HRT Side Effects & Troubleshooting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

This is Dr. Heather Hirsch. She’s a board-certified internist, and her clinical expertise focuses on women’s health, particularly in midlife and menopause, and its intersection with chronic diseases (ranging from things associated with sexual health, to things like osteoporosis and heart disease).
So, what does she want us to know?
HRT can be life-changingly positive, but it can be a shaky start
Hormone Replacement Therapy (HRT), and in this context she’s talking specifically about the most common kind, Menopausal Hormone Therapy (MHT), involves taking hormones that our body isn’t producing enough of.
If these are “bioidentical hormones” as used in most of the industrialized world and increasingly also in N. America, then this is by definition a supplement rather than a drug, for what it’s worth, whereas some non-bioidentical hormones (or hormone analogs, which by definition function similarly to hormones but aren’t the same thing) can function more like drugs.
We wrote a little about his previously:
Hormone Replacement Therapy: A Tale Of Two Approaches
For most people most of the time, bioidentical hormones are very much the best way to go, as they are not only more effective, but also have fewer side effects.
That said, even bioidentical hormones can have some undesired effects, so, how to deal with those?
Don’t worry; bleed happy
A reprise of (usually quite light) menstrual bleeding is the most common side effect of menopausal HRT.
This happens because estrogen affects* the uterus, leading to a build-up and shedding of the uterine lining.
*if you do not have a uterus, estrogen can effect uterine tissue. That’s not a typo—here we mean the verb “effect”, as in “cause to be”. It will not grow a new uterus, but it can cause some clumps of uterine tissue to appear; this means that it becomes possible to get endometriosis without having a uterus. This information should not be too shocking, as endometriosis is a matter of uterine tissue growing inconveniently, often in places where it shouldn’t, and sometimes quite far from the uterus (if present, or its usual location, if absent). However, the risk of this happening is far lower than if you actually have a uterus:
What you need to know about endometriosis
Back to “you have a uterus and it’s making you wish you didn’t”:
This bleeding should, however, be light. It’ll probably be oriented around a 28-day cycle even if you are taking your hormones at the same dose every day of the month, and the bleeding will probably taper off after about 6 months of this.
If the bleeding is heavier, all the time, or persists longer than 6 months, then speak to your gynecologist about it. Any of those three; it doesn’t have to be all three!
Bleeding outside of one’s normal cycle can be caused by anything from fibroids to cancer; statistically speaking it’s probably nothing too dire,but when your safety is in question, don’t bet on “probably”, and do get it checked out:
When A Period Is Very Late (i.e., Post-Menopause)
Dr. Hirsch recommends, as possible remedies to try (preferably under your gynecologist’s supervision):
- lowering your estrogen dose
- increasing your progesterone dose
- taking progesterone continuously instead of cyclically
And if you’re not taking progesterone, here’s why you might want to consider taking this important hormone that works with estrogen to do good things, and against estrogen to rein in some of estrogen’s less convenient things:
Progesterone Menopausal HRT: When, Why, And How To Benefit
(the above link contains, as well as textual information, an explanatory video from Dr. Hirsch herself)
Get the best of the breast
Calm your tits. Soothe your boobs. Destress your breasts. Hakuna your tatas. Undo the calamity beleaguering your mammaries.
Ok, more seriously…
Breast tenderness is another very common symptom when starting to take estrogen. It can worry a lot of people (à la “aagh, what is this and is it cancer!?”), but is usually nothing to worry about. But just to be sure, do also check out:
Keeping Abreast Of Your Cancer Risk: How To Triple Your Breast Cancer Survival Chances
Estrogen can cause feelings of breast fullness, soreness, nipple irritation, and sometimes lactation, but this later will be minimal—we’re talking a drop or two now and again, not anything that would feed a baby.
Basically, it happens when your body hasn’t been so accustomed to normal estrogen levels in a while, and suddenly wakes up with a jolt, saying to itself “Wait what are we doing puberty again now? I thought we did menopause? Are we pregnant? What’s going on? Ok, checking all systems!” and then may calm down not too long afterwards when it notes that everything is more or less as it should be already.
If this persists or is more than a minor inconvenience though, Dr. Hirsch recommends looking at the likely remedies of:
- Adjust estrogen (usually the cause)
- Adjust progesterone (less common)
- If it’s progesterone, changing the route of administration can ameliorate things
What if it’s not working? Is it just me?
Dr. Hirsch advises the most common reasons are simply:
- wrong formulation (e.g. animal-derived estrogen or hormone analog, instead of bioidentical)
- wrong dose (e.g. too low)
- wrong route of administration (e.g. oral vs transdermal; usually transdermal estradiol is most effective but many people do fine on oral; progesterone meanwhile is usually best as a pessary/suppository, but many people do fine on oral)
Writer’s example: in 2022 there was an estrogen shortage in my country, and while I had been on transdermal estradiol hemihydrate gel, I had to go onto oral estradiol valerate tablets for a few months, because that’s what was available. And the tablets simply did not work for me at all. I felt terrible and I have a good enough intuitive sense of my hormones to know when “something wrong is not right”, and a good enough knowledge of the pharmacology & physiology to know what’s probably happening (or not happening). And sure enough, when I got my blood test results, it was as though I’d been taking nothing. It was such a relief to get back on the gel once it became available again!
So, if something doesn’t seem to be working for you, speak up and get it fixed if at all possible.
See also: What You Should Have Been Told About Menopause Beforehand
Want to know more from Dr. Hirsch?
You might like this book of hers, which we haven’t reviewed yet, but present here for your interest:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Rest More Efficiently (Yes, Really)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Rest More Efficiently (Yes, Really)
We’ve talked before about how to recover more quickly after a workout, especially if you overdid it. There are a lot of tips in that article, so by all means check it out if you didn’t catch it at the time!
That was very specific to recovering from exercise, though. Today we’re looking at something a little different, a little more holistic.
You’re busier than you think
Maybe your life is an obvious blur of busy-ness. Maybe it’s not. But either way, you’re almost certainly busier than you think. Especially on a cellular level.
Your resting metabolic rate (RMR), or how many calories you burn while at rest (i.e., calories used just to keep you alive) will depend on various factors including age, sex, weight, body composition, and other things.
That said, it’ll probably be between 1000 and 2000 calories per day. You can get a rough idea of what it might be for you, using this calculator:
How Many Calories Do You Burn a Day at Rest (Doing Nothing)?
So if ever you wonder why you feel so exhausted, despite having done nothing, it could be that your body was busy:
- Metabolizing, generally (did you have a big meal?)
- Fighting an illness (bacterial or viral infection, for example)
- Fighting an imaginary illness and creating a real one in the process (stress, inflammation, etc)
- Recovering/rebuilding from something you did yesterday or even before that
- Thinking (your brain is your largest organ by mass, and consumes the most calories by far)
Your brain does not get a free pass on being part of your body! Just like if a certain muscle group were working out constantly for 16 hours you’d be feeling pretty tired, the same goes for the organ that is your brain, if it’s been working out constantly.
Your body is a composite organism—take advantage of that
Dolphins can shut down half of their brain at once, to let each hemisphere of the brain sleep independently in shifts. We (except in the case of split brain patients, where the corpus callosum has been severed) can’t do that, but we can let different parts of the organism that is our body work in shifts.
This is the real meaning of “a change is as a good as a rest”:
If you’ve been doing cognitive work (at your desk perhaps, maybe managing a spreadsheet, say), then taking a break to do crosswords will not, actually, give you break. Because you’re still sitting manipulating letters and numbers. As far as your brain (still having to do work!) is concerned, it’s basically the same. Nor will checking out social media; you’re still sitting examining a screen.
Instead, time to get physically active. Literally just doing the washing up would be a better break! Some yoga or Pilates would be perfect.
In contrast, if you’ve been doing a vigorous bit of gardening, then for example taking a break to lift weights isn’t going to be a break, because again you just switched to a similar task.
Better to pick up that book you’ve been meaning to read, or the crosswords we mentioned earlier. Or just lounge in your nicely-gardened garden.
The important thing is: to not require the same resources from the body (including the brain, it’s still part of the body) that you have been.
For more specific tips than we have room for here today, check out:
How to Take Better Breaks at Work, According to Research
Give your metabolism a break too
Not completely—you don’t need to be put into cryostasis or anything.
But, give your metabolism a rest, in relative terms. Intermittent fasting is great for precisely this; it lets your body rest and reset.
See: Intermittent Fasting: we sort the science from the hype!
So does the practice of meditation, by the way. You don’t have to get fancy with it, either:
Check out: No Frills, Evidence-Based Mindfulness
Enjoy, and rest well!
Share This Post
-
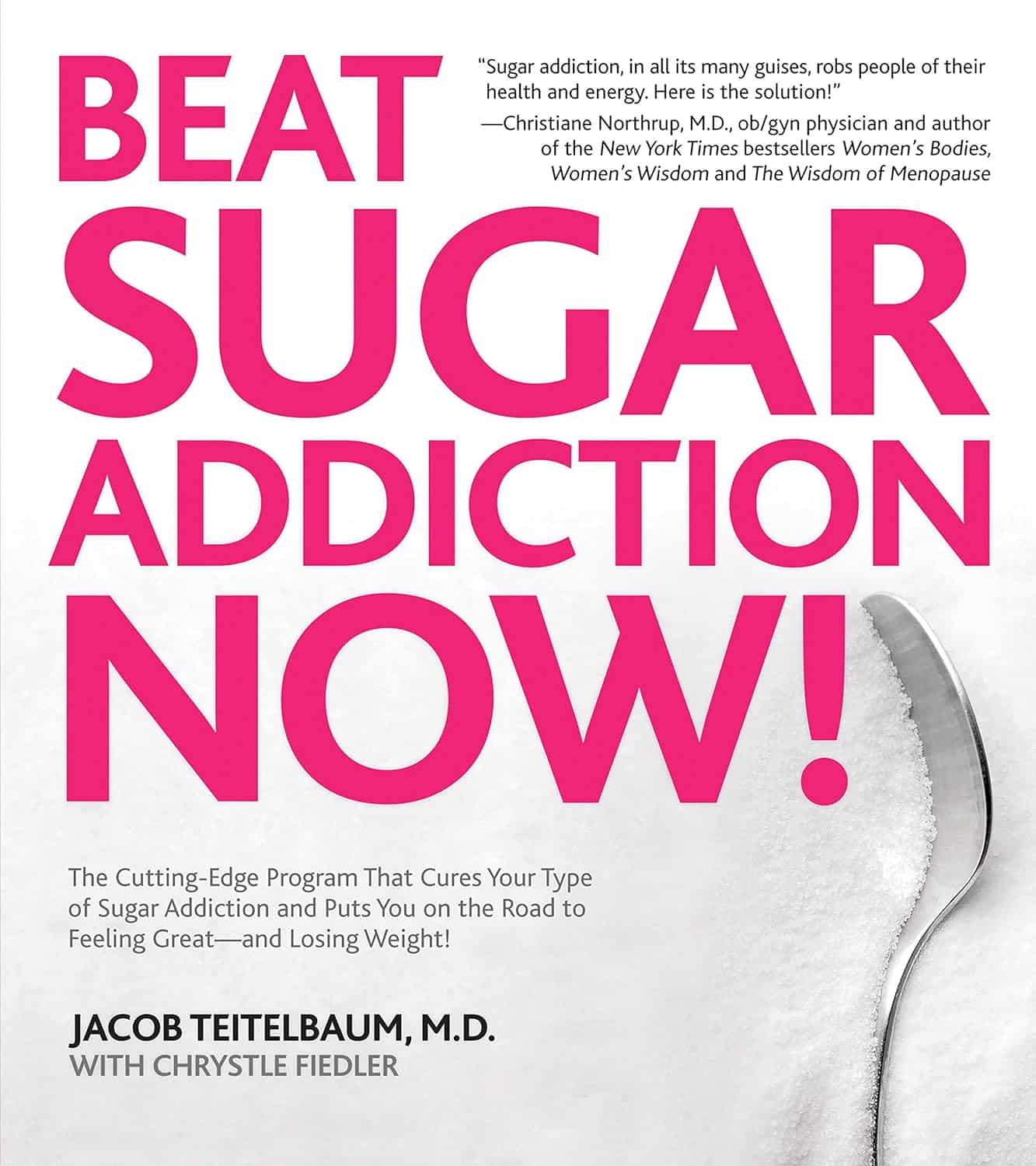
Beat Sugar Addiction Now! – by Dr. Jacob Teitelbaum & Chrystle Fiedler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sugar isn’t often thought of as an addiction in the same category as alcohol or nicotine, but it’s actually very similar in some ways…
A bold claim, but: in each case, it has to do with dopamine responses to something that has:
- an adverse effect on our health,
- a quickly developed tolerance to same,
- and unpleasant withdrawal symptoms when quitting.
However, not all sugar addictions are created equal, and Dr. Teitelbaum lays four different types of sugar addiction out for us:
- Most related to “I need to perform and I need to perform now”
- Most related to “I just need something to get me through one more stressful day, again, just like every day before it”
- Most related to “ate too much sugar because of the above, and now a gut overgrowth of C. albicans is at the wheel”
- Most related to “ate too much sugar because of the above, and now insulin resistance is a problem that perpetuates itself too”
Of course, these may overlap, and indeed, they tend to stack cumulatively as time goes by.
However, Dr. Teitelbaum notes that as readers we may recognize ourselves as being at a particular point in the above, and there are different advices for each of them.
You thought it was just going to be about going cold turkey? Nope!
Instead, a multi-vector approach is recommended, including adjustments to sleep, nutrition, immune health, hormonal health, and more.
In short: if you’ve been trying to to kick the “White Death” habit as Gloria Swanson called it (sugar, that is, not the WW2 Finnish sniper of the same name—we can’t help you with that one), then this book is really much more helpful than others that take the “well, just don’t eat it, then” approach!
Pick up your copy of Beat Sugar Addiction Now from Amazon, and start your journey!
Share This Post
-
Glycemic Index vs Glycemic Load vs Insulin Index
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Actually Use Those Indices
Carbohydrates are essential for our life, and/but often bring about our early demise. It would be a very conveniently simple world if it were simply a matter of “enjoy in moderation”, but the truth is, it’s not that simple.
To take an extreme example, for the sake of clearest illustration: The person who eats an 80% whole fruit diet (and makes up the necessary protein and fats etc in the other 20%) will probably be healthier than the person who eats a “standard American diet”, despite not practising moderation in their fruit-eating activities. The “standard American diet” has many faults, and one of those faults is how it promotes sporadic insulin spikes leading to metabolic disease.
If your breakfast is a glass of orange juice, this is a supremely “moderate” consumption, but an insulin spike is an insulin spike.
Quick sidenote: if you’re wondering why eating immoderate amounts of fruit is unlikely to cause such spikes, but a single glass of orange juice is, check out:
Which Sugars Are Healthier, And Which Are Just The Same?
Glycemic Index
The first tool in our toolbox here is glycemic index, or GI.
GI measures how much a carb-containing food raises blood glucose levels, also called blood sugar levels, but it’s just glucose that’s actually measured, bearing in mind that more complex carbs will generally get broken down to glucose.
Pure glucose has a GI of 100, and other foods are ranked from 0 to 100 based on how they compare.
Sometimes, what we do to foods changes its GI.
- Some is because it changed form, like the above example of whole fruit (low GI) vs fruit juice (high GI).
- Some is because of more “industrial” refinement processes, such as whole grain wheat (medium GI) vs white flour and white flour products (high GI)
- Some is because of other changes, like starches that were allowed to cool before being reheated (or eaten cold).
Broadly speaking, a daily average GI of 45 is considered great.
But that’s not the whole story…
Glycemic Load
Glycemic Load, or GL, takes the GI and says “ok, but how much of it was there?”, because this is often relevant information.
Refined sugar may have a high GI, but half a teaspoon of sugar in your coffee isn’t going to move your blood sugar levels as much as a glass of Coke, say—the latter simply has more sugar in, and just the same zero fiber.
GL is calculated by (grams of carbs / 100) x GI, by the way.
But it still misses some important things, so now let’s look at…
Insulin Index
Insulin Index, which does not get an abbreviation (probably because of the potentially confusing appearance of “II”), measures the rise in insulin levels, regardless of glucose levels.
This is important, because a lot of insulin response is independent of blood glucose:
- Some is because of other sugars, some some is in response to fats, and yes, even proteins.
- Some is a function of metabolic base rate.
- Some is a stress response.
- Some remains a mystery!
Another reason it’s important is that insulin drives weight gain and metabolic disorders far more than glucose.
Note: the indices of foods are calculated based on average non-diabetic response. If for example you have Type 1 Diabetes, then when you take a certain food, your rise in insulin is going to be whatever insulin you then take, because your body’s insulin response is disrupted by being too busy fighting a civil war in your pancreas.
If your diabetes is type 2, or you are prediabetic, then a lot of different things could happen depending on the stage and state of your diabetes, but the insulin index is still a very good thing to be aware of, because you want to resensitize your body to insulin, which means (barring any urgent actions for immediate management of hyper- or hypoglycemia, obviously) you want to eat foods with a low insulin index where possible.
Great! What foods have a low insulin index?
Many factors affect insulin index, but to speak in general terms:
- Whole plant foods are usually top-tier options
- Lean and/or white meats generally have lower insulin index than red and/or fatty ones
- Unprocessed is generally lower than processed
- The more solid a food is, generally the lower its insulin index compared to a less solid version of the same food (e.g. baked potatoes vs mashed potatoes; cheese vs milk, etc)
But do remember the non-food factors too! This means where possible:
- reducing/managing stress
- getting frequent exercise
- getting good sleep
- practising intermittent fasting
See for example (we promise you it’s relevant):
Fix Chronic Fatigue & Regain Your Energy, By Science
…as are (especially recommendable!) the two links we drop at the bottom of that page; do check them out if you can
Take care!
Share This Post
Related Posts
-
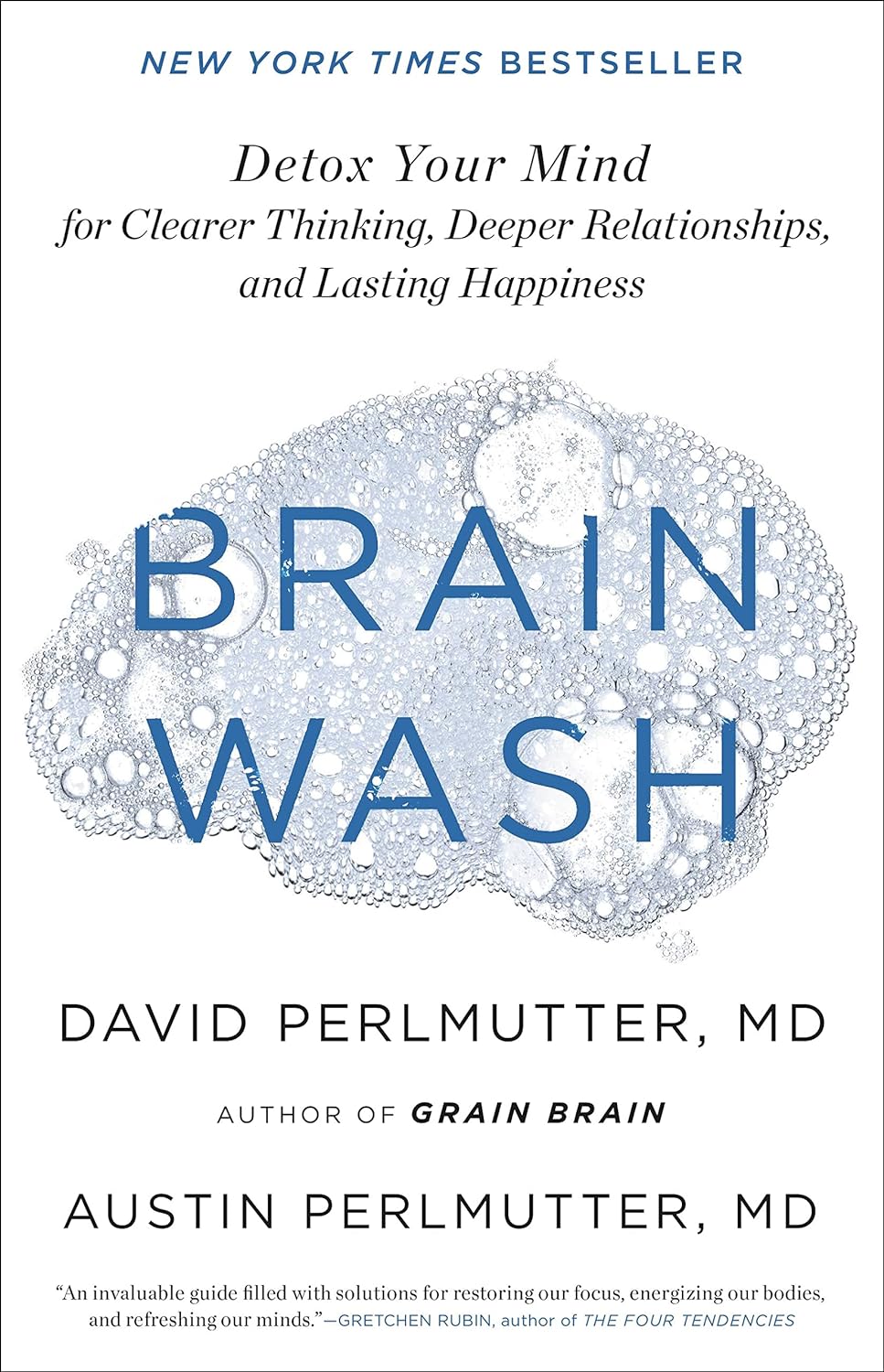
Brain Wash – by Dr. David Perlmutter, Dr. Austin Perlmutter, and Kristen Loberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be familiar with the lead author of this book, Dr. David Perlmutter, as a big name in the world of preventative healthcare. A lot of his work has focused specifically on carbohydrate metabolism, and he is as associated with grains and he is with brains. This book focuses on the latter.
Dr. Perlmutter et al. take a methodical look at all that is ailing our brains in this modern world, and systematically lay out a plan for improving each aspect.
The advice is far from just dietary, though the chapter on diet takes a clear stance:
❝The food you eat and the beverages you drink change your emotions, your thoughts, and the way you perceive the world❞
The style is explanatory, and the book can be read comfortably as a “sit down and read it cover to cover” book; it’s an enjoyable, informative, and useful read.
Bottom line: if you’d like to give your brain a gentle overhaul, this is the one-stop-shop book to give you the tools to do just that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Best Workouts for Women Over 40 To Give Your Metabolism A Makeover
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After 40, the usual course of events goes: your lean muscle mass decreases, which slows your metabolism and makes it easier to gain fat. At the same time, bone density decreases, increasing the risk of osteoporosis and frailty. This leads to lower mobility, flexibility, and overall frustration.
But it doesn’t have to be that way! Fitness coach Jessica Cooke explains how:
It all depends on this
Strength training helps counteract these effects by increasing lean muscle mass, which boosts metabolism and fat burning. It also improves bone density, reducing the risk of osteoporosis. Plus, it builds strength, fitness, and a toned physique.
The best part? It doesn’t require long workouts—short, effective sessions work best.
While walking is very beneficial for general health, it doesn’t provide the resistance needed to build muscle. Without resistance, your body composition won’t change, and so your metabolism will remain the same. Strength training is essential for burning fat at rest and improving overall fitness.
You don’t have to do high-impact exercises or jumping to see results. Low-impact strength training is effective and gentle on the joints. Lifting weights or using your body weight in a controlled manner will help build muscle and improve strength.
Many women only do cardio and neglect strength training, leading to minimal progress. Another common mistake is overcomplicating workouts—simple, consistent strength training is all you need.
Aim to strength train three times per week for 20 minutes. Focus on compound movements that work multiple muscle groups, such as:
- squats
- lunges
- deadlifts
- press-ups
- shoulder presses
- upright rows
- planks
- glute bridges
- sit-ups
- Russian twists
Start with light (e.g. 2-3 kg) weights and maintain proper form.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Don’t Let Menopause Run You Down: 4 Critical Things Female Runners Should Know
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid UTIs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Psst… A Word To The Wise
Urinary Tract Infections (UTIs) can strike at any age, but they get a lot more common as we get older:
- About 10% of women over 65 have had one
- About 30% of women over 85 have had one
Source: Urinary tract infection in older adults
Note: those figures are almost certainly very underreported, so the real figures are doubtlessly higher. However, we print them here as they’re still indicative of a disproportionate increase in risk over time.
What about men?
Men do get UTIs too, but at a much lower rate. The difference in average urethra length means that women are typically 30x more likely to get a UTI.
However! If a man does get one, then assuming the average longer urethra, it will likely take much more treatment to fix:
Case study: 26-Year-Old Man With Recurrent Urinary Tract Infections
Risk factors you might want to know about
While you may not be able to do much about your age or the length of your urethra, there are some risk factors that can be more useful to know:
Catheterization
You might logically think that having a catheter would be the equivalent of having a really long urethra, thus keeping you safe, but unfortunately, the opposite is true:
Read more: Review of Catheter-Associated Urinary Tract Infections
Untreated menopause
Low estrogen levels can cause vaginal tissue to dry, making it easier for pathogens to grow.
For more information on menopausal HRT, see:
What You Should Have Been Told About Menopause Beforehand
Sexual activity
Most kinds of sexual activity carry a risk of bringing germs very close to the urethra. Without wishing to be too indelicate: anything that’s going there should be clean, so it’s a case for washing your hands/partner(s)/toys etc.
For the latter, beyond soap and water, you might also consider investing in a UV sanitizer box ← This example has a 9” capacity; if you shop around though, be sure to check the size is sufficient!
Kidney stones and other kidney diseases
Anything that impedes the flow of urine can raise the risk of a UTI.
See also: Keeping Your Kidneys Healthy (Especially After 60)
Diabetes
How much you can control this one will obviously depend on which type of diabetes you have, but diabetes of any type is an immunocompromizing condition. If you can, managing it as well as possible will help many aspects of your health, including this one.
More on that:
How To Prevent And Reverse Type 2 Diabetes
Note: In the case of Type 1 Diabetes, the above advice will (alas) not help you to prevent or reverse it. However, reducing/avoiding insulin resistance is even more important in cases of T1D (because if your exogenous insulin stops working, you die), so the advice is good all the same.
How do I know if I have a UTI?
Routine screening isn’t really a thing, since the symptoms are usually quite self-evident. If it hurts/burns when you pee, the most likely reason is a UTI.
Get it checked out; the test is a (non-invasive) urinalysis test. In other words, you’ll give a urine sample and they’ll test that.
Anything else I can do to avoid it?
Yes! We wrote previously about the benefits of cranberry supplementation, which was found even to rival antibiotics:
❝…recommend cranberry ingestion to decrease the incidence of urinary tract infections, particularly in individuals with recurrent urinary tract infections. This would also reduce the [need for] administration of antibiotics❞
Read more: Health Benefits Of Cranberries
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: