Syphilis Is Killing Babies. The U.S. Government Is Failing to Stop the Disease From Spreading.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Karmin Strohfus, the lead nurse at a South Dakota jail, punched numbers into a phone like lives depended on it. She had in her care a pregnant woman with syphilis, a highly contagious, potentially fatal infection that can pass into the womb. A treatment could cure the woman and protect her fetus, but she couldn’t find it in stock at any pharmacy she called — not in Hughes County, not even anywhere within an hour’s drive.
Most people held at the jail where Strohfus works are released within a few days. “What happens if she gets out before I’m able to treat her?” she worried. Exasperated, Strohfus reached out to the state health department, which came through with one dose. The treatment required three. Officials told Strohfus to contact the federal Centers for Disease Control and Prevention for help, she said. The risks of harm to a developing baby from syphilis are so high that experts urge not to delay treatment, even by a day.
Nearly three weeks passed from when Strohfus started calling pharmacies to when she had the full treatment in hand, she said, and it barely arrived in time. The woman was released just days after she got her last shot.
Last June, Pfizer, the lone U.S. manufacturer of the injections, notified the Food and Drug Administration of an “impending stock out” that it anticipated would last a year. The company blamed “an increase in syphilis infection rates as well as competitive shortages.”
Across the country, physicians, clinic staff and public health experts say that the shortage is preventing them from reining in a surge of syphilis and that the federal government is downplaying the crisis. State and local public health authorities, which by law are responsible for controlling the spread of infectious diseases, report delays getting medicine to pregnant people with syphilis. This emergency was predictable: There have been shortages of this drug in eight of the last 20 years.
Yet federal health authorities have not prevented the drug shortages in the past and aren’t doing much to prevent them in the future.
Syphilis, which is typically spread during sex, can be devastating if it goes untreated in pregnancy: About 40% of babies born to women with untreated syphilis can be stillborn or die as newborns, according to the CDC. Infants that survive can suffer from deformed bones, excruciating pain or brain damage, and some struggle to hear, see or breathe. Since this is entirely preventable, a baby born with syphilis is a shameful sign of a failing public health system.
In 2022, the most recent year for which the CDC has data available, more than 3,700 babies were infected with syphilis, including nearly 300 who were stillborn or died as infants. More than 50% of these cases occurred because, even though the pregnant parent was diagnosed with syphilis, they were never properly treated.
That year, there were 200,000 cases identified in the U.S., a 79% increase from five years before. Infection rates among pregnant people and babies increased by more than 250% in that time; South Dakota, where Strohfus works, had the highest rates — including a more than 400% increase among pregnant women. Statewide, the rate of babies born with the disease, a condition known as congenital syphilis, jumped more than 40-fold in just five years.
And that was before the current shortage of shots.
In Mississippi, the state with the second highest rate of syphilis in pregnant women, Dr. Caroline Weinberg started having trouble this summer finding treatments for her clinic’s patients, most of whom are uninsured, live in poverty or lack transportation. She began spending hours each month scouring medicine suppliers’ websites for available doses of the shots, a form of penicillin sold under the brand name Bicillin L-A.
“The way people do it for Taylor Swift, that’s how I’ve been with the Bicillin shortage,” Weinberg said. “Desperately checking the websites to see what I can snag.”
The shortage is driving up infection rates even further.
In a November survey by the National Coalition of STD Directors, 68% of health departments that responded said the drug shortage will cause syphilis rates in their area to increase, further crushing the nation’s most disadvantaged populations.
“This is the most basic medicine,” said Meghan O’Connell, chief public health officer for the Great Plains Tribal Leaders’ Health Board, which represents 18 tribal communities in South Dakota and three other states. “We allow ourselves to continue to not have enough, and it impacts so many people.”
ProPublica examined what the federal government has done to manage the crisis and the ways in which experts say it has fallen short.
The government could pressure Pfizer to be more transparent.
Twenty years ago, there were at least three manufacturers of the syphilis shot. Then Pfizer, one of the manufacturers, purchased the other two companies and became the lone U.S. supplier.
Pfizer’s supply has fallen short since then. In 2016, the company announced a shortage due to a manufacturing issue; it lasted two years. Even during times when Pfizer had not notified the FDA of an official shortage, clinics across the country told ProPublica, the shots were often hard to get.
Several health officials said they would like to see the government use its power as the largest purchaser of the drug to put pressure on Pfizer to produce adequate supplies and to be more transparent about how much of the drug they have on hand, when it will be widely available and how stable the supply will be going forward.
In response to questions, Pfizer said there are two reasons its supply is falling short. One, the company said, was a surge in use of the pediatric form of the drug after a shortage of a different antibiotic last winter. Pfizer also blamed a 70% increase in demand for the adult shots since last February, which it described as unexpected.
Public health experts say the increase in cases and subsequent rise in demand was easy to see coming. Officials have been raising the alarm about skyrocketing syphilis cases for years. “If Pfizer was truly caught completely off guard, it raises significant questions about the competency of the company to forecast obvious infectious disease trends,” a coalition of organizations wrote to the White House Drug Shortage Task Force in September.
Pfizer said it is consistently communicating with the CDC and FDA about its supply and that it has been transparent with public health groups and policymakers.
The FDA has a group dedicated to addressing drug shortages. But Valerie Jensen, associate director of that staff, said the FDA can’t force manufacturers to make more of a drug. “It is up to manufacturers to decide how to respond to that increased demand.” she said. “What we’re here to do is help with those plans.”
Pfizer said it had a target of increasing production by about 20% in 2023 but faced delays toward the end of the year. The company did not explain the reason for those delays.
The company said it has invested $38 million in the last five years in the Michigan facility where it makes the shots and that it is increasing production capacity. It also said it is adding evening shifts at the facility and actively recruiting and training new workers. Pfizer said it also reduced manufacturing time from 110 to 50 days. By the end of June, the company expects the supply to recover, which it described as having eight weeks of inventory based on its forecast demands with no disruptions in sight.
The government could manufacture the drug itself.
Having only one supplier for a drug, especially one of public health importance, makes the country vulnerable to shortages. With just one manufacturer, any disruption — contamination at a plant, a shortage of raw materials, a severe weather event or a flawed prediction of demand — can put lives at risk. What’s ultimately needed, public health experts say, is another manufacturer.
Congressional Democrats recently introduced a bill that would authorize the U.S. Department of Health and Human Services to manufacture generic drugs in exactly this scenario, when there are few manufacturers and regular shortages. Called the Affordable Drug Manufacturing Act, it would also establish an office of drug manufacturing.
This same bill was introduced in 2018, but it didn’t have bipartisan support and was never taken up for a vote. Sen. Elizabeth Warren, the Massachusetts Democrat who introduced the bill in the Senate, said she’s hopeful this time will be different. Lawmakers from both parties understand the risks created by drug shortages, and COVID-19 helped everyone understand the role the government can play to boost manufacturing.
Still, it’s unlikely to be passed with the current gridlock in Congress.
The government could reserve syphilis drugs for infected patients.
Responding to the shortage of shots to treat the disease, the CDC in July asked health care providers nationwide to preserve the scarce remaining doses for people who are pregnant. The shots are considered the gold standard treatment for anyone with syphilis, faster and with fewer side effects than an alternative pill regimen. And for people who are pregnant, the pills are not an option; the shots are the only safe treatment.
Despite that call, the military is giving shots to new recruits who don’t have syphilis, to prevent outbreaks of severe bacterial respiratory infections. The Army has long administered this treatment at boot camps held at Fort Leonard Wood, Fort Moore and Fort Sill. The Army has been unable to obtain the shots several times in the past few years, according to the U.S. Army Center for Initial Military Training. But the Defense Health Agency’s pharmacy operations center has been working with Pfizer to ensure military sites can get them, a spokesperson for the Defense Health Agency said.
“Until we think about public health the way we think about our military, we’re not going to see a difference,” said Dr. John Vanchiere, chief of pediatric infectious diseases at Louisiana State University Health Shreveport.
Some public health officials, including Alaska’s chief medical officer, Dr. Anne Zink, questioned whether the military should be using scarce shots for prevention.
“We should ask if that’s the best use,” she said.
Using antibiotics to prevent streptococcal outbreaks is a well-established, evidence-based public health practice that’s also used by other branches of the armed services, said Lt. Col. Randy Ready, a public affairs officer with the Army’s Initial Military Training center. “The Army continues to work with the CDC and the entire medical community in regards to public health while also taking into account the unique missions and training environments our Soldiers face,” including basic training, Ready said in a written statement.
The government isn’t stockpiling syphilis drugs.
In rare instances, the federal government has created stockpiles of drugs considered key to public health. In 2018, confronting shortages of various drugs to treat tuberculosis, the CDC created a small stockpile of them. And the federal Administration for Strategic Preparedness and Response keeps a national stockpile of supplies necessary for public health emergencies, including vaccines, medical supplies and antidotes needed in case of a chemical warfare attack.
In November, the Biden administration announced it was creating a new syphilis task force. When asked why the federal government doesn’t stockpile syphilis treatments, Adm. Rachel Levine, the HHS official who leads the task force, said officials don’t routinely stockpile drugs, because they have expiration dates.
In a written statement, an HHS spokesperson said that Bicillin has a shelf life of two years and that the Strategic National Stockpile “does not deploy products that are commercially available.” In general, the spokesperson wrote, stockpiles are most effective before a national shortage begins and can’t overcome the problems of limited suppliers or fragile supply chains. “There is also a risk that stockpiles can exacerbate shortages, particularly when supply is already low, by removing drugs from circulation that would have otherwise been available,” the spokesperson wrote.
Stephanie Pang, a senior director with the coalition of STD directors, said that given the critical role of this drug and the severe access concerns, she thinks a stockpile is necessary. “I don’t have another solution that actually gets drugs to patients,” Pang said.
The government could declare a federal emergency.
Some public health officials say the federal government needs to treat the syphilis crisis the way it did Ebola or monkeypox.
Declare a federal emergency, said Dr. Michael Dube, an infectious disease specialist for more than 30 years. That would free up money for more public health staff and fund more creative approaches that could lead to a long-term solution to the near-constant shortages, he said. “I’d hate to have to wait for some horrible anecdotes to get out there in order to get the public’s and the policymakers’ minds on it,” said Dube, who oversees medical care for AIDS Healthcare Foundation wellness clinics across the country.
Citing an alarming surge in syphilis cases, the Great Plains Tribes wrote to the HHS secretary last week asking that the agency declare a public health emergency in their areas. In the request, they asked HHS to work globally to find adequate syphilis treatment and send the needed medicine to the Great Plains region.
During the 2014 outbreak of Ebola in West Africa, Congress gave hundreds of millions of dollars to HHS to help develop new rapid tests and vaccines. Facing a global outbreak of monkeypox in 2022, a White House task force deployed more than a million vaccines, regularly briefed the public and sent extra resources to Pride parades and other places where people at risk were gathered.
Levine, leader of the federal syphilis task force, countered that declaring an emergency wouldn’t make much of a difference. The government, she said, already has a “dramatic and coordinated response” involving several agencies.
The FDA recently approved an emergency import of a similar syphilis treatment made by a French manufacturer that had plenty on hand. According to the company, Provepharm, the imported shots are enough to cover approximately one or two months of typical use by all people in the U.S. (The FDA would not say how many doses Provepharm sent, and the company said it was not allowed to reveal that number under the federal rules governing such emergency imports.)
Clinics applaud that development. But many of them can’t afford the imported shots.
The government could do more to rein in the cost.
Clinics and hospitals that primarily serve low-income patients often qualify for a federal program that allows them to purchase drugs at steeply discounted prices. Pharmaceutical companies that want Medicaid to cover their outpatient drugs must participate in the program.
One factor in determining the discount price is whether a pharmaceutical company has raised the price of a drug by more than the rate of inflation. Because Pfizer has hiked the price of its Bicillin shots significantly over the years, the government requires that it be sold to qualifying clinics for just pennies a dose. Otherwise, a single Pfizer shot can retail for upwards of $500. The French shots are comparable in retail price and not eligible for the discount program.
Several clinic directors also said they worried that drug distributors were reserving the limited supply of the Pfizer shot for organizations that could pay full price. For several days in January, for example, the website of Henry Schein, a medical supplier, showed doses of the shot available at full price, while doses at the penny pricing were out of stock, according to screenshots shared with ProPublica. When asked whether it was only selling shots at full price, a spokesperson for Henry Schein did not respond to the question.
Local health departments that qualify for the discount program told ProPublica they’ve had to pay full price at other distributors, because it was the only stock available.
The Health Resources and Services Administration, the federal agency that regulates the discount program, said that a drug manufacturer is ultimately responsible for ensuring that when supplies are available, they are available at the discounted price. When asked about this, Pfizer said that it has “one inventory that is distributed to our trade partners” and that hospitals and clinics that qualify for the discount program are “responsible for ensuring compliance with the program and orders through the wholesaler accordingly.” The company added, “Pfizer plays no part in this process.”
In October, on Weinberg’s regular search for shots for her Mississippi clinic, she found doses of Bicillin for sale at the discounted price and purchased 40. “The idea that we’re supposed to be hoarding treatment is a horrific compact,” she said. Word got out that the clinic, called Plan A, has some shots, and other clinics began sending pregnant patients there.
The clinic’s supply is dwindling. Weinberg is happy to get the shots to patients who need them. But she’s not sure how much longer her reserve will last — or if she’ll be able to find more when they’re gone.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Maximize Your Misery! (7 Great Methods)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s imagine that instead of being healthily fulfilled in life, you wanted to spend your days as miserable as possible. What should you do?
Here are a few pointers:
Stay still
Avoid physical activity and/or outdoor exposure, to avoid any mood-lifting neurochemicals. In fact, remain indoors as much as possible, preferably in the same room.
If you want to absolutely maximize your misery, make your bedroom the sole space for all activities that it’s possible to do there.
Disrupt your sleep
Keep an irregular sleep schedule by varying your bedtime and wake-up times frequently. Sleep in as much as possible, and make up for it by staying up late to ensure ongoing exhaustion.
Maximize screentime
Use digital entertainment as much as possible to distract you from meaningful activities and rest—as a bonus, this will also help you to avoid self-reflection.
Begin and end your day with a device in hand.
Fuel negative emotions
If you’re going to focus on something, focus on problems you cannot control, to stoke the fires of anger and angst.
A good way of doing this is by staying informed about distressing events, while avoiding meaningful actions to address them. Contribute only in token gestures, and then lament the lack of change.
Follow your impulses
Act on short-term desires without considering long-term consequences, while avoiding behaviors that you know might improve your mood or wellbeing.
Trust that doing the same things that have not previously resulted in happiness, will continue to reliably deliver unhappiness.
Set goals to miss
It’s important that your goals should be vague, and overly ambitious in their scope and/or deliverability. Ideally you should also disregard any preparatory work that a person would normally do before embarking on such a project.
Bonus tip: you can further sabotage any chances of progress, by waiting for motivation to strike before you take any action.
Pursue happiness
Focus on chasing happiness itself, instead of improving your situation or skills. Treat happiness as an end goal, instead of a by-product of worthwhile activities.
Want to learn more?
If you’d like to know many more ways to be miserable, we featured these 7 from this book of 40, which we haven’t reviewed yet, but probably will one of these days:
How to Be Miserable: 40 Strategies You Already Use – by Dr. Randy Paterson
Alternatively…
If for some strange reason you’d rather not do those things, you might consider a previous article of ours:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Enjoy!
Share This Post
-
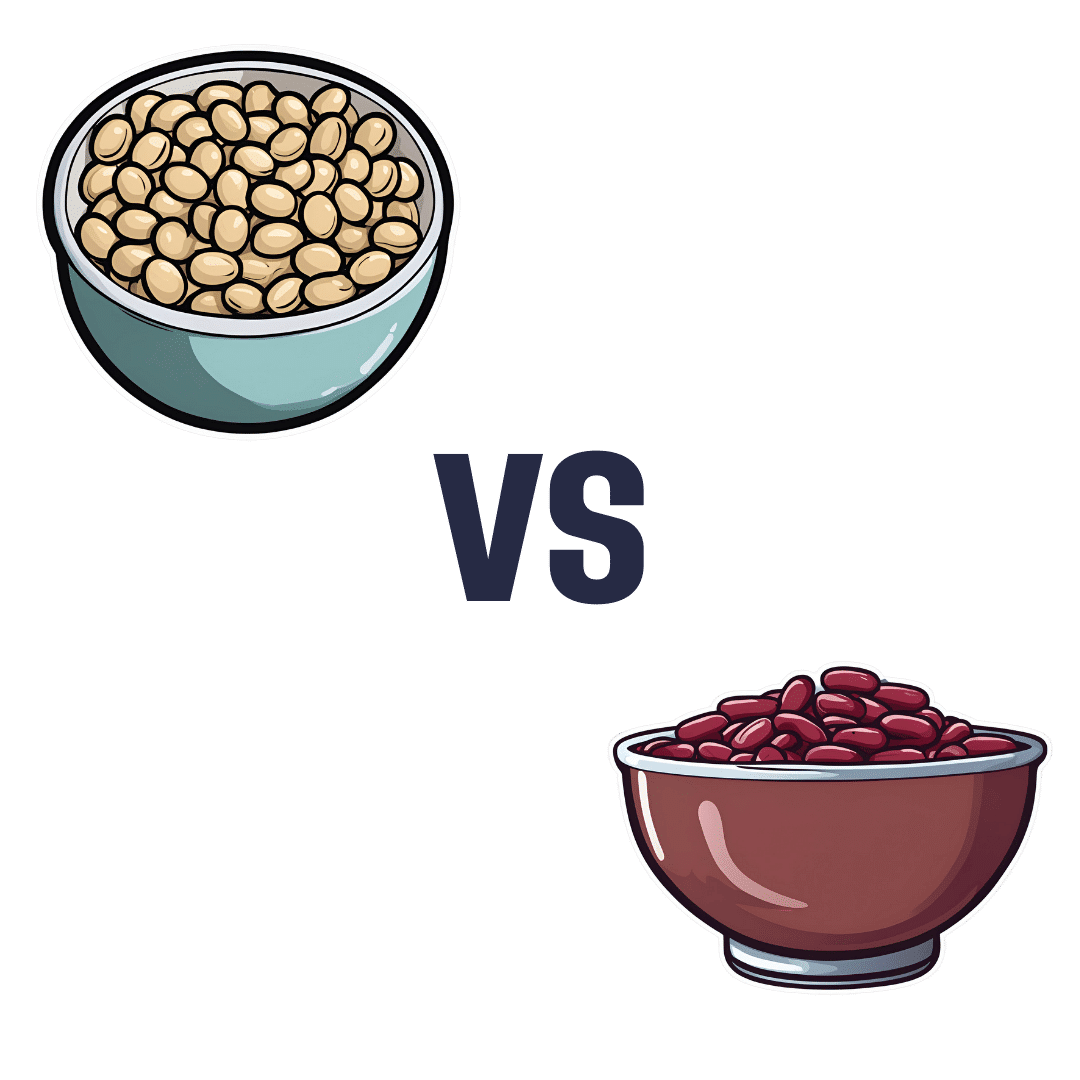
Soy Beans vs Kidney Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soy beans to kidney beans, we picked the soy.
Why?
In terms of macros, soy has 2x the protein, while kidney beans have nearly 3x the carbs and very slightly more fiber. Ratio-wise, the “very slightly more fiber” does not offset the “nearly 3x the carbs” when it comes to glycemic index (though both are still good, really, but this is a head-to-head so the comparison is relevant), and 2x the protein is also quite a bonus, so this category’s an easy win for soy.
In the category of vitamins, soy beans have more of vitamins A, B2, B6, C, E, K, and choline, while kidney beans have more of vitamins B3, B5, and B9, thus making for a 7:3 win for soy.
When it comes to minerals, soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while kidney beans are not higher in any mineral. Another clear win for soy.
Adding up the three strong wins for soy, makes for an overall easy win for soy. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Plant vs Animal Protein: Head to Head
Take care!
Share This Post
-
Relieve GERD and Acid Reflux with Stretches and Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Looking for relief from GERD or acid reflux? Today we’re featuring an amazing video by Dr. Jo, packed with stretches and exercises designed to ease those symptoms.
Here’s a quick rundown, in case you don’t have time to watch the whole video.
If you’re not familiar with GERD, you can find our simple explanation of GERD here. Or, if you’re on the other end of the spectrum and want to do a deeper dive on the topic, we reviewed a great book on the topic).
1. Mobilize Your SEM Muscle
The sternocleidomastoid (SEM) muscle, if tight, can aggravate acid reflux. Dr. Jo shows how to gently mobilize this muscle by turning your head while holding the SEM in place. It’s simple but effective.
2. Portrait Pose Stretch
Stretch out that SEM with the Portrait Pose. Place your hand on your collarbone, turn your head away, side bend, and look up. Hold for 30 seconds. You’ll feel the tension melting away.
3. Seated Cat-Cow Motion
Open up your stomach area with this easy exercise. Sit down, roll your body forward, arch your back (Cow), then curl your spine and tuck your chin (Cat). Alternate for 30 seconds and feel the difference.
4. Quadruped Cat-Cow with Breathing
Similar to the seated cat-cow, the quadruped cat-cow focuses on flexing the lower spine whilst on all fours. Bonus tip: focus on deep belly breathing during the exercise. This helps improve digestion and ease reflux symptoms.
5. Exaggerated Pelvic Tilt
Lie on your back and tilt your pelvis back and forth. This loosens up the abdominal area and helps everything flow better.
6. Trunk Rotation
Lie down, bend your knees, and rotate them to one side. Hold for 30 seconds, then switch sides. It’s a great way to relax and stretch your abdominal muscles.
We know this is a quick overview (sorry if it seems rushed!), but if you have a few more minutes on your hand you can watch the whole video below.
Feel better soon! And if you have any favorite tips or videos to share, email us at 10almonds.
Share This Post
Related Posts
-
Why do disinfectants only kill 99.9% of germs? Here’s the science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever wondered why most disinfectants indicate they kill 99.9% or 99.99% of germs, but never promise to wipe out all of them? Perhaps the thought has crossed your mind mid-way through cleaning your kitchen or bathroom.
Surely, in a world where science is able to do all sorts of amazing things, someone would have invented a disinfectant that is 100% effective?
The answer to this conundrum requires understanding a bit of microbiology and a bit of mathematics.
Davor Geber/Shutterstock What is a disinfectant?
A disinfectant is a substance used to kill or inactivate bacteria, viruses and other microbes on inanimate objects.
There are literally millions of microbes on surfaces and objects in our domestic environment. While most microbes are not harmful (and some are even good for us) a small proportion can make us sick.
Although disinfection can include physical interventions such as heat treatment or the use of UV light, typically when we think of disinfectants we are referring to the use of chemicals to kill microbes on surfaces or objects.
Chemical disinfectants often contain active ingredients such as alcohols, chlorine compounds and hydrogen peroxide which can target vital components of different microbes to kill them.
Diseinfectants can contain a range of ingredients. Maridav/Shutterstock The maths of microbial elimination
In the past few years we’ve all become familiar with the concept of exponential growth in the context of the spread of COVID cases.
This is where numbers grow at an ever-accelerating rate, which can lead to an explosion in the size of something very quickly. For example, if a colony of 100 bacteria doubles every hour, in 24 hours’ time the population of bacteria would be more than 1.5 billion.
Conversely, the killing or inactivating of microbes follows a logarithmic decay pattern, which is essentially the opposite of exponential growth. Here, while the number of microbes decreases over time, the rate of death becomes slower as the number of microbes becomes smaller.
For example, if a particular disinfectant kills 90% of bacteria every minute, after one minute, only 10% of the original bacteria will remain. After the next minute, 10% of that remaining 10% (or 1% of the original amount) will remain, and so on.
Because of this logarithmic decay pattern, it’s not possible to ever claim you can kill 100% of any microbial population. You can only ever scientifically say that you are able to reduce the microbial load by a proportion of the initial population. This is why most disinfectants sold for domestic use indicate they kill 99.9% of germs.
Other products such as hand sanitisers and disinfectant wipes, which also often purport to kill 99.9% of germs, follow the same principle.
You might have noticed none of the cleaning products in your laundry cupboard kill 100% of germs. Africa Studio/Shutterstock Real-world implications
As with a lot of science, things get a bit more complicated in the real world than they are in the laboratory. There are a number of other factors to consider when assessing how well a disinfectant is likely to remove microbes from a surface.
One of these factors is the size of the initial microbial population that you’re trying to get rid of. That is, the more contaminated a surface is, the harder the disinfectant needs to work to eliminate the microbes.
If for example you were to start off with only 100 microbes on a surface or object, and you removed 99.9% of these using a disinfectant, you could have a lot of confidence that you have effectively removed all the microbes from that surface or object (called sterilisation).
In contrast, if you have a large initial microbial population of hundreds of millions or billions of microbes contaminating a surface, even reducing the microbial load by 99.9% may still mean there are potentially millions of microbes remaining on the surface.
Time is is a key factor that determines how effectively microbes are killed. So exposing a highly contaminated surface to disinfectant for a longer period is one way to ensure you kill more of the microbial population.
This is why if you look closely at the labels of many common household disinfectants, they will often suggest that to disinfect you should apply the product then wait a specified time before wiping clean. So always consult the label on the product you’re using.
Disinfectants won’t necessarily work in your kitchen exactly like they work in a lab. Ground Picture/Shutterstock Other factors such as temperature, humidity and the type of surface also influence how well a disinfectant works outside the lab.
Similarly, microbes in the real world may be either more or less sensitive to disinfection than those used for testing in the lab.
Disinfectants are one part infection control
The sensible use of disinfectants plays an important role in our daily lives in reducing our exposure to pathogens (microbes that cause illness). They can therefore reduce our chances of getting sick.
The fact disinfectants can’t be shown to be 100% effective from a scientific perspective in no way detracts from their importance in infection control. But their use should always be complemented by other infection control practices, such as hand washing, to reduce the risk of infection.
Hassan Vally, Associate Professor, Epidemiology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not to Age – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: it’s a great book, and it’s this reviewer’s favorite of Dr. Greger’s so far (for posterity: it’s just been published and this reviewer has just finished reading the copy she got on pre-order)
Unlike many popular physician authors, Dr. Greger doesn’t rehash a lot of old material, and instead favours prioritizing new material in each work. Where appropriate, he’ll send the reader to other books for more specific information (e.g: you want to know how to avoid premature death? Go read How Not To Die. You want to know how to lose weight? How Not To Diet. Etc).
In the category of new information, he has a lot to offer here. And with over 8,000 references, it’s information, not conjecture. On which note, we recommend the e-book version if that’s possible for you, for three reasons:
- It’s possible to just click the references and be taken straight to the cited paper itself online
- To try to keep the book’s size down, Dr. Greger has linked to other external resources too
- The only negative reviews on Amazon, so far, are people complaining that the print copy’s text is smaller than they’d like
For all its information-density (those 8,000+ references are packed into 600ish pages), the book is very readable even to a lay reader; the author is a very skilled writer.
As for the content, we can’t fit more than a few sentences here so forgive the brevity, but we’ll mention that he covers:
- Slowing 11 pathways of aging
- The optimal anti-aging regimen according to current best science
- Preserving function (specific individual aspects of aging, e.g. hearing, sight, cognitive function, sexual function, hair, bones, etc)
- “Dr. Greger’s Anti-Aging Eight”
In terms of “flavor” of anti-aging science, his approach can be summed up as: diet and lifestyle as foundation; specific supplements and interventions as cornerstones.
Bottom line: this is now the anti-aging book.
Click here to check out How Not To Age, and look after yourself with the best modern science!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 Secrets Behind The Healing Power Of Plants
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-established that whole food plant-based diets including fruits, vegetables, beans, whole grains, nuts, and seeds can reverse chronic diseases like type 2 diabetes, hypertension, high cholesterol, obesity, and more.
Dr. Laurie Marbas explains how it works:
Three ways plant-based diets heal
There’s a lot to be said for plants, from their fiber to their beneficial phytochemicals. For example:
Reversing insulin resistance: plant-based diets help reverse insulin resistance, a major factor in type 2 diabetes, heart disease, obesity, and many other maladies. Particularly high-fiber foods like beans and oats stabilize blood sugar by slowing sugar absorption and reducing insulin spikes. These diets are also naturally low in saturated fats, which are linked to insulin resistance, and include phytonutrients from colorful fruits and vegetables that improve insulin sensitivity. Studies demonstrate that plant-based diets lower HbA1C levels (glycated hemoglobin, a measure of how sugary your blood has been on average in the past 2−3 months) and can even reverse type 2 diabetes for most* people.
*Scientists are very reluctant to claim absolutes such as “all”, “every”, etc, since it cannot be proven that it will work for all people (there are over 8 billion of us after all, and any one of us could get in theory get type 2 diabetes and then try reversing it, so it’s hard to speak for all 8 billion-odd of us) but it is well-established that it usually does indeed reverse it, and for what it’s worth, the confidence interval in such studies is always at least 95% sure, usually higher, which multiplied by countless studies can indeed give us quite some confidence.
Reducing chronic inflammation: chronic inflammation, linked to diseases like arthritis, heart disease, and cancer, can also be reduced through a plant-based diet. Foods rich in antioxidants, such as berries, leafy greens, and nuts, neutralize inflammation-causing free radicals. Omega-3-rich plant foods like chia seeds, flax seeds, and walnuts further balance inflammation. Additionally, fiber fosters healthy gut bacteria, which produce vital compounds that reduce systemic inflammation (and do a lot more good things besides, but we’re limiting ourselves to talking about inflammation here). Research shows that plant-based diets can significantly lower inflammation markers within weeks (almost certainly you’ll notice the difference yourself, too).
Synergy of whole foods: perhaps the biggest power of a plant-based diet lies in the synergy of its components. Nutrients like the fiber and phytonutrients we mentioned work together to combat inflammation and remove waste products that could fuel disease. For example, magnesium, found abundantly in leafy greens (which is why most Americans are deficient in magnesium), supports over 300 enzymatic processes, including blood sugar and inflammation regulation. This holistic approach ensures the whole body receives all the tools it needs to repair, regenerate, and thrive, thus once you’re on the right track, it’s “the gift that keeps on giving” when it comes to health, as each part helps the other parts to work better, which help the other parts to work better, which… (etc)
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: