How To Stop Binge-Eating: Flip This Switch!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“The Big Eating Therapist” Sarah Dosanjh has insights from both personal and professional experience:
No “Tough Love” Necessary
Eating certain foods is often socially shamed, and it’s easy to internalize that, and feel guilty. While often guilt is considered a pro-social emotion that helps people to avoid erring in a way that will get us excluded from the tribe (bearing in mind that for most of our evolutionary history, exile would mean near-certain death), it is not good at behavior modification when it comes to addictions or anything similar to addictions.
The reason for this is that if we indulge in a pleasure we feel we “shouldn’t” and expect we’d be shamed for, we then feel bad, and we immediately want something to make us feel better. Guess what that something will be. That’s right: the very same thing we literally just felt ashamed about.
So guilt is not helpful when it comes to (for example) avoiding binge-eating.
Instead, Dosanjh points us to a study whereby dieters ate a donut and drank water, before being given candy for taste testing. The control group proceeded without intervention, while the experimental group had a self-compassion intervention between the donut and the candy. This meant that researchers told the participants not to feel bad about eating the donut, emphasizing self-kindness, mindfulness, and common humanity. The study found that those who received the intervention, ate significantly less candy.
What we can learn from this is: we must be kind to ourselves. Allowing ourselves, consciously and mindfully, “a little treat”, secures its status as being “little”, and “a treat”. Then we smile, thinking “yes, that was a nice little thing to do for myself”, and proceed with our day.
This kind of self-compassion helps avoid the “meta-binge” process, where guilt from one thing leads to immediately reaching for another.
For more on this, plus a link to the study she mentioned, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
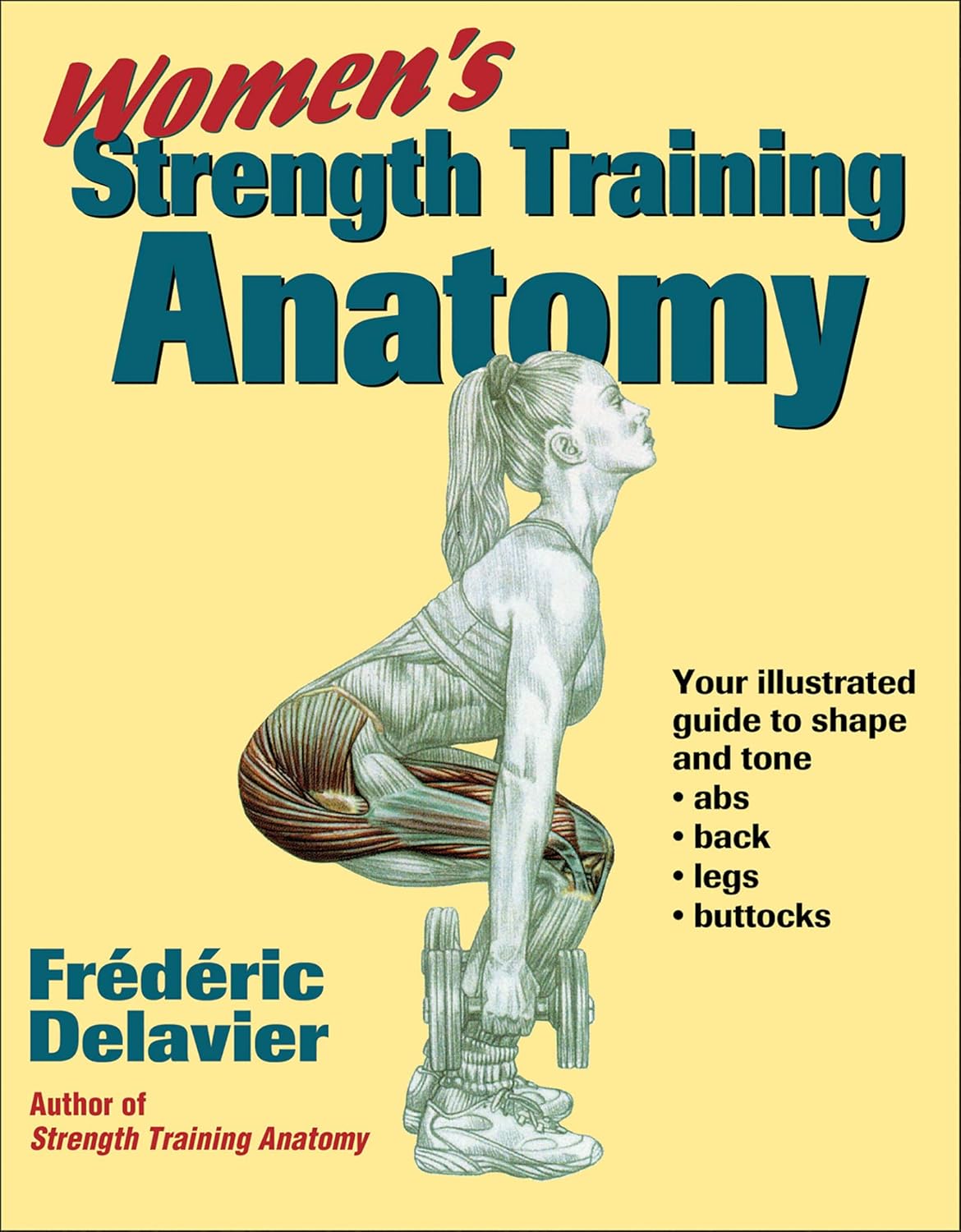
Women’s Strength Training Anatomy – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fitness guides for women tend to differ from fitness guides for men, in the wrong ways:
“Do some squats and jumping jacks, and here’s a exercise for your abs; you too can look like our model here”
In those other books we are left wonder: where’s the underlying information? Where are the explanations that aren’t condescending? Where, dare we ask, is the understanding that a woman might ever lift something heavier than a baby?
Delavier, in contrast, delivers. With 130 pages of detailed anatomical diagrams for all kinds of exercises to genuinely craft your body the way you want it for you. Bigger here, smaller there, functional strength, you decide.
And rest assured: no, you won’t end up looking like Arnold Schwarzenegger unless you not only eat like him, but also have his genes (and possibly his, uh, “supplement” regime).
What you will get though, is a deep understanding of how to tailor your exercise routine to actually deliver the personalized and specific results that you want.
Pick Up Today’s Book on Amazon!
Not looking for a feminine figure? You may like the same author’s book for men:
Share This Post
-
You’re Not Forgetful: How To Remember Everything
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Elizabeth Filips, medical student busy learning a lot of information, explains how in today’s video:
Active processing
An important thing to keep in mind is that forgetting is an active process, not passive as once believed. It has its own neurotransmitters and pathways, and as such, to improve memory, it’s essential to understand and manage forgetting.
So, how does forgetting occur? Memories are stored with cues or tags, which help retrieve information. However, overloading cues with too much information can cause “transient forgetting”—that is to say, the information is still in there somewhere; you just don’t have the filing system required to retrieve the data. This is the kind of thing that you will try hard to remember at some point in the day when you need it, fail, and then wake up at 3am with an “Aha!” because your brain finally found what you were looking for. So, to avoid that, use unique and strong cues to help improve recall (mnemonics are good for this, as are conceptual anchors).
While memory does not appear to actually be finite, there is some practical truth in the “finite storage” model insofar as learning new information can overwrite previous knowledge, iff your brain mistakes it for an update rather than addition. So for that reason, it’s good to periodically go over old information—in psychology this is called rehearsal, which may conjure theatrical images, but it can be as simple as mentally repeating a phone number, a mnemonic, or visually remembering a route one used to take to go somewhere.
Self-perception affects memory performance. Negative beliefs about one’s memory can worsen performance (so don’t say “I have a bad memory”, even to yourself, and in contrast, find more positive affirmations to make about your memory), and mental health in general plays a significant role in memory. For example, if you have ever had an extended period of depression, then chances are good you have some huge gaps in your memory for that time in your life.
A lot of what we learned in school was wrong—especially what we learned about learning. Traditional (vertical) learning is harder to retain, whereas horizontal learning (connecting topics through shared characteristics) creates stronger, interconnected memories. In short, your memories should tell contextual stories, not be isolated points of data.
Embarking on a new course of study? Yes? (If not, then why not? Pick something!)
It may be difficult at first, but experts memorize things more quickly due to built-up intuition in their field. For example a chess master can glance at a chess board for about 5 seconds and memorize the position—but only if the position is one that could reasonably arise in a game; if the pieces are just placed at random, then their memorization ability plummets to that of the average person, because their expertise has been nullified.
What this means in practical terms: building a “skeleton” framework before learning can enhance memorization through logical connections. For this reason, if embarking on a serious course of study, getting a good initial overview when you start is critical, so that you have a context for the rest of what you learn to go into. For example, let’s say you want to learn a language; if you first quickly do a very basic bare-bones course, such as from Duolingo or similar, then even though you’ll have a very small vocabulary and a modest grasp of grammar and make many mistakes and have a lot of holes in your knowledge, you now have somewhere to “fit” every new word or idea you learn. Same goes for other fields of study; for example, a doctor can be told about a new drug and remember everything about it immediately, because they understand the systems it interacts with, understand how it does what it does, and can compare it mentally to similar drugs, and they thus have a “place” in that overall system for the drug information to reside. But for someone who knows nothing about medicine, it’s just a lot of big words with no meaning. So: framework first, details later.
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Boost Your Memory Immediately (Without Supplements)
Take care!
Share This Post
-
Energize! – by Dr. Michael Breus & Stacey Griffith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book book by Dr. Breus, The Power Of When. So what’s different in this one?
While the chronotypes featured in The Power Of When also feature here (and sufficient explanation is given to make this a fine stand-alone book), this book has a lot to do with metabolism also. By considering a person’s genetically predisposed metabolic rate to be fast, medium, or slow (per being an ectomorph, mesomorph, or endomorph), and then putting that next to one’s sleep chronotype, we get 12 sub-categories that in this book each get an optimized protocol of sleep, exercise (further divided into: what kind of exercise when), and eating/fasting.
Which, in effect, amounts to a personalized coaching program for optimized energy!
The guidance is based on a combination of actual science plus “if this then that” observation-based principles—of the kind that could be described as science if they had been studied clinically instead of informally. Dr. Breus is a sleep scientist, by the way, and his co-author Stacey Griffith is a fitness coach. So between the two of them, they have sleep and exercise covered, and the fasting content is very reasonable and entirely consistent with current consensus of good practice.
The style is very pop-psychology, and very readable, and has a much more upbeat feel than The Power Of When, which seems to be because of Griffith’s presence as a co-author (most of the book is written from a neutral perspective, and some parts have first-person sections by each of the authors, so the style becomes distinct accordingly).
Bottom line: if you’d like to be more energized but [personal reason why not here] then this book may not fix all your problems, but it’ll almost certainly make a big difference and help you to stop sabotaging things and work with your body rather than against it.
Share This Post
Related Posts
-
The Doctor’s Kitchen – by Dr. Rupy Aujla
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured Dr. Aujla before as an expert-of-the-week, and now it’s time to review a book by him. What’s his deal, and what should you expect?
Dr. Aujla first outlines the case for food as medicine. Not just “eat nutritionally balanced meals”, but literally, “here are the medicinal properties of these plants”. Think of some of the herbs and spices we’ve featured in our Monday Research Reviews, and add in medicinal properties of cancer-fighting cruciferous vegetables, bananas with dopamine and dopamine precursors, berries full of polyphenols, hemp seeds that fight cognitive decline, and so forth.
Most of the book is given over to recipes. They’re plant-centric, but mostly not vegan. They’re consistent with the Mediterranean diet, but mostly Indian. They’re economically mindful (favoring cheap ingredients where reasonable) while giving a nod to where an extra dollar will elevate the meal. They don’t give calorie values etc—this is a feature not a bug, as Dr. Aujla is of the “positive dieting” camp that advocates for us to “count colors, not calories”. Which, we have to admit, makes for very stress-free cooking, too.
Dr. Aujla is himself an Indian Brit, by the way, which gives him two intersecting factors for having a taste for spices. If you don’t share that taste, just go easier on the pepper etc.
As for the medicinal properties we mentioned up top? Four pages of references at the back, for any who are curious to look up the science of them. We at 10almonds do love references!
Bottom line: if you like tasty food and you’re looking for a one-stop, well-rounded, food-as-medicine cookbook, this one is a top-tier choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
To Medicate or Not? That is the Question! – by Dr. Asha Bohannon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medications are, of course, a necessity of life (literally!) for many, especially as we get older. Nevertheless, overmedication is also a big problem that can cause a lot of harm too, and guess what, it comes with the exact same “especially as we get older” tag too.
So, what does Dr. Bohannon (a doctor of pharmacy, diabetes educator, and personal trainer too) recommend?
Simply put: she recommends starting with a comprehensive health history assessment and analysing one’s medication/supplement profile, before getting lab work done, tweaking all the things that can be tweaked along the way, and—of course—not neglecting lifestyle medicine either.
The book is prefaced and ended with pep talks that probably a person who has already bought the book does not need, but they don’t detract from the practical content either. Nevertheless, it feels a little odd that it takes until chapter 4 to reach “step 1” of her 7-step method!
The style throughout is conversational and energetic, but not overly padded with hype; it’s just a very casual style. Nevertheless, she brings to bear her professional knowledge and understanding as a doctor of pharmacy, to include her insights into the industry that one might not observe from outside of it.
Bottom line: if you’d like to do your own personal meds review and want to “know enough to ask the right questions” before bringing it up with your doctor, this book is a fine choice for that.
Click here to check out To Medicate Or Not, and make informed choices!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dr. Greger’s Anti-Aging Eight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Greger’s Anti-Aging Eight
This is Dr. Michael Greger. We’ve featured him before: Brain Food? The Eyes Have It!
This time, we’re working from his latest book, the excellent “How Not To Age”, which we reviewed all so recently. It is very information-dense, but we’re going to be focussing on one part, his “anti-aging eight”, that is to say, eight interventions he rates the most highly to slow aging in general (other parts of the book pertained to slowing eleven specific pathways of aging, or preserving specific bodily functions against aging, for example).
Without further ado, his “anti-aging eight” are…
- Nuts
- Greens
- Berries
- Xenohormesis & microRNA manipulation
- Prebiotics & postbiotics
- Caloric restriction / IF
- Protein restriction
- NAD+
As you may have noticed, some of these are things might appear already on your grocery shopping list; others don’t seem so “household”. Let’s break them down:
Nuts, greens, berries
These are amongst the most nutrient-dense and phytochemical-useful parts of the diet that Dr. Greger advocates for in his already-famous “Dr. Greger’s Daily Dozen”.
For brevity, we’ll not go into the science of these here, but will advise you: eat a daily portion of nuts, a daily portion of berries, and a couple of daily portions of greens.
Xenohormesis & microRNA manipulation
You might, actually, have these on your grocery shopping list too!
Hormesis, you may recall from previous editions of 10almonds, is about engaging in a small amount of eustress to trigger the body’s self-strengthening response, for example:
Xenohormesis is about getting similar benefits, second-hand.
For example, plants that have been grown to “organic” standards (i.e. without artificial pesticides, herbicides, fertilizers) have had to adapt to their relatively harsher environment by upping their levels of protective polyphenols and other phytochemicals that, as it turns out, are as beneficial to us as they are to the plants:
Hormetic Effects of Phytochemicals on Health and Longevity
Additionally, the flip side of xenohormesis is that some plant compounds can themselves act as a source of hormetic stress that end up bolstering us. For example:
In essence, it’s not just that it has anti-oxidant effect; it also provides a tiny oxidative-stress immunization against serious sources of oxidative stress—and thus, aging.
MicroRNA manipulation is, alas, too complex to truly summarize an entire chapter in a line or two, but it has to do with genetic information from the food that we eat having a beneficial or deleterious effect to our own health:
Diet-derived microRNAs: unicorn or silver bullet?
A couple of quick takeaways (out of very many) from Dr. Greger’s chapter on this is to spring for the better quality olive oil, and skip the cow’s milk:
- Impact of Phenol-Enriched Virgin Olive Oils on the Postprandial Levels of Circulating microRNAs Related to Cardiovascular Disease
- MicroRNA exosomes of pasteurized milk: potential pathogens of Western diseases
Prebiotics & Postbiotics
We’re short on space, so we’ll link you to a previous article, and tell you that it’s important against aging too:
Making Friends With Your Gut (You Can Thank Us Later)
An example of how one of Dr. Greger’s most-recommended postbiotics helps against aging, by the way:
- The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans
- Urolithin A improves muscle strength, exercise performance, and biomarkers of mitochondrial health in a randomized trial in middle-aged adults
(Urolithin can be found in many plants, and especially those containing tannins)
See also: How to Make Urolithin Postbiotics from Tannins
Caloric restriction / Intermittent fasting
This is about lowering metabolic load and promoting cellular apoptosis (programmed cell death; sounds bad; is good) and autophagy (self-consumption; again, sounds bad; is good).
For example, he cites the intermittent fasters’ 46% lower risk of dying in the subsequent years of follow-up in this longitudinal study:
For brevity we’ll link to our previous IF article, but we’ll revisit caloric restriction in a main feature on of these days:
Fasting Without Crashing? We sort the science from the hype!
Dr. Greger favours caloric restriction over intermittent fasting, arguing that it is easier to adhere to and harder to get wrong if one has some confounding factor (e.g. diabetes, or a medication that requires food at certain times, etc). If adhered to healthily, the benefits appear to be comparable for each, though.
Protein restriction
In contrast to our recent main feature Protein vs Sarcopenia, in which that week’s featured expert argued for high protein consumption levels, protein restriction can, on the other hand, have anti-aging effects. A reminder that our body is a complex organism, and sometimes what’s good for one thing is bad for another!
Dr. Greger offers protein restriction as a way to get many of the benefits of caloric restriction, without caloric restriction. He further notes that caloric restriction without protein restriction doesn’t decrease IGF-1 levels (a marker of aging).
However, for FGF21 levels (these are good and we want them higher to stay younger), what matters more than lowering proteins in general is lowering levels of the amino acid methionine—found mostly in animal products, not plants—so the source of the protein matters:
For example, legumes deliver only 5–10% of the methionine that meat does, for the same amount of protein, so that’s a factor to bear in mind.
NAD+
This is about nicotinamide adenine dinucleotide, or NAD+ to its friends.
NAD+ levels decline with age, and that decline is a causal factor in aging, and boosting the levels can slow aging:
Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
Can we get NAD+ from food? We can, but not in useful quantities or with sufficient bioavailability.
Supplements, then? Dr. Greger finds the evidence for their usefulness lacking, in interventional trials.
How to boost NAD+, then? Dr. Greger prescribes…
Exercise! It boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
Another study on resistance training found the same 127% boost:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: