How Gluconolactone Restores Immune Regulation In Lupus
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s be clear up front: this will not cure lupus.
However, it will interrupt the pathology of lupus in such a way as to, as the title says, restore immune regulation—so that your body stops attacking itself, or at the very least, attacks itself significantly less.
What is gluconolactone anyway?
Gluconolactone (also called glucono-δ-lactone) an oxidized derivative of glucose, when glucose is exposed to oxygen and a certain enzyme (glucose oxidase). It’s used in various food-related fermentation processes, and also helps such foods to have a tangy flavor.
It’s also known as E575, showing that E-numbers need not always be scary 🙂
How does it work?
First, a recap on how lupus works: lupus is an autoimmune disease where the immune system attacks its own tissues, causing inflammation and organ damage (to oversimplify it in very few words).
Next, how lupus is currently treated: mostly with immunosuppressant drugs, which reduce symptoms but have significant side effects, not least of all the fact that your immune system will be suppressed, leaving you vulnerable to infections, cancer, aging, and the like. So, there’s really a “damned if you do, damned if you don’t” aspect here (because untreated lupus will run your immune system into the ground with its chronic inflammation, which will also leave you vulnerable to the aforementioned things).
See also: How to Prevent (or Reduce) Inflammation
Now, how gluconolactone works: it increases the number of regulatory T-cells (also called “Tregs” by scientists who don’t want to have to say/write “regulatory T-cells” many times per day), which are the ones that tell the rest of your immune system what not to attack. It also inhibits pro-inflammatory T-helper-cells that are otherwise involved in autoimmune dysfunction.
Where is the science for this?
It’s a shiny new paper that covers three angles:
- In lupus-suffering mouse in vivo studies, it improved Treg function and reduced inflammatory skin rashes
- In human cell culture in vitro studies (with cell cultures from human lupus patients), it bolstered Treg count and improved immune regulation
- In human patient in vivo studies, a gluconolactone cream controlled skin inflammation and improved the clinical and histologic appearance of the skin lesions within 2 weeks
❝These results suggest that gluconolactone could be a targeted treatment option with fewer side effects for autoimmune diseases such as lupus.
Gluconolactone acts like a ‘power food’ for regulatory T cells—a real win-win situation for immune regulation❞
~ Dr. Antonios Kolios
You can find the paper itself here:
Where can I get gluconolactone?
At the moment, this is still in the clinical trials phase, so it’s not something you can get a prescription for yet, alas.
But definitely keep an eye out for it!
We would hypothesize that eating foods fermented with E575 (it’s sometimes used in feta cheese, hence today’s featured image, and it’s also often used as a pickling agent) may well help, but that’s just our hypothesis as it isn’t what was tested in the above studies.
Want to learn more?
In the meantime, if you’d like to learn more about lupus, we recommend this very comprehensive book:
*The “et al.” are: Jemima Albayda, MD; Divya Angra, MD; Alan N. Baer, MD; Sasha Bernatsky, MD, PhD; George Bertsias, MD, PhD; Ashira D. Blazer, MD; Ian Bruce, MD; Jill Buyon, MD; Yashaar Chaichian, MD; Maria Chou, MD; Sharon Christie, Esq; Angelique N. Collamer, MD; Ashté Collins, MD; Caitlin O. Cruz, MD; Mark M. Cruz, MD; Dana DiRenzo, MD; Jess D. Edison, MD; Titilola Falasinnu, PhD; Andrea Fava, MD; Cheri Frey, MD; Neda F. Gould, PhD; Nishant Gupta, MD; Sarthak Gupta, MD; Sarfaraz Hasni, MD; David Hunt, MD; Mariana J. Kaplan, MD; Alfred Kim, MD; Deborah Lyu Kim, DO; Rukmini Konatalapalli, MD; Fotios Koumpouras, MD; Vasileios C. Kyttaris, MD; Jerik Leung, MPH; Hector A. Medina, MD; Timothy Niewold, MD; Julie Nusbaum, MD; Ginette Okoye, MD; Sarah L. Patterson, MD; Ziv Paz, MD; Darryn Potosky, MD; Rachel C. Robbins, MD; Neha S. Shah, MD; Matthew A. Sherman, MD; Yevgeniy Sheyn, MD; Julia F. Simard, ScD; Jonathan Solomon, MD; Rodger Stitt, MD; George Stojan, MD; Sangeeta Sule, MD; Barbara Taylor, CPPM, CRHC; George Tsokos, MD; Ian Ward, MD; Emma Weeding, MD; Arthur Weinstein, MD; Sean A. Whelton, MD
The reason we mention this is to render it clear that this isn’t one man’s opinions (as happens with many books about certain topics), but rather, a panel of that many doctors all agreeing that this is correct and good, evidence-based, up-to-date (as of the publication of this latest revised edition) information.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stop Cancer 20 Years Ago
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Get Abreast And Keep Abreast
This is Dr. Jenn Simmons. Her specialization is integrative oncology, as she—then a breast cancer surgeon—got breast cancer, decided the system wasn’t nearly as good from the patients’ side of things as from the doctors’ side, and took to educate herself, and now others, on how things can be better.
What does she want us to know?
Start now
If you have breast cancer, the best time to start adjusting your lifestyle might be 20 years ago, but the second-best time is now. We realize our readers with breast cancer (or a history thereof) probably have indeed started already—all strength to you.
What this means for those of us without breast cancer (or a history therof) is: start now
Even if you don’t have a genetic risk factor, even if there’s no history of it in your family, there’s just no reason not to start now.
Start what, you ask? Taking away its roots. And how?
Inflammation as the root of cancer
To oversimplify: cancer occurs because an accidentally immortal cell replicates and replicates and replicates and takes any nearby resources to keep on going. While science doesn’t know all the details of how this happens, it is a factor of genetic mutation (itself a normal process, without which evolution would be impossible), something which in turn is accelerated by damage to the DNA. The damage to the DNA? That occurs (often as not) as a result of cellular oxidation. Cellular oxidation is far from the only genotoxic thing out there, and a lot of non-food “this thing causes cancer” warnings are usually about other kinds of genotoxicity. But cellular oxidation is a big one, and it’s one that we can fight vigorously with our lifestyle.
Because cellular oxidation and inflammation go hand-in-hand, reducing one tends to reduce the other. That’s why so often you’ll see in our Research Review Monday features, a line that goes something like:
“and now for those things that usually come together: antioxidant, anti-inflammatory, anticancer, and anti-aging”
So, fight inflammation now, and have a reduced risk of a lot of other woes later.
See: How to Prevent (or Reduce) Inflammation
Don’t settle for “normal”
People are told, correctly but not always helpfully, such things as:
- It’s normal to have less energy at your age
- It’s normal to have a weaker immune system at your age
- It’s normal to be at a higher risk of diabetes, heart disease, etc
…and many more. And these things are true! But that doesn’t mean we have to settle for them.
We can be all the way over on the healthy end of the distribution curve. We can do that!
(so can everyone else, given sufficient opportunity and resources, because health is not a zero-sum game)
If we’re going to get a cancer diagnosis, then our 60s are the decade where we’re most likely to get it. Earlier than that and the risk is extant but lower; later than that and technically the risk increases, but we probably got it already in our 60s.
So, if we be younger than 60, then now’s a good time to prepare to hit the ground running when we get there. And if we missed that chance, then again, the second-best time is now:
See: Focusing On Health In Our Sixties
Fast to live
Of course, anything can happen to anyone at any age (alas), but this is about the benefits of living a fasting lifestyle—that is to say, not just fasting for a 4-week health kick or something, but making it one’s “new normal” and just continuing it for life.
This doesn’t mean “never eat”, of course, but it does mean “practice intermittent fasting, if you can”—something that Dr. Simmons strongly advocates.
See: Intermittent Fasting: We Sort The Science From The Hype
While this calls back to the previous “fight inflammation”, it deserves its own mention here as a very specific way of fighting it.
It’s never too late
All of the advices that go before a cancer diagnosis, continue to stand afterwards too. There is no point of “well, I already have cancer, so what’s the harm in…?”
The harm in it after a diagnosis will be the same as the harm before. When it comes to lifestyle, preventing a cancer and preventing it from spreading are very much the same thing, which is also the same as shrinking it. Basically, if it’s anticancer, it’s anticancer, no matter whether it’s before, during, or after.
Dr. Simmons has seen too many patients get a diagnosis, and place their lives squarely in the hands of doctors, when doctors can only do so much.
Instead, Dr. Simmons recommends taking charge of your health as best you are able, today and onwards, no matter what. And that means two things:
- Knowing stuff
- Doing stuff
So it becomes our responsibility (and our lifeline) to educate ourselves, and take action accordingly.
Want to know more?
We recently reviewed her book, and heartily recommend it:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Enjoy!
Share This Post
-
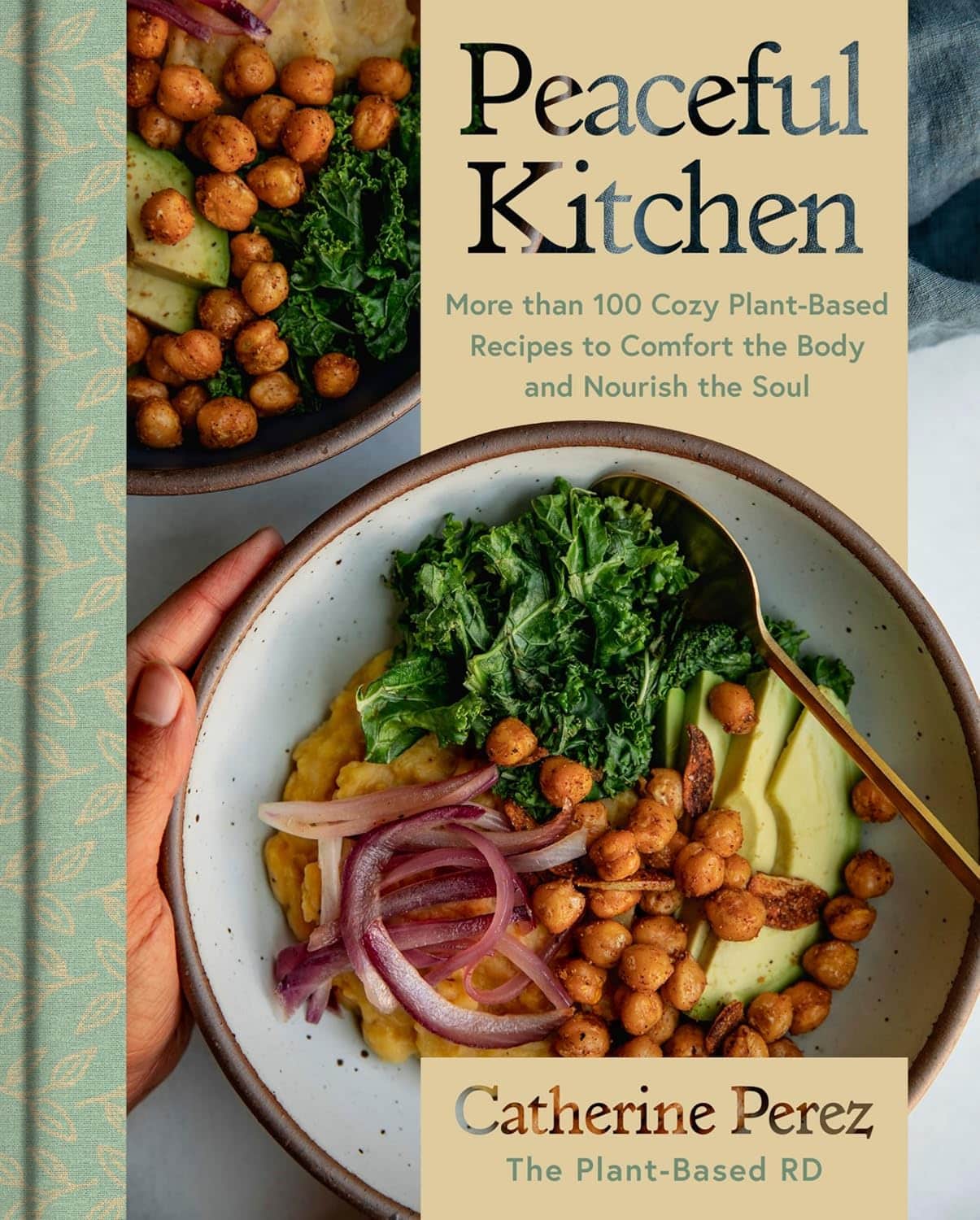
Peaceful Kitchen – by Catherine Perez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a keen cook and Registered Dietician with a Master’s in same, covers the basics of the science of nutrition as relevant to her recipes, but first and foremost this is not a science textbook—it’s a cookbook, and its pages contain more love for the art than citations for the (perfectly respectable) science.
Mexican and Dominican cuisine are the main influences in this book, but there are dishes from around the world too.
The recipes themselves are… Comparable in difficulty to the things we often feature in our recipes section here at 10almonds. They’re probably not winning any restaurants Michelin stars, but they’re not exactly student survival recipes either. They’re made from mostly non-obscure whole foods, nutritionally-dense ingredients at that, with minimal processed foods involved.
That said, she does take a “add, don’t subtract” approach to nutrition, i.e. focussing more on adding in diversity of plants than on “don’t eat this; don’t eat that” mandates.
If there’s any criticism to be levelled at the book, it’s that in most cases we’d multiply the spices severalfold, but that’s not a big problem as readers can always judge that individually; she’s given the basic information of which spices in which proportions, which is the key knowledge.
Bottom line: if you’re looking to expand your plant-based cooking repertoire, this one is a fine choice.
Click here to check out Peaceful Kitchen, and try some new things!
Share This Post
-
A Hospital Kept a Brain-Damaged Patient on Life Support to Boost Statistics. His Sister Is Now Suing for Malpractice.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
In 2018, Darryl Young was hoping for a new lease on life when he received a heart transplant at a New Jersey hospital after years of congestive heart failure. But he suffered brain damage during the procedure and never woke up.
The following year, a ProPublica investigation revealed that Young’s case was part of a pattern of heart transplants that had gone awry at Newark Beth Israel Medical Center in 2018. The spate of bad outcomes had pushed the center’s percentage of patients still alive one year after surgery — a key benchmark — below the national average. Medical staff were under pressure to boost that metric. ProPublica published audio recordings from meetings in which staff discussed the need to keep Young alive for a year, because they feared another hit to the program’s survival rate would attract scrutiny from regulators. On the recordings, the transplant program’s director, Dr. Mark Zucker, cautioned his team against offering Young’s family the option of switching from aggressive care to comfort care, in which no lifesaving efforts would be made. He acknowledged these actions were “very unethical.”
ProPublica’s revelations horrified Young’s sister Andrea Young, who said she was never given the full picture of her brother’s condition, as did the findings of a subsequent federal regulator’s probe that determined that the hospital was putting patients in “immediate jeopardy.” Last month, she filed a medical malpractice lawsuit against the hospital and members of her brother’s medical team.
The lawsuit alleges that Newark Beth Israel staff were “negligent and deviated from accepted standards of practice,” leading to Young’s tragic medical outcome.
Defendants in the lawsuit haven’t yet filed responses to the complaint in court documents. But spokesperson Linda Kamateh said in an email that “Newark Beth Israel Medical Center is one of the top heart transplant programs in the nation and we are committed to serving our patients with the highest quality of care. As this case is in active litigation, we are unable to provide further detail.” Zucker, who is no longer on staff at Newark Beth Israel, didn’t respond to requests for comment. His attorney also didn’t respond to calls and emails requesting comment.
Zucker also didn’t respond to requests for comment from ProPublica in 2018; Newark Beth Israel at the time said in a statement, made on behalf of Zucker and other staff, that “disclosures of select portions of lengthy and highly complex medical discussions, when taken out of context, may distort the intent of conversations.”
The lawsuit alleges that Young suffered brain damage as a result of severely low blood pressure during the transplant surgery. In 2019, when the federal Centers for Medicare and Medicaid Services scrutinized the heart transplant program following ProPublica’s investigation, the regulators found that the hospital had failed to implement corrective measures even after patients suffered, leading to further harm. For example, one patient’s kidneys failed after a transplant procedure in August 2018, and medical staff made recommendations internally to increase the frequency of blood pressure measurement during the procedure, according to the lawsuit. The lawsuit alleges that the hospital didn’t implement its own recommendations and that one month later, “these failures were repeated” in Young’s surgery, leading to brain damage.
The lawsuit also alleges that Young wasn’t asked whether he had an advance directive, such as a preference for a do-not-resuscitate order, despite a hospital policy stating that patients should be asked at the time of admission. The lawsuit also noted that CMS’ investigation found that Andrea Young was not informed of her brother’s condition.
Andrea Young said she understands that mistakes can happen during medical procedures, “however, it’s their duty and their responsibility to be honest and let the family know exactly what went wrong.” Young said she had to fight to find out what was going on with her brother, at one point going to the library and trying to study medical books so she could ask the right questions. “I remember as clear as if it were yesterday, being so desperate for answers,” she said.
Andrea Young said that she was motivated to file the lawsuit because she wants accountability. “Especially with the doctors never, from the outset, being forthcoming and truthful about the circumstances of my brother’s condition, not only is that wrong and unethical, but it took a lot away from our entire family,” she said. “The most important thing to me is that those responsible be held accountable.”
ProPublica’s revelation of “a facility putting its existence over that of a patient is a scary concept,” said attorney Jonathan Lomurro, who’s representing Andrea Young in this case with co-counsel Christian LoPiano. Besides seeking damages for Darryl Young’s children, “we want to call attention to this so it doesn’t happen again,” Lomurro said.
The lawsuit further alleges that medical staff at Newark Beth Israel invaded Young’s privacy and violated the Health Insurance Portability and Accountability Act, more commonly known as HIPAA, by sharing details of his case with the media without his permission. “We want people to be whistleblowers and want information out,” but that information should be told to patients and their family members directly, Lomurro said.
The 2019 CMS investigation determined that Newark Beth Israel’s program placed patients in “immediate jeopardy,” the most serious level of violation, and required the hospital to implement corrective plans. Newark Beth Israel did not agree with all of the regulator’s findings and in a statement at the time said that the CMS team lacked the “evidence, expertise and experience” to assess and diagnose patient outcomes.
The hospital did carry out the corrective plans and continues to operate a heart transplant program today. The most recent federal data, based on procedures from January 2021 through June 2023, shows that the one year probability of survival for a patient at Newark Beth is lower than the national average. It also shows that the number of graft failures, including deaths, in that time period was higher than the expected number of deaths for the program.
Andrea Young said she’s struggled with a feeling of emptiness in the years after her brother’s surgery. They were close and called each other daily. “There’s nothing in the world that can bring my brother back, so the only solace I will have is for the ones responsible to be held accountable,” she said. Darryl Young died on Sept 12, 2022, having never woken up after the transplant surgery.
A separate medical malpractice lawsuit filed in 2020 by the wife of another Newark Beth Israel heart transplant patient who died after receiving an organ infected with a parasitic disease is ongoing. The hospital has denied the allegations in court filing. The state of New Jersey, employer of the pathologists named in the case, settled for $1.7 million this month, according to the plaintiff’s attorney Christian LoPiano. The rest of the case is ongoing.
Share This Post
Related Posts
-
Two Awesome Hours – by Dr. Josh Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The brain is an amazing and powerful organ, with theoretically unlimited potential in some respects. So why doesn’t it feel that way a lot of the time?
The truth is that not only are we often tired, dehydrated, or facing other obvious physiological challenges to peak brain health, but also… We’re simply not making the best use of it!
What Dr. Davis does is outline for us how we can create the conditions for “two awesome hours” of effective mental performance by:
- Recognizing when to most effectively flip the switch on our automatic thinking
- Scheduling tasks based on their “processing demand” and recovery time
- Learning how to direct attention, rather than avoid distractions
- Feeding and moving our bodies in ways that prep us for success
- Identifying what matters in our environment to be at the top of our mental game
Why only two hours? Why not four, or eight, or more?
Well, our brains need recovery time too, so we can’t be “always on” and operating and peak efficiency. But, what we can do is optimize a couple of hours for absolute peak efficiency, and then enjoy the rest of time with lower cognitive-load activities.
Bottom line: if the idea of what you could accomplish if you could just be guaranteed two schedulable hours (your preference when!) of peak cognitive performance per day, then this is a great book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Blood Sugar Solution – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main purpose of this book is combating metabolic disease, the amalgam of what’s often prediabetes (sometimes fully-fledged diabetes) and cardiovascular disease (sometimes fully-fledged heart disease).
To achieve this (after an introductory section explaining what the sociomedical problems are and why the sociomedical problems are happening), he offers a seven-step program; we’ll not keep those steps a mystery; they are:
- Boost your nutrition
- Regulate your hormones
- Reduce inflammation
- Improve your digestion
- Maximize detoxification
- Enhance energy metabolism
- Soothe your mind
Thereafter, it’s all about leading the reader by the hand through the steps; he also offers a six-week action plan, and a six-week meal plan with recipes.
The style is very sensationalist (too sensationalist for this reviewer’s personal taste) but nevertheless backed up with hard science when it comes to hard claims. So, if you don’t mind wading through (or skipping) some early chapters that are a bit “used car salesman” in feel, there’s actually a lot of good information, especially in the middle of the book, and useful practical guides in the middle and end.
Bottom line: if you want a good comprehensive science-based practical guide to addressing the risk of metabolic disease, this is that.
Click here to check out The Blood Sugar Solution, and look after yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Heal & Reenergize Your Brain With Optimized Sleep Cycles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes 8 hours sleep can result in grogginess while 6 hours can result in waking up fresh as a daisy, so what gives? Dr. Tracey Marks explains, in this short video.
Getting more than Zs in
Sleep involves 90-minute cycles, usually in 4 stages:
- Stage 1: (drowsy state): brief muscle jerks; lasts a few minutes.
- Stage 2: (light sleep): sleep spindles for memory consolidation; 50% of total sleep.
- Stage 3 (deep sleep): tissue repair, immune support, brain toxin removal via the glymphatic system.
- Stage 4 (REM sleep): emotional processing, creativity, problem-solving, and dreaming.
Some things can disrupt some or all of those. To give a few common examples:
- Alcohol: impairs REM sleep.
- Caffeine: hinders deep sleep even if consumed hours before bed.
- Screentime: delays sleep onset due to blue light (but not by much); the greater problem is that it can also disrupt REM sleep due to mental stimulation.
To optimize things, Dr. Marks recommends:
- 90-minute rule: plan sleep to align with full cycles (e.g: 22:30 to 06:00 = 7½ hours, which is 5x 90-minute cycles).
- Smart alarms: use sleep-tracking apps with built-in alarm, to wake you up during light sleep phases.
- Strategic naps: keep naps to 20 minutes or a full 90-minute cycle.
- Pink noise: improves deep sleep.
- Meal timing: avoid eating within 3 hours of bedtime.
- Natural light: get morning light exposure in the morning to strengthen circadian rhythm.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Calculate (And Enjoy) The Perfect Night’s Sleep
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: