The Mind-Gut Connection – by Dr. Emeran Mayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the mind-gut connection before, so what makes this one stand out?
Firstly, it’s a lot more comprehensive than the usual “please, we’re begging you, eat some fiber”.
And yes, of course that’s part of it. Prebiotics, probiotics, reduce fried and processed foods, reduce sugar/alcohol, reduce meat, and again, eat some greenery.
But where this book really comes into its own is looking more thoroughly at the gut microbiota and their function. Dr. Mayer goes well beyond “there are good and bad bacteria” and looks at the relationship each of them have with the body’s many hormones, and especially neurotransmitters like serotonin and dopamine.
He also looks at the two-way connection between brain and gut. Yes, our gut gives us “gut feelings”, but 10% of communication between the brain and gut is in the other direction; he explores what that means for us, too.
Finally, he does give a lot of practical advice, not just dietary but also behavioral, to make the most of our mind-gut connection and make it work for our health, rather than against it.
Bottom line: this is the best book on the brain-gut connection that this reviewer has read so far, and certainly the most useful if you already know about gut-healthy nutrition, and are looking to take your understanding to the next level.
Click here to check out The Mind-Gut Connection, and start making yours work for your benefit!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not Fantastic To Be Plastic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We Are Such Stuff As Bottles Are Made Of
We’ve written before about PFAS, often found in non-stick coatings and the like:
PFAS Exposure & Cancer: The Numbers Are High
Today we’re going to be talking about microplastics & nanoplastics!
What are microplastics and nanoplastics?
Firstly, they’renot just the now-banned plastic microbeads that have seen some use is toiletries (although those are classified as microplastics too).
Many are much smaller than that, and if they get smaller than a thousandth of a millimeter, then they get the additional classification of “nanoplastic”.
In other words: not something that can be filtered even if you were to use a single-micron filter. The microplastics would still get through, for example:
Scientists find about a quarter million invisible nanoplastic particles in a liter of bottled water
And unfortunately, that’s bad:
❝What’s disturbing is that small particles can appear in different organs and may cross membranes that they aren’t meant to cross, such as the blood-brain barrier❞
Note: they’re crossing the same blood-brain barrier that many of our nutrients and neurochemicals are too big to cross.
These microplastics are also being found in arterial plaque
What makes arterial plaque bad for the health is precisely its plasticity (the arterial walls themselves are elastic), so you most certainly do not want actual plastic being used as part of the cement that shouldn’t even be lining your arteries in the first place:
Microplastics found in artery plaque linked with higher risk of heart attack, stroke and death
❝In this study, patients with carotid artery plaque in which MNPs were detected had a higher risk of a composite of myocardial infarction, stroke, or death from any cause at 34 months of follow-up than those in whom MNPs were not detected❞
~ Dr. Raffaele Marfella et al.
(MNP = Micro/Nanoplastics)
Source: Microplastics and Nanoplastics in Atheromas and Cardiovascular Events
We don’t know how bad this is yet
There are various ways this might not be as bad as it looks (the results may not be repeated, the samples could have been compromised, etc), but also, perhaps cynically but nevertheless honestly, it could also be worse than we know yet—only more experiments being done will tell us which.
In the meantime, here’s a rundown of what we do and don’t know:
Study links microplastics with human health problems—but there’s still a lot we don’t know
Take care!
Share This Post
-
The New Menopause – by Dr. Mary Claire Haver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is most famous for “The Galveston Diet”, which book is astonishingly similar in its content, chapters, format, etc to Nikki Williams’ “It’s Not You, It’s Your Hormones” which came out a few years previously but didn’t get the same marketing.
Nonetheless, this time Dr. Haver has something new to add, and we think it’s worth a read.
The general theme of this book is a comprehensive overview of the menopause, experientially (subjective to the person going through it) and empirically (by science), from start to finish and beyond. This book’s more about human physiology, and less about diet than the previous.
Dr. Haver also discusses in-depth how estrogen is thought of as a sex hormone (and it is), to the point that people consider it perhaps expendable, and forget (or are simply unaware) that we have estrogen receptors throughout our bodies and estrogen is vital for maintaining many other bodily functions, including your heart, cognitive function, bone integrity, blood sugar balance, and more.
(in case you’re wondering “why don’t men fall to bits, then?”, don’t worry, their testosterone does these things for them. Testosterone is orders of magnitude less potent than estrogen, mg for mg, so they need a lot more of it, but under good conditions they produce plenty so it’s fine)
But, the amount of testosterone available to peri/postmenopausal women is simply not enough to do that job (and it’d also result in a transition of secondary sex characteristics, which for most people would be very unwanted), so, something else needs to be done.
Dr. Haver also discusses in detail the benefits and risks of HRT and how to get/manage them, respectively, with the latest up-to-date research (at time of going to print; the book was published in April 2024).
Bottom line: if you want to know what’s going on with your peri- or post-menopausal body and how it could be better (or if you want to know what’s going on with someone else approaching/experiencing menopause), then this is a top-tier book.
Click here to check out The New Menopause, and know what’s going on and what to do about it!
Share This Post
-
Zero Sugar / One Month – by Becky Gillaspy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the evils of sugar before, so what makes this one different?
This one has a focus on helping the reader quit it. It assumes we already know the evils of sugar (though it does cover that too).
It looks at the mechanisms of sugar addiction (habits-based and physiological), and how to safely and painlessly cut through those to come out the other side, free from sugar.
The author gives a day-by-day plan, for not only eliminating sugar, but also adding and including things to fill the gap it leaves, keeping us sated, energized, and happy along the way.
In the category of subjective criticism, it does also assume we want to lose weight, which may not be the case for many readers. But that’s a by-the-by and doesn’t detract from the useful guide to quitting sugar, whatever one’s reasons.
Bottom line: if you would like to quit sugar but find it hard, this book thinks of everything and walks you by the hand, making it easy.
Click here to check out Zero Sugar / One Month, and reap the health benefits!
Share This Post
Related Posts
-
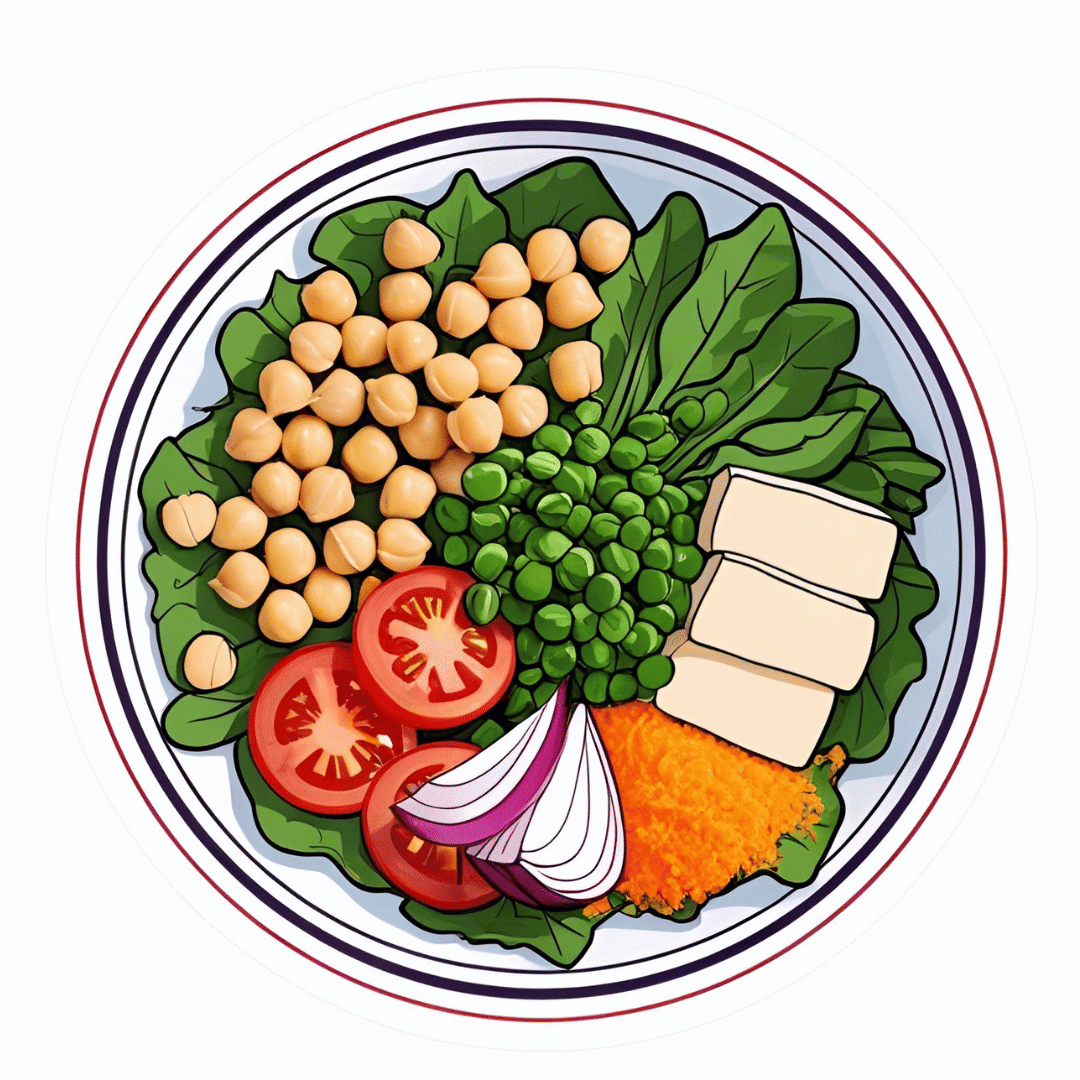
The High-Protein, High-Fiber Superfood Salad You’ll Want To Enjoy Daily
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This salad from Nisha Vora at Rainbow Plant Life has 30g protein and takes minutes to prepare, while being tasty enough to look forward to eating each day:
Easy preparation
Prepare the toppings first; you can do a week’s in advance at once:
- Roasted chickpeas:
- Drain, rinse, and dry two cans of chickpeas.
- Toss with olive oil, salt, and pepper.
- Roast at 425°F for 30–35 minutes.
- Roasted walnuts:
- Chop and toss with olive oil, salt, and pepper.
- Roast at 350°F for 12 minutes after chickpeas finish.
As for the salad base:
- Kale:
- Remove tough stems, slice thinly.
- Wash and massage with lemon juice and salt to soften.
- Cabbage:
- Slice thinly with a knife or mandolin.
- Store in a sealed bag in the fridge for up to a week.
Red wine vinaigrette dressing:
- Key ingredients: red wine vinegar, lemon juice, red pepper flakes, garlic, olive oil.
- Can be stored in the fridge for up to 10 days.
Putting it all together:
- Toss kale and cabbage with vinaigrette by hand.
- Add roasted chickpeas and walnuts for crunch.
- Include a protein source like tofu (store-bought curry tofu recommended).
- Mix in fresh vegetables like grated carrots, sliced bell peppers, or beets.
- Add extras like sauerkraut, avocado, pickled onions, and such.
- Top with fresh herbs (she recommends parsley, basil, or dill).
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
21 Most Beneficial Polyphenols & What Foods Have Them
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Roasted chickpeas:
-
Do We Need Supplements, And Do They Work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does our diet need a little help?
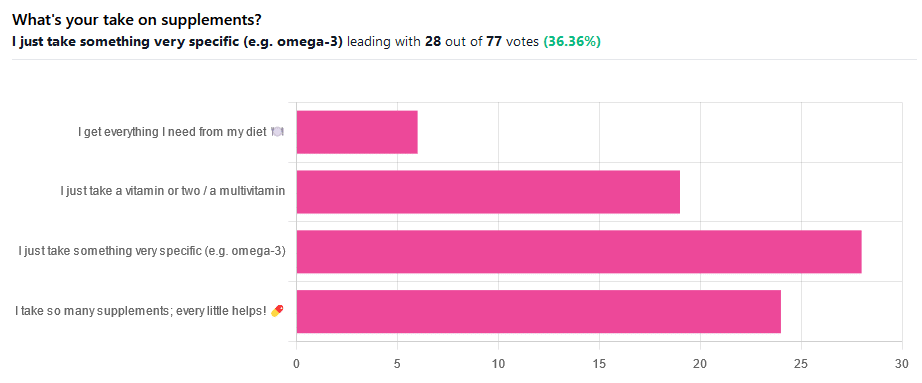
We asked you for your take on supplements, and got the above-illustrated, below-described set of results.
- The largest minority of respondents (a little over a third) voted for “I just take something very specific”
- The next most respondents voted for “I take so many supplements; every little helps!”
- Almost as many voted for “I just take a vitamin or two / a multivitamin”
- Fewest, about 8%, voted for “I get everything I need from my diet”
But what does the science say?
Food is less nutritious now than it used to be: True or False?
True or False depending on how you measure it.
An apple today and an apple from a hundred years ago are likely to contain the same amounts of micronutrients per apple, but a lower percentage of micronutrients per 100g of apple.
The reason for this is that apples (and many other food products; apples are just an arbitrary example) have been selectively bred (and in some cases, modified) for size, and because the soil mineral density has remained the same, the micronutrients per apple have not increased commensurate to the increase in carbohydrate weight and/or water weight. Thus, the resultant percentage will be lower, despite the quantity remaining the same.
We’re going to share some science on this, and/but would like to forewarn readers that the language of this paper is a bit biased, as it looks to “debunk” claims of nutritional values dropping while skimming over “yes, they really have dropped percentage-wise” in favor of “but look, the discrete mass values are still the same, so that’s just a mathematical illusion”.
The reality is, it’s no more a mathematical illusion than is the converse standpoint of saying the nutritional value is the same, despite the per-100g values dropping. After all, sometimes we eat an apple as-is; sometimes we buy a bag of frozen chopped fruit. That 500g bag of chopped fruit is going to contain less copper (for example) than one from decades past.
Here’s the paper, and you’ll see what we mean:
Supplements aren’t absorbed properly and thus are a waste of money: True or False?
True or False depending on the supplement (and your body, and the rest of your diet)
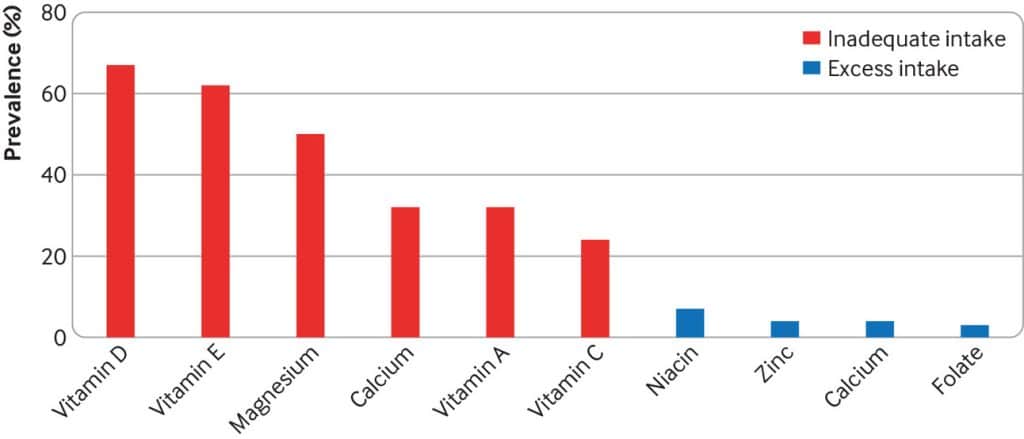
Many people are suffering from dietary deficiencies of vitamins and minerals, that could be easily correctable by supplementation:
However, as this study by Dr. Fang Fang Zhang shows, a lot of vitamin and mineral supplementation does not appear to have much of an effect on actual health outcomes, vis-à-vis specific diseases. She looks at:
- Cardiovascular disease
- Cancer
- Type 2 diabetes
- Osteoporosis
Her key take-aways from this study were:
- Randomised trial evidence does not support use of vitamin, mineral, and fish oil supplements to reduce the risk of non-communicable diseases
- People using supplements tend to be older, female, and have higher education, income, and healthier lifestyles than people who do not use them
- Use of supplements appreciably reduces the prevalence of inadequate intake for most nutrients but also increases the prevalence of excess intake for some nutrients
- Further research is needed to assess the long term effects of supplements on the health of the general population and in individuals with specific nutritional needs, including those from low and middle income countries
Read her damning report: Health effects of vitamin and mineral supplements
On the other hand…
This is almost entirely about blanket vitamin-and-mineral supplementation. With regard to fish oil supplementation, many commercial fish oil supplements break down in the stomach rather than the intestines, and don’t get absorbed well. Additionally, many people take them in forms that aren’t pleasant, and thus result in low adherence (i.e., they nominally take them, but in fact they just sit on the kitchen counter for a year).
One thing we can conclude from this is that it’s good to check the science for any given supplement before taking it, and know what it will and won’t help for. Our “Monday Research Review” editions of 10almonds do this a lot, although we tend to focus on herbal supplements rather than vitamins and minerals.
We can get everything we need from our diet: True or False?
Contingently True (but here be caveats)
In principle, if we eat the recommended guideline amounts of various macro- and micro-nutrients, we will indeed get all that we are generally considered to need. Obviously.
However, this may come with:
- Make sure to get enough protein… Without too much meat, and also without too much carbohydrate, such as from most plant sources of protein
- Make sure to get enough carbohydrates… But only the right kinds, and not too much, nor at the wrong time, and without eating things in the wrong order
- Make sure to get enough healthy fats… Without too much of the unhealthy fats that often exist in the same foods
- Make sure to get the right amount of vitamins and minerals… We hope you have your calculators out to get the delicate balance of calcium, magnesium, potassium, phosphorus, and vitamin D right.
That last one’s a real pain, by the way. Too much or too little of one or another and the whole set start causing problems, and several of them interact with several others, and/or compete for resources, and/or are needed for the others to do their job.
And, that’s hard enough to balance when you’re taking supplements with the mg/µg amount written on them, never mind when you’re juggling cabbages and sardines.
On the topic of those sardines, don’t forget to carefully balance your omega-3, -6, and -9, and even within omega-3, balancing ALA, EPA, and DHA, and we hope you’re juggling those HDL and LDL levels too.
So, when it comes to getting everything we need from our diet, for most of us (who aren’t living in food deserts and/or experiencing food poverty, or having a medical condition that restricts our diet), the biggest task is not “getting enough”, it’s “getting enough of the right things without simultaneously overdoing it on the others”.
With supplements, it’s a lot easier to control what we’re putting in our bodies.
And of course, unless our diet includes things that usually can’t be bought in supermarkets, we’re not going to get the benefits of taking, as a supplement, such things as:
Etc.
So, there definitely are supplements with strong science-backed benefits, that probably can’t be found on your plate!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Working Smarter < Working Brighter!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to working smarter, not harder, there’s plenty of advice and honestly, it’s mostly quite sensible. For example:
(Nice to see they featured a method we talked about last week—great minds!)
But, as standards of productivity rise, the goalposts get moved too, and the treadmill just keeps on going…
- 49% of entrepreneurs say they’ve struggled with some kind of mental illness
- Millennial women are one of the workforce groups at the highest risk of anxiety
- About 7 in 10 millennials experience burnout at work
Not that these things are confined to Millennials, by any stretch, but Millennials make up a huge portion of working people. Ideally, this age group should be able to bring the best of both worlds to the workplace by combining years of experience with youthful energy.
So clearly something is going wrong; the question is: what can be done about it?
Workers of the World, Unwind
A knee-jerk response might be “work to rule”—a tactic long-used by disgruntled exploited workers to do no more than the absolute minimum required to not get fired. And it’s arguably better for them than breaking themselves at work, but that’s not exactly enriching, is it?
This is Brittany Berger, founder of “Work Brighter”.
She’s a content marketing consultant, mental health advocate, and (in her words) a highly ridiculous human who always has a pop culture reference at the ready.
What, besides pop culture references, is she bringing to the table? What is Working Brighter?
❝Working brighter means going beyond generic “work smarter” advice on the internet and personalizing it to work FOR YOU. It means creating your own routines for work, productivity, and self-care.❞
Brittany Berger
Examples of working brighter include…
Asking:
- What would your work involve, if it were more fun?
- How can you make your work more comfortable for you?
- What changes could you make that would make your work more sustainable (i.e., to avoid burnout)?
Remembering:
- Mental health is just health
- Self-care is a “soft skill”
- Rest is work when it’s needed
This is not one of those “what workers really want is not more pay, it’s beanbags” things, by the way (but if you want a beanbag, then by all means, get yourself a beanbag).
It’s about making time to rest, it’s about having the things that make you feel good while you’re working, and making sure you can enjoy working. You’re going to spend a lot of your life doing it; you might as well enjoy it.
❝Nobody goes to their deathbed wishing they’d spent more time at the office❞
Anon
On the contrary, having worked too hard is one of the top reported regrets of the dying!
Article: The Top Five Regrets Of The Dying
And no, they don’t wish they’d “worked smarter, not harder”. They wish (also in the above list, in fact) that they’d had the courage to live a life more true to themselves.
You can do that in your work. Whatever your work is. And if your work doesn’t permit that (be it the evil boss trope, or even that you are the boss and your line of work just doesn’t work that way), time to change that up. Stop focusing on what you can’t do, and look for what you can do.
Spoiler: you can have a blast just trying things out!
That doesn’t mean you should quit your job, or replace your PC with a Playstation, or whatever.
It just means that you deserve comfort and happiness while working, and around your work!
Need a helping hand getting started?
- Create your own self-care plan to avoid burnout
- ⏳ Complete your first “time audit”
- ❣️ Zip through to self-awareness with bullet-journalling
Like A Boss
And pssst, if you’re a business-owner who is thinking “but I have quotas to meet”, your customers are going to love your staff being happier, and will enjoy their interactions with your company much more. Or if your staff aren’t customer-facing, then still, they’ll work better when they enjoy doing it. This isn’t rocket science, but all too many companies give a cursory nod to it before proceeding to ignore it for the rest of the life of the company.
So where do you start, if you’re in those particular shoes?
Read on…
*straightens tie because this is the serious bit* —just kidding, I’m wearing my comfiest dress and fluffy-lined slipper-socks. But that makes this absolutely no less serious:
The Institute for Health and Productivity Management (IHPM) and WorkPlace Wellness Alliance (WPWA) might be a good place to get you on the right track!
❝IHPM/WPWA is a global nonprofit enterprise devoted to establishing the full economic value of employee health as a business asset—a neglected investment in the increased productivity of human capital.
IHPM helps employers identify the full economic cost impact of employee health issues on business performance, design and implement the best programs to reduce this impact by improving functional health and productivity, and measure the success of their efforts in financial terms.❞
The Institute for Health and Productivity Management
They offer courses and consultations, but they also have free downloadables and videos, which are awesome and in many cases may already be enough to seriously improve things for your business already:
Check Out IHPM’s Resources Here!
What can you do to make your working life better for you? We’d love to hear about any changes you make inspired by Brittany’s work—you can always just hit reply, and we’re always glad to hear from you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: