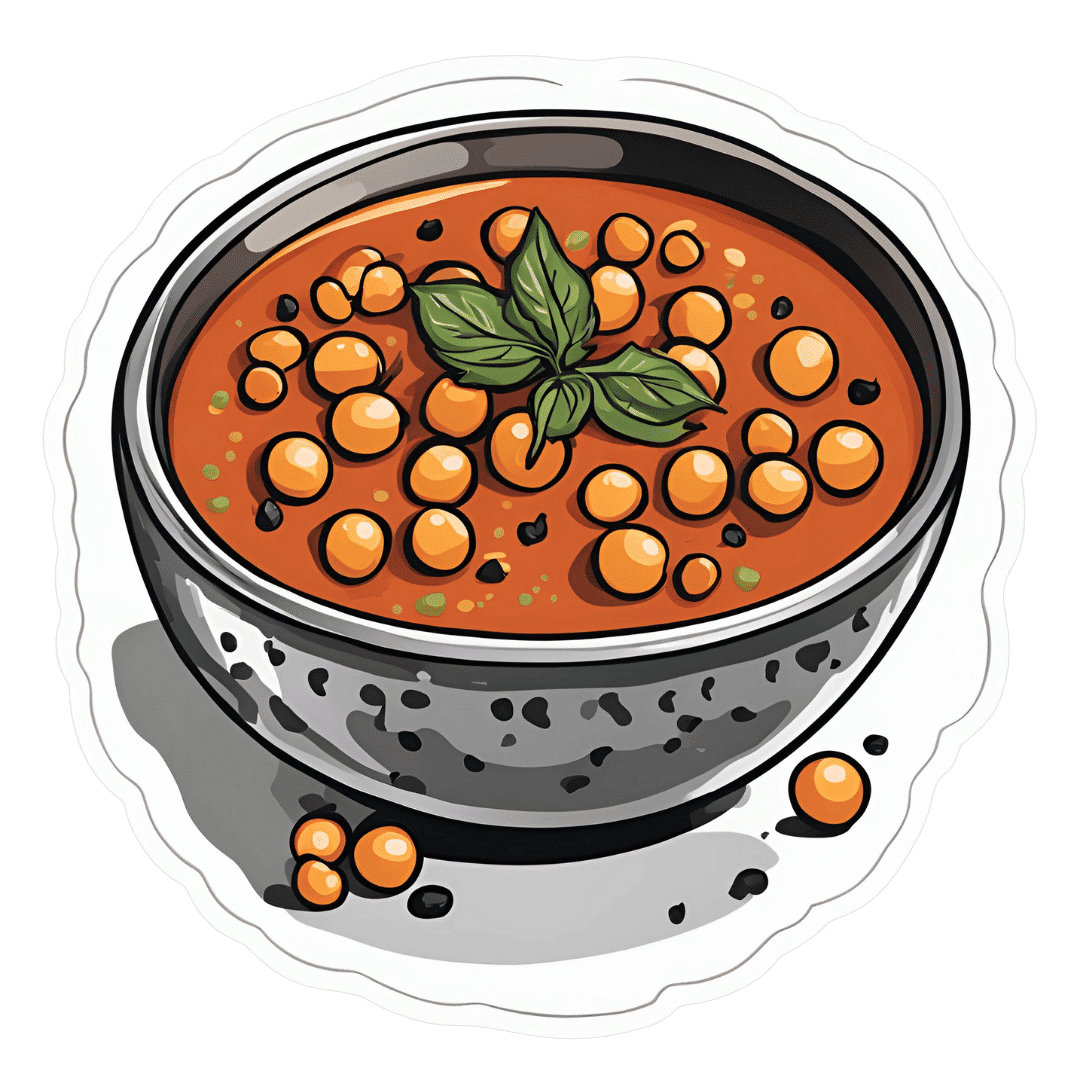
Gut-Healthy Sunset Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So-called for its gut-healthy ingredients, and its flavor profile being from the Maghreb (“Sunset”) region, the western half of the N. African coast.
You will need
- 1 can chickpeas (do not drain)
- 1 cup low-sodium vegetable stock
- 1 small onion, finely chopped
- 1 carrot, finely chopped
- 2 tbsp sauerkraut, drained and chopped (yes, it is already chopped, but we want it chopped smaller so it can disperse evenly in the soup)
- 2 tbsp tomato paste
- 1 tbsp harissa paste (adjust per your heat preference)
- 1 tbsp ras el-hanout
- ¼ bulb garlic, crushed
- Juice of ½ lemon
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
- Optional: herb garnish; we recommend cilantro or flat-leaf parsley
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a sauté pan or similar (something suitable for combination cooking, as we’ll be frying first and then adding liquids), and fry the onion and carrot until the onion is soft and translucent; about 5 minutes.
2) Stir in the garlic, tomato paste, harissa paste, and ras el-hanout, and fry for a further 1 minute.
3) Add the remaining ingredients* except the lemon juice. Bring to the boil and then simmer for 5 minutes.
*So yes, this includes adding the “chickpea water” also called “aquafaba”; it adds flavor and also gut-healthy fiber in the form of oligosaccharides and resistant starches, which your gut microbiota can use to make short-chain fatty acids, which improve immune function and benefit the health in more ways than we can reasonably mention as a by-the-way in a recipe.
4) Stir in the lemon juice, and serve, adding a herb garnish if you wish.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← today’s recipe scored 5/5 of these, plus quite a few more! Remember that ras el-hanout is a spice blend, so if you’re thinking “wait, where’s the…?” then it’s in the ras el-hanout 😉
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← not to be underestimated!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sarah Raven’s Garden Cookbook – by Sarah Raven
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Note: the US Amazon site currently (incorrectly) lists the author as “Jonathan Buckley”. The Canadian, British, and Australian sites all list the author correctly as Sarah Raven, and some (correctly) credit Jonathan Buckley as the photographer she used.
First, what it’s not: a gardening book. Beyond a few helpful tips, pointers, and “plant here, harvest here” instructions, this book assumes you are already capable of growing your own vegetables.
She does assume you are in a temperate climate, so if you are not, this might not be the book for you. Although! The recipes are still great; it’s just you’d have to shop for the ingredients and they probably won’t be fresh local produce for the exact same reason that you didn’t grow them.
If you are in a temperate climate though, this will take you through the year of seasonal produce (if you’re in a temperate climate but it’s in for example Australia, you’ll need to make a six-month adjustment for being in the S. Hemisphere), with many recipes to use not just one ingredient from your garden at a time, but a whole assortment, consistent with the season.
About the recipes: they (which are 450 in number) are (as you might imagine) very plant-forward, but they’re generally not vegan and often not vegetarian. So, don’t expect that you’ll produce everything yourself—just most of the ingredients!
Bottom line: if you like cooking, and are excited by the idea of growing your own food but are unsure how regularly you can integrate that, this book will keep you happily busy for a very long time.
Click here to check out Sarah Raven’s Garden Cookbook, and level-up your home cooking!
Share This Post
-
Bridging The Generation Gap Over The Holidays
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Often seen as a time for family connection, this same holiday period is often experienced as a time of family tension. But it doesn’t have to be that way!
Hopefully this will be of benefit to readers of all ages, but we’re going to write with the largest age-group of our readership, which is people who are most likely to have Gen-Z grandkids.
why are we writing about this?
Not only are health and happiness closely linked, and not only is mental health also just health, but… In terms of the healthy longevity secrets of the “Blue Zones”, strong intergenerational connections are usually a feature.
First, the obvious:
Any holiday tensions, of course, don’t usually start with grandkids, and are more likely amongst the adults, but some points of friction can be the same:
- Differences of opinion on political/social/economic issues
- Difference of opinion on parenting/dating choices
- Differences of opinion on life priorities
And yes, by the way, that includes even young teens (and perhaps younger) having opinions on these things—we are living in an information age, and this does mean a lot of information is a lot more accessible than it used to be, including for kids. Problems (at all ages) may occur when someone is only really exposed to views from within a certain “bias bubble”, but for better or worse, most people will have an opinion on most well-known things.
As a general rule of thumb, all of these differences of opinion can be shelved if (and only if) those involved seek to avoid conflict. And while age is no guarantee of maturity, often it’ll be the older person(s) in the strongest position to redirect things. So, have a stack of “safe” topics up your sleeve.
Bonus: you can also have non-conversational distractions up your sleeve! These may be kitchen-related, for example (time to produce something distracting, or if the nascent conflict was only between you and one other person, time to go check on something, thus removing yourself from the situation).
Next, about “family time” and technology
It can be tempting to try to have a “phones away” rule, but this will tend to only exacerbate a younger person’s withdrawal.
Better: ask (with a tone of cheerful curiosity, not accusation) about what captures their attention so. Ask about their favorite YouTubers or TikTokers or whatever it is that it is for them. Learn about that Subreddit.
Or maybe (more likely for Millennials) they were following what is going on in the world via social media, which takes on an intermediary role for the delivery of world news. Hopefully this won’t run into the differences of opinion that we mentioned up top, but it could also be a perfectly good avenue of conversation, and maybe there’s more common ground than you might expect.
Meanwhile, if you’re the older generation present, chances are your own social media use is more about the human element. That’s great, but watch out:
A common faux pas is taking pictures without asking, let alone posting them online without asking. For many people this may seem an odd thing to object to, but generationally speaking, the younger someone is (down to the upper single digits, anyway) the more likely they might feel strongly about this. So, ask first.
The reason, by the way, is that in this age of digital hypervisibility, what we choose to share online can be a deeply personal thing. And, say what you will about the pros or cons of someone carefully curating an image of how they wish to be seen, shortcutting through that for them with a candid photo posted on Facebook will not endear you to them, even if you can’t see anything wrong with the photo in question, for example.
See also: Make Social Media Work For Your Mental Health
Show an interest, but don’t interrogate
This one doesn’t take too much explanation. If people want to share about their lives, they’ll need only the smallest nudge to do so. If someone passes up an opportunity to talk about something you showed an interest in, chances are they have their own reasons for not wanting to talk about it. This might be hurtful if you feel like they’re keeping you out of their life, but the best way to get them to talk to you is just to be a good listener—not an interrogator that they have to dodge.
For some powerful tools on this, see: Listening, Better
Lastly, if things aren’t so good…
43% of people are currently experiencing some sort of familial estrangement, so if that’s you, you’re not on your own.
Sometimes, it really is too late to fix things, but sometimes it isn’t; we put together a guide that might help:
Family Estrangement & How To Fix It
Take care!
Share This Post
-
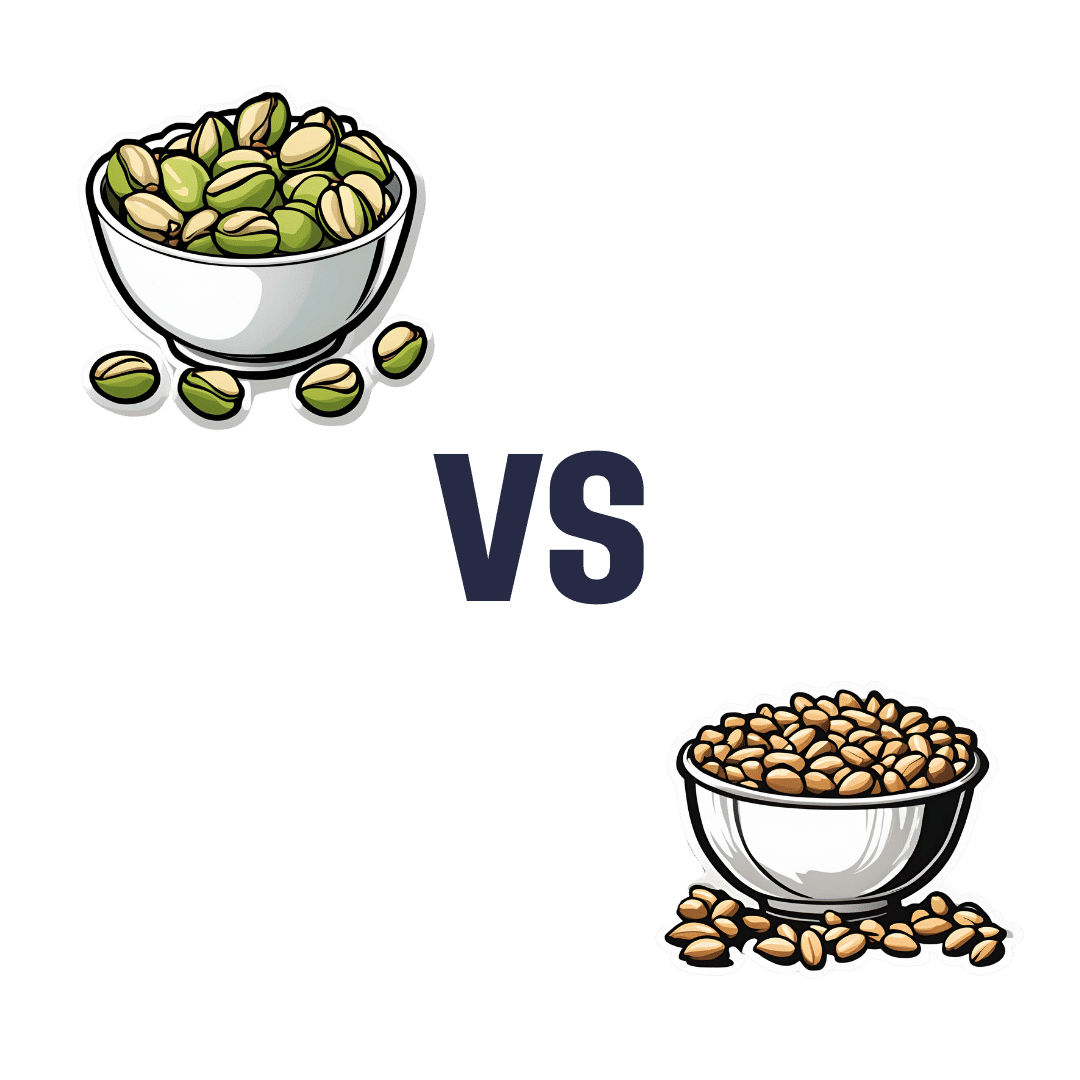
Pistachios vs Pine Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pine nuts, we picked the pistachios.
Why?
First looking at the macros, pistachios have nearly 2x the protein while pine nuts have nearly 2x the fat. The fats are healthy in moderation (mostly polyunsaturated, a fair portion of monounsaturated, and a little saturated), but we’re going to value the protein content higher. Also, pistachios have approximately 2x the carbs, and/but nearly 3x the fiber. All in all, we’ll call this section a moderate win for pistachios.
When it comes to vitamins, pistachios have more of vitamins A, B1, B5, B6, B9, and C, while pine nuts have more of vitamins B2, B3, E, K, and choline. All in all, pistachios are scraping a 6:5 win here, or we could call it a tie if we want to value pine nuts’ vitamins more (due to the difference in how many foods each vitamin is found in, and thus the likelihood of having a deficiency or not).
In the category of minerals, pistachios have more calcium, copper, potassium, and selenium, while pine nuts have more iron, magnesium, manganese, and zinc. This would be a tie if we just call it 4:4, but what’s worth noting is that while both of these nuts are a good source of most of the minerals mentioned, pine nuts aren’t a very good source of calcium or selenium, so we’re going to declare this section a very marginal win for pistachios.
Adding up the moderate win, the scraped win, and the barely scraped win, all adds up to a win for pistachios. However, as you might have noticed, both are great so do enjoy both if you can!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
Mung Beans vs Soy Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to soy beans, we picked the soy.
Why?
Mung beans are great, but honestly, it’s not close:
In terms of macronutrients, soy has more than 2x the protein (of which, it’s also a complete protein, containing significant amounts of all essential amino acids) while mung beans have more than 2x the carbs. In their defense, mung beans also have very slightly more fiber, but the carb:fiber ratio is such that soy beans have the lower GI by far.
When it comes to vitamins, mung beans have more of vitamins A, B3, B5, and, B9, while soy beans have more of vitamins B2, B6, C, E, K, and choline, making for a moderate win for soy beans, especially as that vitamin K is more than 7x as much as mung beans have.
In the category of minerals, soy wins even more convincingly; soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. On the other hand, mung beans have more sodium.
In short, while mung beans are a very respectable option, they don’t come close to meaningfully competing with soy.
Want to learn more?
You might like to read:
How To Sprout Your Seeds, Grains, Beans, Etc
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Health Fix – by Dr. Ayan Panja
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into three main sections:
- The foundations
- The aspirations
- The fixes
The foundations are an overview of the things you’re going to need to know, about biology, behaviors, and being human.
The aspirations are research-generated common hopes, desires, dreams and goals of patients who have come to Dr. Panja for help.
The fixes are exactly what you’d hope them to be. They’re strategies, tools, hacks, tips, tricks, to get you from where you are now to where you want to be, health-wise.
The book is well-structured, with deep-dives, summaries, and practical advice of how to make sure everything you’re doing works together as part of the big picture that you’re building for your health.
All in all, a fantastic catch-all book, whatever your health goals.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dentists Debunk 15 Teeth Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dentists Dr. John Yoo and Dr. Jason Lin leave no gaps in the truth:
The tooth, the whole tooth, and nothing but the tooth
Not only is there no tooth fairy (we are shocked), but also…
- “Baby teeth aren’t important.”
False! Baby teeth act as space holders for permanent teeth, affect speech development, and influence a child’s psychological well-being. - “Acidic fruits will whiten your smile.”
False! In any practical sense, anyway: acidic fruits may temporarily make teeth appear whiter by dispersing stains but cause enamel erosion and weaken teeth over time. - “Fillings last forever.”
False! Fillings can wear down, fail, or develop cavities underneath if oral hygiene isn’t maintained, requiring replacement over time. - “Cavities are irreversible.”
False! Cavities in the enamel can be reversed with fluoride and good oral hygiene, but cavities that reach the dentin are typically irreversible. - “Braces are just for crooked teeth.”
False! Braces also correct functional issues like overbites, underbites, crossbites, and prevent future complications like tooth impaction. - “A knocked-out tooth is gone for good.”
False! A knocked-out tooth can be reimplanted if done quickly (ideally within an hour); storing it in whole milk or saliva helps preserve it. - “Diet sodas won’t give you cavities.”
False! Diet sodas can still cause cavities due to their acidic pH, which erodes enamel, even without sugar. - “Dental cleanings aren’t necessary.”
False! Dental cleanings help remove plaque and tartar that regular brushing can’t, and allow for regular oral health checkups. - “Retainers aren’t for life.”
False! To maintain teeth alignment after braces, retainers should be worn long-term as teeth can shift even years later. - “You should floss before brushing.”
False! The order doesn’t matter, but do floss regularly. - “Everyone has wisdom teeth.”
False! Not everyone is born with wisdom teeth; they are the most commonly missing teeth, and not everyone needs them removed. - “Hydrogen peroxide and baking soda are good toothpaste replacements.”
False! While they are common components in toothpaste, they lack fluoride, which is essential for remineralizing and protecting enamel. - “You’re too old to get braces.”
False! There’s no age limit for braces or aligners; adults often seek them for both aesthetic and functional reasons. - “Teeth that have had root canals can’t feel.”
False! Teeth with root canals can’t feel pain from nerves, but you can still sense pressure due to surrounding ligaments. - “You’ll inevitably lose all your teeth when you’re old.”
False! Good oral hygiene and regular dental care can preserve natural teeth into old age, though genetics also play a role.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- “Baby teeth aren’t important.”