Forget Ringing the Button for the Nurse. Patients Now Stay Connected by Wearing One.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HOUSTON — Patients admitted to Houston Methodist Hospital get a monitoring device about the size of a half-dollar affixed to their chest — and an unwitting role in the expanding use of artificial intelligence in health care.
The slender, battery-powered gadget, called a BioButton, records vital signs including heart and breathing rates, then wirelessly sends the readings to nurses sitting in a 24-hour control room elsewhere in the hospital or in their homes. The device’s software uses AI to analyze the voluminous data and detect signs a patient’s condition is deteriorating.
Hospital officials say the BioButton has improved care and reduced the workload of bedside nurses since its rollout last year.
“Because we catch things earlier, patients are doing better, as we don’t have to wait for the bedside team to notice if something is going wrong,” said Sarah Pletcher, system vice president at Houston Methodist.
But some nurses fear the technology could wind up replacing them rather than supporting them — and harming patients. Houston Methodist, one of dozens of U.S. hospitals to employ the device, is the first to use the BioButton to monitor all patients except those in intensive care, Pletcher said.
“The hype around a lot of these devices is they provide care at scale for less labor costs,” said Michelle Mahon, a registered nurse and an assistant director of National Nurses United, the profession’s largest U.S. union. “This is a trend that we find disturbing,” she said.
The rollout of BioButton is among the latest examples of hospitals deploying technology to improve efficiency and address a decades-old nursing shortage. But that transition has raised its own concerns, including about the device’s use of AI; polls show the public is wary of health providers relying on it for patient care.
In December 2022 the FDA cleared the BioButton for use in adult patients who are not in critical care. It is one of many AI tools now used by hospitals for tasks like reading diagnostic imaging results.
In 2023, President Joe Biden directed the Department of Health and Human Services to develop a plan to regulate AI in hospitals, including by collecting reports of patients harmed by its use.
The leader of BioIntelliSense, which developed the BioButton, said its device is a huge advance compared with nurses walking into a room every few hours to measure vital signs. “With AI, you now move from ‘I wonder why this patient crashed’ to ‘I can see this crash coming before it happens and intervene appropriately,’” said James Mault, CEO of the Golden, Colorado-based company.
The BioButton stays on the skin with an adhesive, is waterproof, and has up to a 30-day battery life. The company says the device — which allows providers to quickly notice deteriorating health by recording more than 1,000 measurements a day per patient — has been used on more than 80,000 hospital patients nationwide in the past year.
Hospitals pay BioIntelliSense an annual subscription fee for the devices and software.
Houston Methodist officials would not reveal how much the hospital pays for the technology, though Pletcher said it equates to less than a cup of coffee a day per patient.
For a hospital system that treats thousands of patients at a time — Houston Methodist has 2,653 non-ICU beds at its eight Houston-area hospitals — such an investment could still translate to millions of dollars a year.
Hospital officials say they have not made any changes in nurse staffing and have no plans to because of implementing the BioButton.
Inside the hospital’s control center for virtual monitoring on a recent morning, about 15 nurses and technicians dressed in scrubs sat in front of large monitors showing the health status of hundreds of patients they were assigned to monitor.
A red checkmark next to a patient’s name signaled the AI software had found readings trending outside normal. Staff members could click into a patient’s medical record, showing patients’ vital signs over time and other medical history. These virtual nurses, if you will, could contact nurses on the floor by phone or email, or even dial directly into the patient’s room via video call.
Nutanben Gandhi, a technician who was watching 446 patients on her monitor that morning, said that when she gets an alert, she looks at the patient’s health record to see if the anomaly can be easily explained by something in the patient’s condition or if she needs to contact nurses on the patient’s floor.
Oftentimes an alert can be easily dismissed. But identifying signs of deteriorating health can be tough, said Steve Klahn, Houston Methodist’s clinical director of virtual medicine.
“We are looking for a needle in a haystack,” he said.
Donald Eustes, 65, was admitted to Houston Methodist in March for prostate cancer treatment and has since been treated for a stroke. He is happy to wear the BioButton.
“You never know what can happen here, and having an extra set of eyes looking at you is a good thing,” he said from his hospital bed. After being told the device uses AI, the Montgomery, Texas, man said he has no problem with its helping his clinical team. “This sounds like a good use of artificial intelligence.”
Patients and nurses alike benefit from remote monitoring like the BioButton, said Pletcher of Houston Methodist.
The hospital has placed small cameras and microphones inside all patient rooms enabling nurses outside to communicate with patients and perform tasks such as helping with patient admissions and discharge instructions. Patients can include family members on the remote calls with nurses or a doctor, she said.
Virtual technology frees up on-duty nurses to provide more hands-on help, such as starting an intravenous line, Pletcher said. With the BioButton, nurses can wait to take routine vital signs every eight hours instead of every four, she said.
Pletcher said the device reduces nurses’ stress in monitoring patients and allows some to work more flexible hours because virtual care can be done from home rather than coming to the hospital. Ultimately it helps retain nurses, not drive them away, she said.
Sheeba Roy, a nurse manager at Houston Methodist, said some members of the nursing staff were nervous about relying on the device and not checking patients’ vital signs as often themselves. But testing has shown the device provides accurate information.
“After we implemented it, the staff loves it,” Roy said.
Serena Bumpus, chief executive officer of the Texas Nurses Association, said her concern with any technology is that it can be more burdensome on nurses and take away time with patients.
“We have to be hypervigilant in ensuring that we are not leaning on this to replace the ability of nurses to critically think and assess patients and validate what this device is telling us is true,” Bumpus said.
Houston Methodist this year plans to send the BioButton home with patients so the hospital can better track their progress in the weeks after discharge, measuring the quality of their sleep and checking their gait.
“We are not going to need less nurses in health care, but we have limited resources and we have to use those as thoughtfully as we can,” Pletcher said. “Looking at projected demand and seeing the supply we have coming, we will not have enough to meet demand, so anything we can do to give time back to nurses is a good thing.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
America Worries About Health Costs — And Voters Want to Hear From Biden and Republicans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
President Joe Biden is counting on outrage over abortion restrictions to help drive turnout for his reelection. Former President Donald Trump is promising to take another swing at repealing Obamacare.
But around America’s kitchen tables, those are hardly the only health topics voters want to hear about in the 2024 campaigns. A new KFF tracking poll shows that health care tops the list of basic expenses Americans worry about — more than gas, food, and rent. Nearly 3 in 4 adults — and majorities of both parties — say they’re concerned about paying for unexpected medical bills and other health costs.
“Absolutely health care is something on my mind,” Rob Werner, 64, of Concord, New Hampshire, said in an interview at a local coffee shop in January. He’s a Biden supporter and said he wants to make sure the Affordable Care Act, also known as Obamacare, is retained and that there’s more of an effort to control health care costs.
The presidential election is likely to turn on the simple question of whether Americans want Trump back in the White House. (Nikki Haley, the former South Carolina governor and U.S. ambassador to the United Nations, remained in the race for the Republican nomination ahead of Super Tuesday, though she had lost the first four primary contests.) And neither major party is basing their campaigns on health care promises.
But in the KFF poll, 80% of adults said they think it’s “very important” to hear presidential candidates talk about what they’d do to address health care costs — a subject congressional and state-level candidates can also expect to address.
“People are most concerned about out-of-pocket expenses for health care, and rightly so,” said Andrea Ducas, vice president of health policy at the Center for American Progress, a Washington, D.C.-based progressive think tank.
Here’s a look at the major health care issues that could help determine who wins in November.
Abortion
Less than two years after the Supreme Court overturned the constitutional right to an abortion, it is shaping up to be the biggest health issue in this election.
That was also the case in the 2022 midterm elections, when many voters rallied behind candidates who supported abortion rights and bolstered Democrats to an unexpectedly strong showing. Since the Supreme Court’s decision, voters in six states — including Kansas, Kentucky, and Ohio, where Republicans control the legislatures — have approved state constitutional amendments protecting abortion access.
Polls show that abortion is a key issue to some voters, said Robert Blendon, a public opinion researcher and professor emeritus at the Harvard T.H. Chan School of Public Health. He said up to 30% across the board see it as a “personal” issue, rather than policy — and most of those support abortion rights.
“That’s a lot of voters, if they show up and vote,” Blendon said.
Proposals to further protect — or restrict — abortion access could drive voter turnout. Advocates are working to put abortion-related measures on the ballot in such states as Arizona, Florida, Missouri, and South Dakota this November. A push in Washington toward a nationwide abortion policy could also draw more voters to the polls, Blendon said.
A surprise ruling by the Alabama Supreme Court in February that frozen embryos are children could also shake up the election. It’s an issue that divides even the anti-abortion community, with some who believe that a fertilized egg is a unique new person deserving of full legal rights and protections, and others believing that discarding unused embryos as part of the in vitro fertilization process is a morally acceptable way for couples to have children.
Pricey Prescriptions
Drug costs regularly rank high among voters’ concerns.
In the latest tracking poll, more than half — 55% — said they were very worried about being able to afford prescription drugs.
Biden has tried to address the price of drugs, though his efforts haven’t registered with many voters. While its name doesn’t suggest landmark health policy, the Inflation Reduction Act, or IRA, which the president signed in August 2022, included a provision allowing Medicare to negotiate prices for some of the most expensive drugs. It also capped total out-of-pocket spending for prescription drugs for all Medicare patients, while capping the price of insulin for those with diabetes at $35 a month — a limit some drugmakers have extended to patients with other kinds of insurance.
Drugmakers are fighting the Medicare price negotiation provision in court. Republicans have promised to repeal the IRA, arguing that forcing drugmakers to negotiate lower prices on drugs for Medicare beneficiaries would amount to price controls and stifle innovation. The party has offered no specific alternative, with the GOP-led House focused primarily on targeting pharmacy benefit managers, the arbitrators who control most Americans’ insurance coverage for medicines.
Costs of Coverage
Health care costs continue to rise for many Americans. The cost of employer-sponsored health plans have hit new highs in the past few months, raising costs for employers and workers alike. Experts have attributed the increase to high demand and expensive prices for certain drugs and treatments, notably weight loss drugs, as well as to medical inflation.
Meanwhile, the ACA is popular. The KFF poll found that more adults want to see the program expanded than scaled back. And a record 21.3 million people signed up for coverage in 2024, about 5 million of them new customers.
Enrollment in Republican-dominated states has grown fastest, with year-over-year increases of 80% in West Virginia, nearly 76% in Louisiana, and 62% in Ohio, according to the Centers for Medicare & Medicaid Services.
Public support for Obamacare and record enrollment in its coverage have made it politically perilous for Republicans to pursue the law’s repeal, especially without a robust alternative. That hasn’t stopped Trump from raising that prospect on the campaign trail, though it’s hard to find any other Republican candidate willing to step out on the same limb.
“The more he talks about it, the more other candidates have to start answering for it,” said Jarrett Lewis, a partner at Public Opinion Strategies, a GOP polling firm.
“Will a conversation about repeal-and-replace resonate with suburban women in Maricopa County?” he said, referring to the populous county in Arizona known for being a political bellwether. “I would steer clear of that if I was a candidate.”
Biden and his campaign have pounced on Trump’s talk of repeal. The president has said he wants to make permanent the enhanced premium subsidies he signed into law during the pandemic that are credited with helping to increase enrollment.
Republican advisers generally recommend that their candidates promote “a market-based system that has the consumer much more engaged,” said Lewis, citing short-term insurance plans as an example. “In the minds of Republicans, there is a pool of people that this would benefit. It may not be beneficial for everyone, but attractive to some.”
Biden and his allies have criticized short-term insurance plans — which Trump made more widely available — as “junk insurance” that doesn’t cover care for serious conditions or illnesses.
Entitlements Are Off-Limits
Both Medicaid and Medicare, the government health insurance programs that cover tens of millions of low-income, disabled, and older people, remain broadly popular with voters, said the Democratic pollster Celinda Lake. That makes it unlikely either party would pursue a platform that includes outright cuts to entitlements. But accusing an opponent of wanting to slash Medicare is a common, and often effective, campaign move.
Although Trump has said he wouldn’t cut Medicare spending, Democrats will likely seek to associate him with other Republicans who support constraining the program’s costs. Polls show that most voters oppose reducing any Medicare benefits, including by raising Medicare’s eligibility age from 65. However, raising taxes on people making more than $400,000 a year to shore up Medicare’s finances is one idea that won strong backing in a recent poll by The Associated Press and NORC Center for Public Affairs Research.
Brian Blase, a former Trump health adviser and the president of Paragon Health Institute, said Republicans, if they win more control of the federal government, should seek to lower spending on Medicare Advantage — through which commercial insurers provide benefits — to build on the program’s efficiencies and ensure it costs taxpayers less than the traditional program.
So far, though, Republicans, including Trump, have expressed little interest in such a plan. Some of them are clear-eyed about the perils of running on changing Medicare, which cost $829 billion in 2021 and is projected to consume nearly 18% of the federal budget by 2032.
“It’s difficult to have a frank conversation with voters about the future of the Medicare program,” said Lewis, the GOP pollster. “More often than not, it backfires. That conversation will have to happen right after a major election.”
Addiction Crisis
Many Americans have been touched by the growing opioid epidemic, which killed more than 112,000 people in the United States in 2023 — more than gun deaths and road fatalities combined. Rural residents and white adults are among the hardest hit.
Federal health officials have cited drug overdose deaths as a primary cause of the recent drop in U.S. life expectancy.
Republicans cast addiction as largely a criminal matter, associating it closely with the migration crisis at the U.S. southern border that they blame on Biden. Democrats have sought more funding for treatment and prevention of substance use disorders.
“This affects the family, the neighborhood,” said Blendon, the public opinion researcher.
Billions of dollars have begun to flow to states and local governments from legal settlements with opioid manufacturers and retailers, raising questions about how to best spend that money. But it isn’t clear that the crisis, outside the context of immigration, will emerge as a campaign issue.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
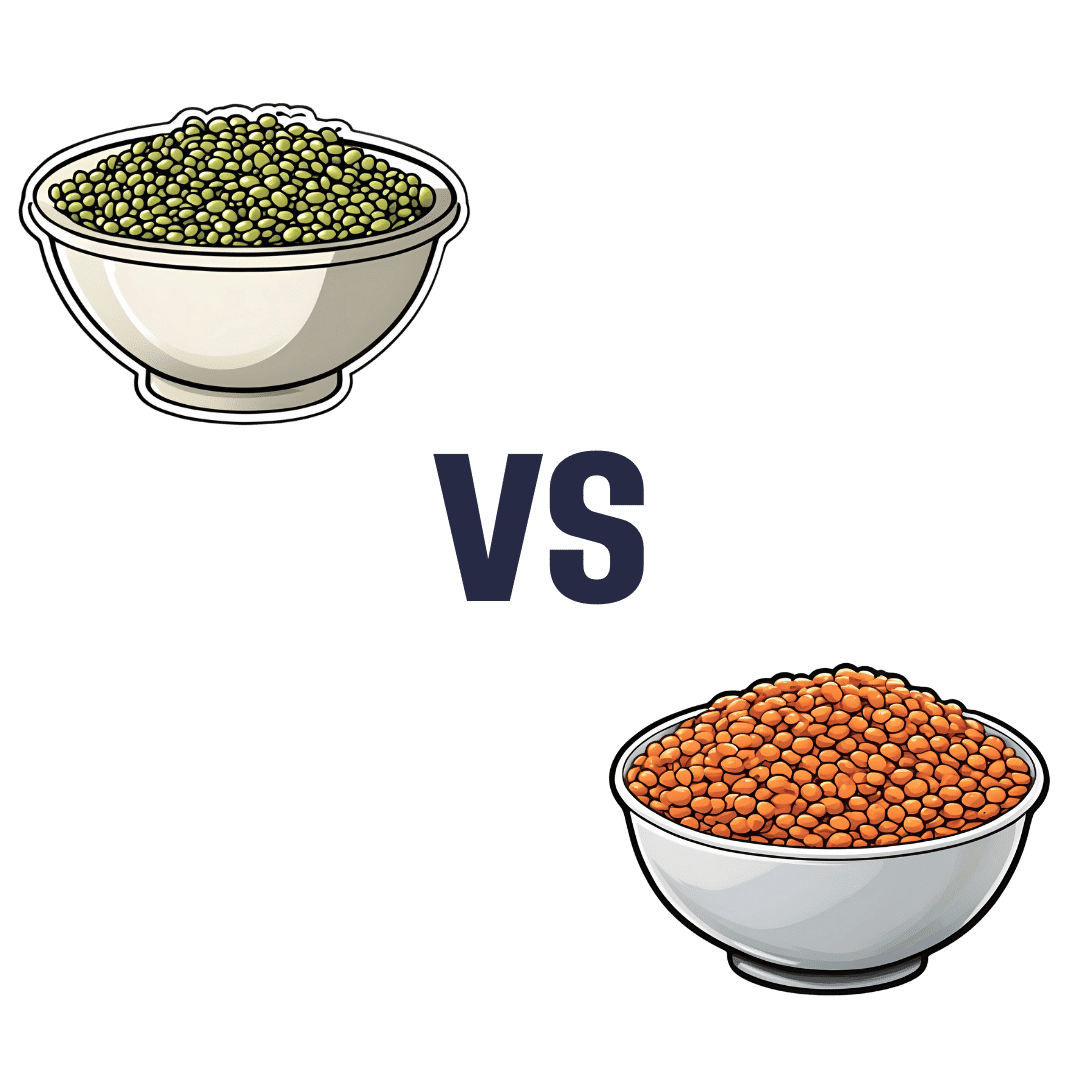
Mung Beans vs Red Lentils – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to red lentils, we picked the lentils.
Why?
Both are great! But the lentils win on overall nutritional density.
In terms of macros, they have approximately the same carbs and fiber, and are both low glycemic index foods. The deciding factor is that the lentils have slightly more protein—but it’s not a huge difference; both are very good sources of protein.
In the category of vitamins, mung beans have more of vitamins A, E, and K, while red lentils have more of vitamins B1, B2, B3, B5, B6, B9, C, and choline. An easy win for lentils.
When it comes to minerals, again both are great, but mung beans have more calcium and magnesium (hence the green color) while red lentils have more copper, iron, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for lentils.
Polyphenols are also a worthy category to note here; both have plenty, but red lentils have more, especially flavonols, anthocyanidins, proanthocyanidins, and anthocyanins (whence the red color).
In short: enjoy both, because diversity is almost always best. But if you’re picking one, red lentils are the most nutritious of the two.
Want to learn more?
You might like to read:
Sprout Your Seeds, Grains, Beans, Etc
Take care!
Share This Post
-
Do We Need Sunscreen In Winter, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I keep seeing advice that we shoudl wear sunscreen out in winter even if it’s not hot or sunny, but is there actually any real benefit to this?❞
Short answer: yes (but it’s indeed not as critical as it is during summer’s hot/sunny days)
Longer answer: first, let’s examine the physics of summer vs winter when it comes to the sun…
In summer (assuming we live far enough from the equator to have this kind of seasonal variation), the part of the planet where we live is tilted more towards the sun. This makes it closer, and more importantly, it’s more directly overhead during the day. The difference in distance through space isn’t as big a deal as the difference in distance through the atmosphere. When the sun is more directly overhead, its rays have a shorter path through our atmosphere, and thus less chance of being blocked by cloud cover / refracted elsewhere / bounced back off into space before it even gets that far.
In winter, the opposite of all that is true.
Morning/evening also somewhat replicate this compared to midday, because the sun being lower in the sky has a similar effect to seasonal variation causing it to be less directly overhead.
For this reason, even though visually the sun may be just as bright on a winter morning as it is on a summer midday, the rays have been filtered very differently by the time they get to us.
This is one reason why you’re much less likely to get sunburned in the winter, compared to the summer (others include the actual temperature difference, your likely better hydration, and your likely more modest attire protecting you).
However…
The reason it is advisable to wear sunscreen in winter is not generally about sunburn, and is rather more about long-term cumulative skin damage (ranging from accelerated aging to cancer) caused by the UV rays—specifically, mostly UVA rays, since UVB rays (with their higher energy but shorter wavelength) have nearly all been blocked by the atmosphere.
Here’s a good explainer of that from the American Cancer Society:
UV (Ultraviolet) Radiation and Cancer Risk
👆 this may seem like a no-brainer, but there’s a lot explained here that demystifies a lot of things, covering ionizing vs non-ionizing radiation, x-rays and gamma-rays, the very different kinds of cancer caused by different things, and what things are dangerous vs which there’s no need to worry about (so far as best current science can say, at least).
Consequently: yes, if you value your skin health and avoidance of cancer, wearing sunscreen when out even in the winter is a good idea. Especially if your phone’s weather app says the UV index is “moderate” or above, but even if it’s “low”, it doesn’t hurt to include it as part of your skincare routine.
But what if sunscreens are dangerous?
Firstly, not all sunscreens are created equal:
Learn more: Who Screens The Sunscreens?
Secondly: consider putting on a protective layer of moisturizer first, and then the sunscreen on top. Bear in mind, this is winter we’re talking about, so you’re probably not going out in a bikini, so this is likely a face-neck-hands job and you’re done.
What about vitamin D?
Humans evolved to have more or less melanin in our skin depending on where we lived, and white people evolved to wring the most vitamin D possible out of the meagre sun far from the equator. Black people’s greater melanin, on the other hand, offers some initial protection against the sun (but any resultant skin cancer is then more dangerous than it would be for white people if it does occur, so please do use sunscreen whatever your skintone).
Nowadays many people live in many places which may or may not be the places we evolved for, and so we have to take that into account when it comes to sun exposure.
Here’s a deeper dive into that, for those who want to learn:
Take care!
Share This Post
Related Posts
-
Salmon vs Tuna – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing salmon to tuna, we picked the tuna.
Why?
It’s close, and there are merits and drawbacks to both!
In terms of macros, tuna is higher in protein, while salmon is higher in fats. How healthy are the fats, you ask? Well, it’s a mix, because while there are plenty of “good” fats in salmon, salmon is also 10x higher in saturated fat and 150% higher in cholesterol.
So when it comes to fats, if you want to eat fish and have the healthiest fats, one option is to skip the salmon, and instead serve tuna with some extra virgin olive oil.
We’ll call this section a clear win for tuna.
On the vitamin front, they are close to equal. Salmon has more of some vitamins, tuna has more of others; all in all we’d say the balance is in salmon’s favor, but by the time a portion of salmon is giving you 350% of your daily requirement, does it really matter that the same portion of tuna is “only” giving you 294% of the daily requirement? It goes like that for a lot of the vitamins they both contain.
Still, we’ll call this section a nominal win for salmon.
In the category of minerals, tuna is much higher in iron while salmon is higher in calcium. The rest of the minerals they both have, tuna is comfortably higher—and since the “% of RDA in a portion” figures are double-digit here rather than triple, those margins are relevant this time.
We’ll call this section a moderate win for tuna.
Both fish carry a risk of mercury poisoning, but this varies more by location than by fish, so it hasn’t been a consideration in this head-to-head.
Totting up the sections, this a modest but clear win for tuna.
Want to learn more?
You might like to read:
Farmed Fish vs Wild-Caught: Important Differences!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Raspberries vs Blackberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing raspberries to blackberries, we picked the blackberries.
Why?
It was very close! Raspberries most certainly also have their merits. But blackberries do just a little bit better in a few categories:
In terms of macros, raspberries have a tiny bit more carbs and fiber, while blackberries have a even tinier bit more protein, and the two berries have an equal glycemic index. We’ll call this category a tie, or else the meanest of nominal wins for raspberry.
In the category of vitamins, raspberries have more of vitamins B1, B2, B5, B6, and choline, while blackberries have more of vitamins A, B3, B9, C, E, and K. This would be a very marginal win for blackberries, except that blackberries have more than 6x the vitamin A, a much larger margin than any of the other differences in vitamins (which were usually small differences), which gives blackberry a more convincing win here.
When it comes to minerals, things are closer: raspberries have more iron, magnesium, manganese, and phosphorus, while blackberries have more calcium, copper, potassium, selenium, and zinc. None of the differences are outstanding, so this is a simple marginal victory for blackberries.
It would be rude to look at berries without noting their polyphenols; we’re not list them all (or this article will get very long, because each has very many polyphenols with names like “pelargonidin 3-O-glucosyl-rutinoside” and so forth), but suffice it to say: raspberries are great for polyphenols and blackberries are even better for polyphenols.
That said… In the category of specific polyphenols we’ve written about before at 10almonds, it’s worth noting a high point of each berry, for the sake of fairness: raspberries have more quercetin (but blackberries have lots too) and blackberries have more ellagic acid (of which, raspberries have some, but not nearly as much). Anyway, just going off total polyphenol content, blackberries are the clear winner here.
Adding up the sections makes for an overall win for blackberries, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Wholewheat Bread vs Seeded White – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing wholewheat bread to seeded bread, we picked the wholewheat.
Why?
First, we will acknowledge that this is a false dichotomy; it is possible to have seeded wholewheat bread. However, it is very common to have wholewheat bread that isn’t seeded, and white bread that is seeded. So, it’s important to be able to decide which is the healthier option, since very often, this false dichotomy is what’s on offer.
We will also advise checking labels (or the baker, if getting from a bakery) to ensure that visibly brown bread is actually wholewheat, and not just dyed brown with caramel coloring or such (yes, that is a thing that some companies do).
Now, as for why we chose the wholewheat over the seeded white…
In terms of macronutrients, wholewheat bread has (on average; individual breads may vary of course) has 2x the protein and a lot more fiber.
Those seeds in seeded bread? They just aren’t enough to make a big impact on the overall nutritional value of the bread in those regards. Per slice, you are getting, what, 10 seeds maybe? This is not a meaningful dietary source of much.
Seeded bread does have proportionally more healthy fats, but the doses are still so low as to make it not worth the while; it just looks like a lot of expressed as a percentage of comparison, because of the wholewheat bread has trace amounts, and the seeded bread has several times those trace amounts, it’s still a tiny amount. So, we’d recommend looking to other sources for those healthy fats.
Maybe dip your bread, of whatever kind, into extra virgin olive oil, for example.
Wholewheat bread of course also has a lower glycemic index. Those seeds in seeded white bread don’t really slow it down at all, because they’re not digested until later.
Want to learn more?
You might like to read:
- Carb-Strong or Carb-Wrong?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Gluten: What’s The Truth?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: