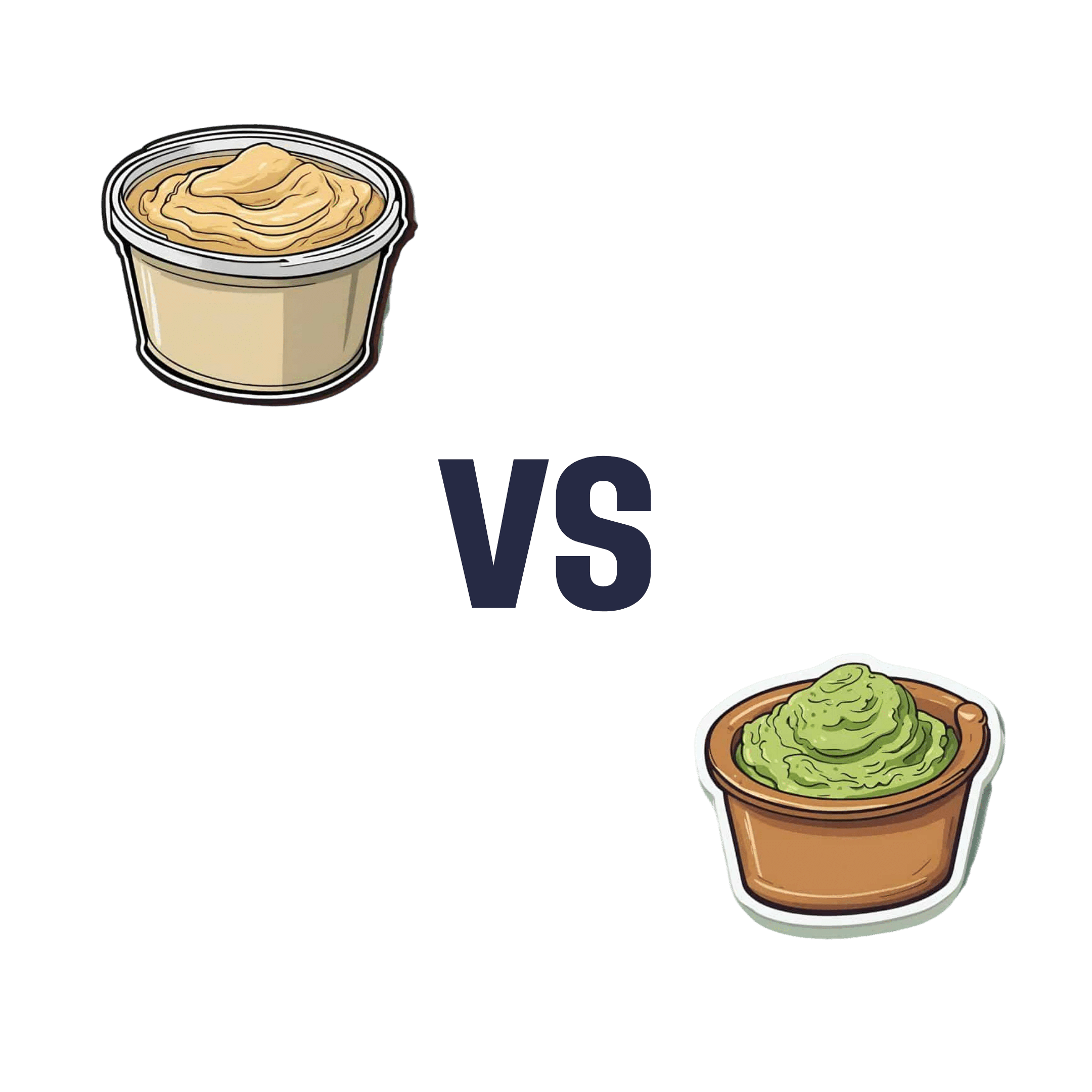
Hummus vs Guacamole – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hummus to guacamole, we picked the guacamole.
Why?
First up, let’s assume that the standards are comparable, for example that both have been made with simple whole foods. The hummus is mostly chickpeas with tahini and a little olive oil and some seasoning; the guacamole is mostly avocado with a little lime juice and some seasoning.
In terms of macronutrients, hummus has slightly more protein and fiber, 2x the carbohydrates (but they are healthy carbs), and usually slightly less fat (but the fats are healthy in both cases).
In terms of micronutrients, the hummus is rich in iron and B vitamins, and the guacamole is rich in potassium, magnesium, vitamins C, E, and K.
So far, it’s pretty much tied. What else is there to consider?
We picked the guacamole because some of its nutrients (especially the potassium, magnesium, and vitamin K) are more common deficiencies in most people’s diets than iron and B vitamins. So, on average, it’s probably the one with the nutrients that you need more of at any given time.
So, it was very very close, and it came down to the above as the deciding factor.
However!
- If you like one and not the other? Eat that one; it’s good.
- If you like both but feel like eating one of them in particular? Eat that one; your body is probably needing those nutrients more right now.
- If you are catering for a group of people? Serve both!
- If you are catering for just yourself and would enjoy both? Serve both! There’s nobody to stop you!
Want to read more?
You might like: Avocado Oil vs Olive Oil – Which is Healthier?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Come As You Are – by Dr. Emily Nagoski
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard the jokes, things like: Q: “Why is the clitoris like Antarctica?” A: “Most men know it’s there; most don’t give a damn”
But… How much do people, in general, really know about the anatomy and physiology of sexual function? Usually very little, but often without knowing how little we know.
This book looks to change that. Geared to a female audience, but almost everyone will gain useful knowledge from this.
The writing style is very easy-to-read, and there are “tl;dr” summaries for those who prefer to skim for relevant information in this rather sizeable (400 pages) tome.
Yes, that’s “what most people don’t know”. Four. Hundred. Pages.
We recommend reading it. You can thank us later!
Share This Post
-
The Plant-Based Athlete – by Matt Frazier and Robert Cheeke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re already a seasoned plant-based athlete yourself, you can probably skip this book; the 60 recipes at the end would still provide value, but there is the “No Meat Athlete Cookbook” that you could hop straight to, in any case.
For most readers, there will be plenty of value from start to finish. We get a quick ground-up tour of nutrition basics, before getting into restructuring diet to optimize it for performance.
There is less in the way of “Vegans struggle with…” and more in the way of “People think vegans struggle with…” and explanations of what vegan athletes actually eat. The book does include science, but isn’t too science-heavy, and relies more on modelling what plant-based superathletes enjoy on a daily basis.
To that end,if the book has a weak point, it’s perhaps that it could have stood to include more science. The book comes recommended by Dr. Michael Greger, whose nutritional approach is incredibly science-heavy and well-referenced, and this book is obviously compatible with that (so they could have!), but in this case Frazier and Cheeke leave us to take their word for it.
Nevertheless, the science is good whether they cite it or not, and this book is quite a comprehensive primer of plant-based athleticism.
Bottom line: if you’re wondering how to optimize the two goals of “eating plants” and “being a powerful athlete”, then this one’s the book for you.
Click here to check out The Plant-Based Athlete and upgrade your health and athletic performance!
Share This Post
-
Palliative care as a true art form
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How do you ease the pain from an ailment amidst lost words? How can you serve the afflicted when lines start to blur? When the foundation of communication begins to crumble, what will be the pillar health-care professionals can lean on to support patients afflicted with dementia during their final days?
The practice of medicine is both highly analytical and evidence based in nature. However, it is considered a “practice” because at the highest level, it resembles a musician navigating an instrument. It resembles art. Between lab values, imaging techniques and treatment options, the nuances for individualized patient care so often become threatened.
Dementia, a non-malignant terminal illness, involves the progressive cognitive and social decline in those afflicted. Though there is no cure, dementia is commonly met in the setting of end-of-life care. During this final stage of life, the importance of comfort via symptomatic management and communication usually is a priority in patient care. But what about the care of a patient suffering from dementia? While communication serves as the vehicle to deliver care at a high level, medical professionals are suddenly met with a roadblock. And there … behind the pieces of shattered communication and a dampened map of ethical guidelines, health-care providers are at a standstill.
It’s 4:37 a.m. You receive a text message from the overnight nurse at a care facility regarding a current seizure. After lorazepam is ordered and administered, Mr. H, a quick-witted 76-year-old, stabilizes. Phenobarbital 15mg SC qhs was also added to prevent future similar events. You exhale a sigh of relief.
Mr. H. has been admitted to the floor 36 hours earlier after having a seizure while playing poker with colleagues. Since he became your patient, he’s shared many stories from professional and family life with you, along with as many jokes as he could fit in between. However, over the course of the next seven days, Mr. H. would develop aspiration pneumonia, progressing to ventilator dependency and, ultimately, multi-organ failure with rapid cognitive decline.
What strategies and tools would you use to maximize the well-being of your patient during his decline? How would you bridge the gap of understanding between the patient’s family and health-care team to provide the standard of care that all patients are owed?
To give Mr. H. the type of care he would have wanted, upon his hospital admission, he should have been questioned about his understanding of illness along with the goals of care of the medical team. The patient should have been informed that it is imperative to adhere to the medical regimen implemented by his team along with the risks of not doing so. In the event disease-related complications arose, advanced directives should have been documented to avoid any unnecessary measures.
It is important to note, that with each change in status of the patient’s health status, the goal of treatment must be reassessed. The patient or surrogate decision-maker’s understanding of these goals is paramount in maintaining the patient’s autonomy. It is often said that effective communication is the bedrock of a healthy relationship. This is true regardless of type of relationship.
This is why I and Megan Vierhout wrote Integrated End of Life Care in Dementia: A Comprehensive Guide, a book targeted at providing a much-needed road map to navigate the many challenges involved in end-of-life care for individuals with dementia. Ultimately, our aim is to provide a compass for both health-care professionals and the families of those affected by the progressive effects of dementia. We provide practical advice on optimizing communication with individuals with dementia while taking their cognitive limitations, preferences and needs into account.
I invite you to explore the unpredictable terrain of end-of-life care for patients with dementia. Together, we can pave a smoother, sturdier path toward the practice of medicine as a true art form.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
4 Critical Things Female Runners Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to keeping up performance in the face of menopause, Shona Hendricks has advice:
Don’t let menopause run you down
- Prioritize recovery! Overtraining without adequate recovery just leads to decreased performance in the long term, and remember, you may not recover as quickly as you used to. If you’re still achey from your previous run, give it another day, or at least make it a lighter run.
- Slow down in easy and long runs! This isn’t “taking the easy way out”; it will improve your overall performance, reducing muscle damage, allowing for quicker recovery and ultimately better fitness gains.
- Focus on nutrition! And that means carbs too. A lot of people fighting menopausal weight gain reduce their intake of food, but without sufficient energy availability, you will not be able to run well. In particular, carbohydrates are vital for energy. Consume them sensibly and with fiber and proteins and fats rather than alone, but do consume them.
- Incorporate strength training! Your run is not “leg day” by itself. Furthermore, do whole-body strength training, to prevent injuries and improve overall performance. A strong core is particularly important.
For more on each of these (and some bonus comments about mobility training for runners), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Boost Your Digestive Enzymes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll Try To Make This Easy To Digest
Do you have a digestion-related problem?
If so, you’re far from alone; around 40% of Americans have digestive problems serious enough to disrupt everyday life:
New survey finds forty percent of Americans’ daily lives are disrupted by digestive troubles
…which puts Americans just a little over the global average of 35%:
Mostly likely on account of the Standard American Diet, or “SAD” as it often gets abbreviated in scientific literature.
There’s plenty we can do to improve gut health, for example:
- Making Friends With Your Gut (You Can Thank Us Later)
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- How Much Difference Do Probiotic Supplements Make?
Today we’re going to be examining digestive enzyme supplements!
What are digestive enzymes?
Digestive enzymes are enzymes that break down food into stuff we can use. Important amongst them are:
- Protease: breaks down proteins (into amino acids)
- Amylase: breaks down starches (into sugars)
- Lipase: breaks down fats (into fatty acids)
All three are available as popular supplements to aid digestion. How does the science stack up for them?
Protease
For this, we only found animal studies like this one, but the results have been promising:
Amylase
Again, the studies for this alone (not combined with other enzymes) have been solely from animal agriculture; here’s an example:
The Effect of Exogenous Amylase Supplementation on the Nutritional Value of Peas
Lipase
Unlike for protease and amylase, now we have human studies as well, and here’s what they had to say:
❝Lipase supplementation significantly reduced stomach fullness without change of EGG.
Furthermore, lipase supplementation may be helpful in control of FD symptom such as postprandial symptoms❞
~ Dr. Seon-Young Park & Dr. Jong-Sun Rew
Read more: Is Lipase Supplementation before a High Fat Meal Helpful to Patients with Functional Dyspepsia?
(short answer: yes, it is)
More studies found the same, such as:
Lipase Supplementation before a High-Fat Meal Reduces Perceptions of Fullness in Healthy Subjects
All together now!
When we look at studies for combination supplementation of digestive enzymes, more has been done, and/but it’s (as you might expect) less specific.
The following paper gives a good rundown:
Pancrelipase Therapy: A Combination Of Protease, Amylase, & Lipase
Is it safe?
For most people it is quite safe, but if taking high doses for a long time it can cause problems, and also there may be complications if you have diabetes, are otherwise immunocompromised, or have some other conditions (listed towards the end of the above-linked paper, along with further information that we can’t fit in here).
As ever, check with your doctor/pharmacist if you’re not completely sure!
Want some?
We don’t sell them, but for your convenience, here’s an example product on Amazon that contains all three
Enjoy!
We’ll Try To Make This Easy To Digest
Do you have a digestion-related problem?
If so, you’re far from alone; around 40% of Americans have digestive problems serious enough to disrupt everyday life:
New survey finds forty percent of Americans’ daily lives are disrupted by digestive troubles
…which puts Americans just a little over the global average of 35%:
Mostly likely on account of the Standard American Diet, or “SAD” as it often gets abbreviated in scientific literature.
There’s plenty we can do to improve gut health, for example:
- Making Friends With Your Gut (You Can Thank Us Later)
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- How Much Difference Do Probiotic Supplements Make?
Today we’re going to be examining digestive enzyme supplements!
What are digestive enzymes?
Digestive enzymes are enzymes that break down food into stuff we can use. Important amongst them are:
- Protease: breaks down proteins (into amino acids)
- Amylase: breaks down starches (into sugars)
- Lipase: breaks down fats (into fatty acids)
All three are available as popular supplements to aid digestion. How does the science stack up for them?
Protease
For this, we only found animal studies like this one, but the results have been promising:
Amylase
Again, the studies for this alone (not combined with other enzymes) have been solely from animal agriculture; here’s an example:
The Effect of Exogenous Amylase Supplementation on the Nutritional Value of Peas
Lipase
Unlike for protease and amylase, now we have human studies as well, and here’s what they had to say:
❝Lipase supplementation significantly reduced stomach fullness without change of EGG.
Furthermore, lipase supplementation may be helpful in control of FD symptom such as postprandial symptoms❞
~ Dr. Seon-Young Park & Dr. Jong-Sun Rew
Read more: Is Lipase Supplementation before a High Fat Meal Helpful to Patients with Functional Dyspepsia?
(short answer: yes, it is)
More studies found the same, such as:
Lipase Supplementation before a High-Fat Meal Reduces Perceptions of Fullness in Healthy Subjects
All together now!
When we look at studies for combination supplementation of digestive enzymes, more has been done, and/but it’s (as you might expect) less specific.
The following paper gives a good rundown:
Pancrelipase Therapy: A Combination Of Protease, Amylase, & Lipase
Is it safe?
For most people it is quite safe, but if taking high doses for a long time it can cause problems, and also there may be complications if you have diabetes, are otherwise immunocompromised, or have some other conditions (listed towards the end of the above-linked paper, along with further information that we can’t fit in here).
As ever, check with your doctor/pharmacist if you’re not completely sure!
Want some?
We don’t sell them, but for your convenience, here’s an example product on Amazon that contains all three
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fall Asleep In 2 Minutes (Doctor Explains)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beyond “sleep hygiene”, Dr. Siobhan Deshauer has insights to share:
Rest for your body and mind
First, do still do the basics. That means dimming/filtering lights for an hour before bed, lowering the room temperature a little, ensuring you have nice fresh sheets, not having alcohol or caffeine before bed, and getting out of bed if you’re not asleep within half an hour, to avoid associating being in bed with wakefulness.
Next, the extra tips:
- Progressive relaxation: tense and relax each muscle group from toes to head
- Box breathing: inhale, hold, exhale, and hold for 4 seconds each; helps calm the nervous system (it’s called “box breathing” because of the 4:4:4:4 setup)
- Diaphragmatic breathing: focus on belly breathing, with longer exhalation to activate the parasympathetic nervous system (note that this can, and even ideally should, be done at the same time as the previous)
- Cognitive shuffling: think of words starting with each letter of a chosen word while visualizing them (this is like “counting sheep”, but does the job better—the job in question being preventing your brain from moving to anything more strenuous or stressful)
For more on all of these plus some extra side-along advice, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Non-Sleep Deep Rest: A Neurobiologist’s Take ← a way to get many of the benefits of sleep, while awake
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: