Heart Health vs Systemic Stress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At The Heart Of Good Health

This is Dr. Michelle Albert. She’s a cardiologist with a decades-long impressive career, recently including a term as the president of the American Heart Association. She’s the current Admissions Dean at UCSF Medical School. She’s accumulated enough awards and honors that if we list them, this email will not fit in your inbox without getting clipped.
What does she want us to know?
First, lifestyle
Although Dr. Albert is also known for her work with statins (which found that pravastatin may have anti-inflammatory effects in addition to lipid-lowering effects, which is especially good news for women, for whom the lipid-lowering effects may be less useful than for men), she is keen to emphasize that they should not be anyone’s first port-of-call unless “first” here means “didn’t see the risk until it was too late and now LDL levels are already ≥190 mg/dL”.
Instead, she recommends taking seriously the guidelines on:
- getting plenty of fruit, vegetables, whole grains, lean protein
- avoiding red meat, processed meats, refined carbohydrates, and sweetened beverages
- getting your 150 minutes per week of moderate exercise
- avoiding alcohol, and definitely abstaining from smoking
See also: These Top Five Things Make The Biggest Difference To Health
Next, get your house in order
No, not your home gym—though sure, that too!
But rather: after the “Top Five Things” we linked just above, the sixth on the list would be “reduce stress”. Indeed, as Dr. Albert says:
❝Heart health is not just about the physical heart but also about emotional well-being. Stress management is crucial for a healthy heart❞
~ Dr. Michelle Albert
This is where a lot of people would advise mindfulness meditation, CBT, somatic therapies, and the like. And these things are useful! See for example:
No-Frills, Evidence-Based Mindfulness
…and:
However, Dr. Albert also advocates for awareness of what some professionals have called “Shit Life Syndrome”.
This is more about socioeconomic factors. There are many of those that can’t be controlled by the individual, for example:
❝Adverse maternal experiences such as depression, economic issues and low social status can lead to poor cognitive outcomes as well as cardiovascular disease.
Many jarring statistics illuminate a marked wealth gap by race and ethnicity… You might be thinking education could help bridge that gap. But it is not that simple.
While education does increase wealth, the returns are not the same for everyone. Black persons need a post-graduate degree just to attain similar wealth as white individuals with a high school degree.❞
~ Dr. Michelle Albert
Read in full: AHA president: The connection between economic adversity and cardiovascular health
What this means in practical terms (besides advocating for structural change to tackle the things such as the racism that has been baked into a lot of systems for generations) is:
Be aware not just of your obvious health risk factors, but also your socioeconomic risk factors, if you want to have good general health outcomes.
So for example, let’s say that you, dear reader, are wealthy and white, in which case you have some very big things in your favor, but are you also a woman? Because if so…
Women and Minorities Bear the Brunt of Medical Misdiagnosis
See also, relevant for some: Obesity Discrimination In Healthcare Settings ← you’ll need to scroll to the penultimate section for this one.
In other words… If you are one of the majority of people who is a woman and/or some kind of minority, things are already stacked against you, and not only will this have its own direct harmful effect, but also, it’s going to make your life harder and that stress increases CVD risk more than salt.
In short…
This means: tackle not just your stress, but also the things that cause that. Look after your finances, gather social support, know your rights and be prepared to self-advocate / have someone advocate for you, and go into medical appointments with calm well-prepared confidence.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The “Five Tibetan Rites” & Why To Do Them!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Spinning Around
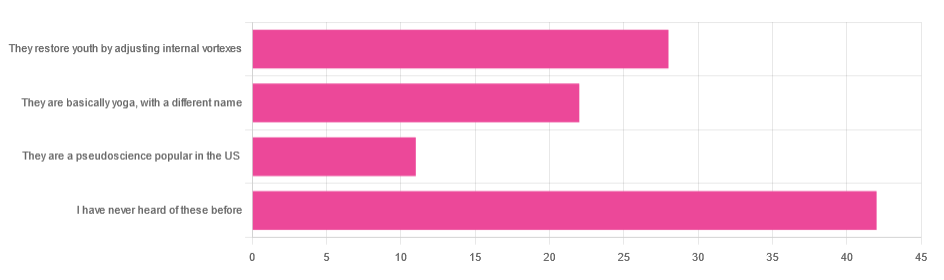
In Tuesday’s newsletter, we asked you for your opinion of the “Five Tibetan Rites”, and got the above-depicted, below-described, set of responses:
- About 41% said “I have never heard of these before”
- About 27% said “they restore youth by adjusting internal vortexes”
- About 22% said “they are basically yoga, by a different name”
- About 11% said “they are a pseudoscience popular in the US”
So what does the science say?
The Five Tibetan Rites are five Tibetan rites: True or False?
False, though this is more question of social science than of health science, so we’ll not count it against them for having a misleading name.
The first known mentioning of the “Five Tibetan Rites” is by an American named Peter Kelder, who in 1939 published, through a small LA occult-specialized publishing house, a booklet called “The Eye of Revelation”. This work was then varyingly republished, repackaged, and occasionally expanded upon by Kelder or other American authors, including Chris Kilham’s popular 1994 book “The Five Tibetans”.
The “Five Tibetan Rites” are unknown as such in Tibet, except for what awareness of them has been raised by people asking about them in the context of the American phenomenon.
Here’s a good history book, for those interested:
The author didn’t originally set out to “debunk” anything, and is himself a keen spiritualist (and practitioner of the five rites), but he was curious about the origins of the rites, and ultimately found them—as a collection of five rites, and the other assorted advices given by Kelder—to be an American synthesis in the whole, each part inspired by various different physical practices (some of them hatha yoga, some from the then-popular German gymnastics movement, some purely American spiritualism, all available in books that were popular in California in the early 1900s).
You may be wondering: why didn’t Kelder just say that, then, instead of telling stories of an ancient Tibetan tradition that empirically does not exist? The answer to this lies again in social science not health science, but it’s been argued that it’s common for Westerners to “pick ‘n’ mix” ideas from the East, champion them as inscrutably mystical, and (since they are inscrutable) then simply decide how to interpret and represent them. Here’s an excellent book on this, if you’re interested:
(in Kelder’s case, this meant that “there’s a Tibetan tradition, trust me” was thus more marketable in the West than “I read these books in LA”)
They are at least five rites: True or False?
True! If we use the broad definition of “rite” as “something done repeatedly in a solemn fashion”. And there are indeed five of them:
- Spinning around (good for balance)
- Leg raises (this one’s from German gymnastics)
- Kneeling back bend (various possible sources)
- Tabletop (hatha yoga, amongst others)
- Pendulum (hatha yoga, amongst others) ← you may recognize this one from the Sun Salutation
You can see them demonstrated here:
Click Here If The Embedded Video Doesn’t Load Automatically
Kelder also advocated for what was basically the Hay Diet (named not for the substance but for William Hay; it involved separating foods into acid and alkali, not necessarily according to the actual pH of the foods, and combining only “acid” foods or only “alkali” foods at a time), which was popular at the time, but has since been rejected as without scientific merit. Kelder referred to this as “the sixth rite”.
The Five Rites restore youth by adjusting internal vortexes: True or False?
False, in any scientific sense of that statement. Scientifically speaking, the body does not have vortexes to adjust, therefore that is not the mechanism of action.
Spiritually speaking, who knows? Not us, a humble health science publication.
The Five Rites are a pseudoscience popular in the US: True or False?
True, if 27% of those who responded of our mostly North American readership can be considered as representative of what is popular.
However…
“Pseudoscience” gets thrown around a lot as a bad word; it’s often used as a criticism, but it doesn’t have to be. Consider:
A small child who hears about “eating the rainbow” and mistakenly understands that we are all fuelled by internal rainbows that need powering-up by eating fruits and vegetables of different colors, and then does so…
…does not hold a remotely scientific view of how things are happening, but is nevertheless doing the correct thing as recommended by our best current science.
It’s thus a little similar with the five rites. Because…
The Five Rites are at least good for our health: True or False?
True! They are great for the health.
The first one (spinning around) is good for balance. Science would recommend doing it both ways rather than just one way, but one is not bad. It trains balance, trains our stabilizing muscles, and confuses our heart a bit (in a good way).
See also: Fall Special (How To Not Fall, And Not Get Injured If You Do)
The second one (leg raises) is excellent for core strength, which in turn helps keep our organs where they are supposed to be (this is a bigger health issue than most people realise, because “out of sight, out of mind”), which is beneficial for many aspects of our health!
See also: Visceral Belly Fat & How To Lose It ← visceral fat is the fat that surrounds your internal organs; too much there becomes a problem!
The third, fourth, and fifth ones stretch our spine (healthily), strengthen our back, and in the cases of the fourth and fifth ones, are good full-body exercises for building strength, and maintaining muscle mass and mobility.
See also: Building & Maintaining Mobility
So in short…
If you’ve been enjoying the Five Rites, by all means keep on doing them; they might not be Tibetan (or an ancient practice, as presented), and any mystical aspect is beyond the scope of our health science publication, but they are great for the health in science-based ways!
Take care!
Share This Post
-
Thinking of using an activity tracker to achieve your exercise goals? Here’s where it can help – and where it probably won’t
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of year when many people are getting started on their resolutions for the year ahead. Doing more physical activity is a popular and worthwhile goal.
If you’re hoping to be more active in 2024, perhaps you’ve invested in an activity tracker, or you’re considering buying one.
But what are the benefits of activity trackers? And will a basic tracker do the trick, or do you need a fancy one with lots of features? Let’s take a look.
Why use an activity tracker?
One of the most powerful predictors for being active is whether or not you are monitoring how active you are.
Most people have a vague idea of how active they are, but this is inaccurate a lot of the time. Once people consciously start to keep track of how much activity they do, they often realise it’s less than what they thought, and this motivates them to be more active.
You can self-monitor without an activity tracker (just by writing down what you do), but this method is hard to keep up in the long run and it’s also a lot less accurate compared to devices that track your every move 24/7.
By tracking steps or “activity minutes” you can ascertain whether or not you are meeting the physical activity guidelines (150 minutes of moderate to vigorous physical activity per week).
It also allows you to track how you’re progressing with any personal activity goals, and view your progress over time. All this would be difficult without an activity tracker.
Research has shown the most popular brands of activity trackers are generally reliable when it comes to tracking basic measures such as steps and activity minutes.
But wait, there’s more
Many activity trackers on the market nowadays track a range of other measures which their manufacturers promote as important in monitoring health and fitness. But is this really the case? Let’s look at some of these.
Resting heart rate
This is your heart rate at rest, which is normally somewhere between 60 and 100 beats per minute. Your resting heart rate will gradually go down as you become fitter, especially if you’re doing a lot of high-intensity exercise. Your risk of dying of any cause (all-cause mortality) is much lower when you have a low resting heart rate.
So, it is useful to keep an eye on your resting heart rate. Activity trackers are pretty good at tracking it, but you can also easily measure your heart rate by monitoring your pulse and using a stopwatch.
Heart rate during exercise
Activity trackers will also measure your heart rate when you’re active. To improve fitness efficiently, professional athletes focus on having their heart rate in certain “zones” when they’re exercising – so knowing their heart rate during exercise is important.
But if you just want to be more active and healthier, without a specific training goal in mind, you can exercise at a level that feels good to you and not worry about your heart rate during activity. The most important thing is that you’re being active.
Also, a dedicated heart rate monitor with a strap around your chest will do a much better job at measuring your actual heart rate compared to an activity tracker worn around your wrist.
Maximal heart rate
This is the hardest your heart could beat when you’re active, not something you could sustain very long. Your maximal heart rate is not influenced by how much exercise you do, or your fitness level.
Most activity trackers don’t measure it accurately anyway, so you might as well forget about this one.
VO₂max
Your muscles need oxygen to work. The more oxygen your body can process, the harder you can work, and therefore the fitter you are.
VO₂max is the volume (V) of oxygen (O₂) we could breathe maximally (max) over a one minute interval, expressed as millilitres of oxygen per kilogram of body weight per minute (ml/kg/min). Inactive women and men would have a VO₂max lower than 30 and 40 ml/kg/min, respectively. A reasonably good VO₂max would be mid thirties and higher for women and mid forties and higher for men.
VO₂max is another measure of fitness that correlates well with all-cause mortality: the higher it is, the lower your risk of dying.
For athletes, VO₂max is usually measured in a lab on a treadmill while wearing a mask that measures oxygen consumption. Activity trackers instead look at your running speed (using a GPS chip) and your heart rate and compare these measures to values from other people.
If you can run fast with a low heart rate your tracker will assume you are relatively fit, resulting in a higher VO₂max. These estimates are not very accurate as they are based on lots of assumptions. However, the error of the measurement is reasonably consistent. This means if your VO₂max is gradually increasing, you are likely to be getting fitter.
So what’s the take-home message? Focus on how many steps you take every day or the number of activity minutes you achieve. Even a basic activity tracker will measure these factors relatively accurately. There is no real need to track other measures and pay more for an activity tracker that records them, unless you are getting really serious about exercise.
Corneel Vandelanotte, Professorial Research Fellow: Physical Activity and Health, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Collagen Cure – by Dr. James DiNicolantonio
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Collagen is vital for, well, most of our bodies, really. Where me most tend to feel its deficiency is in our joints and skin, but it’s critical for bones and many other tissues too.
You may be wondering: why a 572-page book to say what surely must amount to “take collagen, duh”?
Dr. DiNicolantonio has a lot more of value to offer us than that. In this book, we learn about not just collagen synthesis and usage, different types of collagen, the metabolism of it in our diet (if we get it—vegans and vegetarians won’t). We also learn about the building blocks of collagen (vegans and vegetarians do get these, assuming a healthy balanced diet), with a special focus on glycine, the smallest amino acid which makes up about a third of the mass of collagen (a protein).
Not stopping there, we also learn about the interplay of other nutrients with our metabolism of glycine and, if applicable, collagen. Vitamin C and copper are star features, but there’s a lot more going on with other nutrients too, down to the level of “So take this 75 minutes before this but after that and/but definitely not with the other”, etc.
The style is incredibly clear and readable for something that’s also quite scientifically dense (over 1000 references and many diagrams).
Bottom line: if you’re serious about maintaining your body as you get older, and you’d like a book about collagen that’s a lot more helpful than “take collagen, duh”, then this is the book for you.
Click here to check out The Collagen Cure, and take care of yours!
Share This Post
Related Posts
-
Your Vitamins are Obsolete: The Vitamer Revolution – by Dr. Sheldon Zablow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not:a book to tell you “throw out your vitamins and just eat these foods”.
This book focuses mainly on two vitamins in which deficiencies are common especially as we get older: B9 and B12.
So, what does the title mean? It’s not so much that your vitamins are obsolete—that would imply that they were more useful previously, which is not the case. Rather, the most common forms of vitamins B9 and B12 provided in supplements are folic acid and cyanocobalamin, respectively, which as he demonstrates with extensive research to back up his claims, cannot be easily absorbed or used especially well.
About those vitamers: a vitamer is simply a form of a vitamin—most vitamins we need can arrive in a variety of forms. In the case of vitamins B9 and B12, he advocates for ditching vitamers folic acid and cyanocobalamin, cheap as they are, and springing for bioactive vitamers L-methylfolate, methylcobalamin, and adenosylcobalamin.
He also discusses (again, just as well-evidenced as the above things) why we might struggle to get enough from our diet after a certain age. For example, if trying to get these vitamins from meat, 50% of people over 50 cannot manufacture enough stomach acid to break down that protein to release the vitamins.
And as for methyl-B12 vitamers, you might expect you can get those from meat, and technically you can, but they don’t occur in all animals, just in one kind of animal. Specifically, the kind that has the largest brain-to-body ratio. However, eating the meat of this animal can result in protein folding errors in general and Creutzfeldt–Jakob disease in particular, so the author does not recommend eating humans, however nutritionally convenient that would be.
All this means that supplementation after a certain age really can be a sensible way to do it—but do it wisely, and pick the right vitamers.
The style of the book is informationally dense, but very readable even for a layperson provided one starts at the beginning and reads forwards, as otherwise one will find oneself in a mire of terms whose explanations one missed when they were first introduced.
Bottom line: if you are over 50 and/or have any known or suspected issues with vitamins B9 and/or B12, this book becomes very important reading.
Click here to check out Your Vitamins Are Obsolete, and get your body what it needs!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Painkilling Power Of Opioids, Without The Harm?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to painkilling medications, they can generally be categorized into two kinds:
- non-opioids (e.g. ibuprofen, paracetamol/acetaminophen, aspirin)
- ones that actually work for something more serious than a headache
That’s an oversimplification, but broadly speaking, when there is serious painkilling to be done, that’s when doctors consider it’s time to break out the opioids.
Nor are all opioids created equal—there’s a noteworthy difference between codeine and morphine, for instance—but the problems of opioids are typically the same (tolerance, addiction, and eventual likelihood of overdose when one tries to take enough to make it work after developing a tolerance), and it becomes simply a matter of degree.
See also: I’ve been given opioids after surgery to take at home. What do I need to know?
So, what’s the new development?
A team of researchers have found that the body can effectively produce its own targetted painkilling peptides, similar in function to benzodiazepines (an opioid drug), but—and which is a big difference—confined to the peripheral nervous system (PNS), meaning that it doesn’t enter the brain.
- The peptides killing the pain before it can reach the brain is obviously good because that means the pain is simply not experienced
- The peptides not having any effect on the brain, however, means that the mechanism of addiction of opioids simply does not apply here
- The peptides not having any effect on the brain also means that the CNS can’t be “put to sleep” by these peptides in the same way it can if a high dose of opioids is taken (this is what typically causes death in opioid overdoses; the heart simply beats too slowly to maintain life)
The hope, therefore, is to now create medications that target the spinal ganglia that produce these peptides, to “switch them on” at will.
Obviously, this won’t happen overnight; there will need to be first a lot of research to find a drug that does that (likely this will involve a lot of trial and error and so many mice/rats), and then multiple rounds of testing to ascertain that the drug is safe and effective for humans, before it can then be rolled out commercially.
But, this is still a big breakthrough; there arguably hasn’t been a breakthrough this big in pain research since various opioid-related breakthroughs in the 70s and 80s.
You can see a pop-science article about it here:
And you can see the previous research (from earlier this year) that this is now building from, about the glial cells in the spinal ganglia, here:
Peripheral gating of mechanosensation by glial diazepam binding inhibitor
But wait, there’s more!
Remember what we said about affecting the PNS without affecting the CNS, to kill the pain without killing the brain?
More researchers are already approaching the same idea to deal with the same problem, but from the angle of gene therapy, and have already had some very promising results with mice:
Structure-guided design of a peripherally restricted chemogenetic system
…which you can read about in pop-science terms (with diagrams!) here:
New gene therapy could alleviate chronic pain, researchers find
While you’re waiting…
In the meantime, approaches that are already available include:
- The 7 Approaches To Pain Management
- Managing Chronic Pain (Realistically!)
- Science-Based Alternative Pain Relief ← when painkillers aren’t helping, these things might!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cranberry juice really can help with UTIs – and reduce reliance on antibiotics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cranberry juice has been used medicinally for centuries. Our new research indicates it should be a normal aspect of urinary tract infection (UTI) management today.
While some benefits of cranberry compounds for the prevention of UTIs have been suspected for some time, it hasn’t been clear whether the benefits from cranberry juice were simply from drinking more fluid, or something in the fruit itself.
For our study, published this week, we combined and collectively assessed 3,091 participants across more than 20 clinical trials.
Our analysis indicates that increasing liquids reduces the rate of UTIs compared with no treatment, but cranberry in liquid form is even better at reducing UTIs and antibiotic use.
Julie Falk/Flickr, CC BY-NC-ND Are UTIs really that bad?
Urinary tract infections affect more than 50% of women and 20% of men in their lifetime.
Most commonly, UTIs are caused from the bug called Escherichia coli (E.coli). This bug lives harmlessly in our intestines, but can cause infection in the urinary tract. This is why, particularly for women, it is recommended people wipe from front to back after using the toilet.
An untreated UTI can move up to the kidneys and cause even more serious illness.
Even when not managing infection, many people are anxious about contracting a UTI. Sexually active women, pregnant women and older women may all be at increased risk.
Why cranberries?
To cause a UTI, the bacteria need to attach to the wall of the urinary bladder. Increasing fluids helps to flush out bacteria before it attaches (or makes its way up into the bladder).
Some beneficial compounds in cranberry, such as proanthocyanidins (also called condensed tannins), prevent the bacteria from attaching to the wall itself.
While there are treatments, over 90% of the bugs that cause UTIs exhibit some form of microbial resistance. This suggests that they are rapidly changing and some cases of UTI might be left untreatable.
The juice of cranberries has long been thought to have infection-fighting properties. duckeesue/Shutterstock What we found
Our analysis showed a 54% lower rate of UTIs from cranberry juice consumption compared to no treatment. This means that significantly fewer participants who regularly consumed cranberry juice (most commonly around 200 millilitres each day) reported having a UTI during the periods assessed in the studies we analysed.
Cranberry juice was also linked to a 49% lower rate of antibiotic use than placebo liquid and a 59% lower rate than no treatment, based on analysis of indirect and direct effects across six studies. The use of cranberry compounds, whether in drinks or tablet form, also reduced the prevalence of symptoms associated with UTIs.
While some studies we included presented conflicts of interest (such as receiving funding from cranberry companies), we took this “high risk of bias” into account when analysing the data.
The study found extra hydration helped but not to the same extent as cranberry juice. Pixelshot/Shutterstock So, when can cranberry juice help?
We found three main benefits of cranberry juice for UTIs.
1. Reduced rates of infections
Increasing fluids (for example, drinking more water) reduced the prevalence of UTIs, and taking cranberry compounds (such as tablets) was also beneficial. But the most benefits were identified from increasing fluids and taking cranberry compounds at the same time, such as with cranberry juice.
2. Reduced use of antibiotics
The data shows cranberry juice lowers the need to use antibiotics by 59%. This was identified as fewer participants in randomised cranberry juice groups required antibiotics.
Increasing fluid intake also helped reduce antibiotic use (by 25%). But this was not as useful as increasing fluids at the same time as using cranberry compounds.
Cranberry compounds alone (such as tablets without associated increases in fluid intake) did not affect antibiotic use.
3. Reducing symptoms
Taking cranberry compounds (in any form, liquid or tablet) reduced the symptoms of UTIs, as measured in the overall data, by more than five times.
Take home advice
While cranberry juice cannot treat a UTI, it can certainly be part of UTI management.
If you suspect that you have a UTI, see your GP as soon as possible.
Christian Moro, Associate Professor of Science & Medicine, Bond University and Charlotte Phelps, Senior Teaching Fellow, Medical Program, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: