to learn more?
You might like to read:
Pomegranate’s Health Gifts Are Mostly In Its Peel ← in other words, the one part of the fruit you don’t normally eat. However! It can be dried and ground into a powder supplement, or else made in pomegranate tea.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When And Why Do We Pick Up Our Phones?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The School of Life’s Alain de Botton makes the argument that—if we pay attention, if we keep track—there’s an understory to why we pick up our phones:
It’s not about information
Yes, our phones (or rather, the apps therein) are designed to addict us, to draw us back, to keep us scrolling and never let us go. We indeed seek out information like our ancestors once sought out berries; searching, encouraged by a small discovery, looking for more. The neurochemistry is similar.
But when we look at the “when” of picking up our phones, de Botton says, it tells a different story:
We pick them up not to find out what’s going on with the world, but rather specifically to not find out what’s going with ourselves. We pick them up to white out some anxiety we don’t want to examine, a line of thought we don’t want to go down, memories we don’t want to consider, futures we do not want to have to worry about.
And of course, phones do have a great educational potential, are an immensely powerful tool for accessing knowledge of many kinds—if only we can remain truly conscious while using them, and not take them as the new “opiate of the masses”.
De Botton bids us, when next we pick up our phone. ask a brave question:
“If I weren’t allowed to consult my phone right now, what might I need to think about?”
As for where from there? There’s more in the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Making Social Media Work For Your Mental Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Golden Rules To Lose Belly Fat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our belly is often the first place we gain fat and the last to lose it—due to hormonal changes, poor blood flow, and fat cell types. This also means that weight loss efforts can result in it looking worse before it looks better, as we lose weight from elsewhere around it. But, there is a way forwards:
What to do about it
Cori Lefkowith, of “Redefining Strength” and “Strength At Any Age” fame, advise that we follow the following “5 golden rules”:
- Mindset: avoid “All or Nothing” thinking; focus on small, sustainable changes and consistent habits.
- Macros: prioritize protein (40%+ of calories), balance fats and carbs for hormonal health, and avoid extreme calorie deficits (your body will try to save you from starvation by slowing your metabolism to conserve energy, and storing fat).
- Nutrition quality: focus on whole, nutrient-dense foods for better satiety, gut health, and energy. Get plenty of fiber and water; your body still needs those too.
- Muscle building: strength training preserves muscle, boosts metabolism, and improves body composition—don’t ditch your strength training for cardio; it won’t help and that swap would hinder..
- Daily walks: 15–20 minutes of walking after dinner aids digestion, and reduces stress (remember: stress invites your body to store extra fat, especially at the belly). It also incidentally burns calories without stressing the body, but honestly, it’s really not very many calories, so that’s not the main reason to do it.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It ← this is not the same thing as subcutaneous fat; the remedy is partly the same though, and it’s important to do both if you’re carrying excess weight both on your belly and in your viscera, if you want to reduce your overall waist size.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: