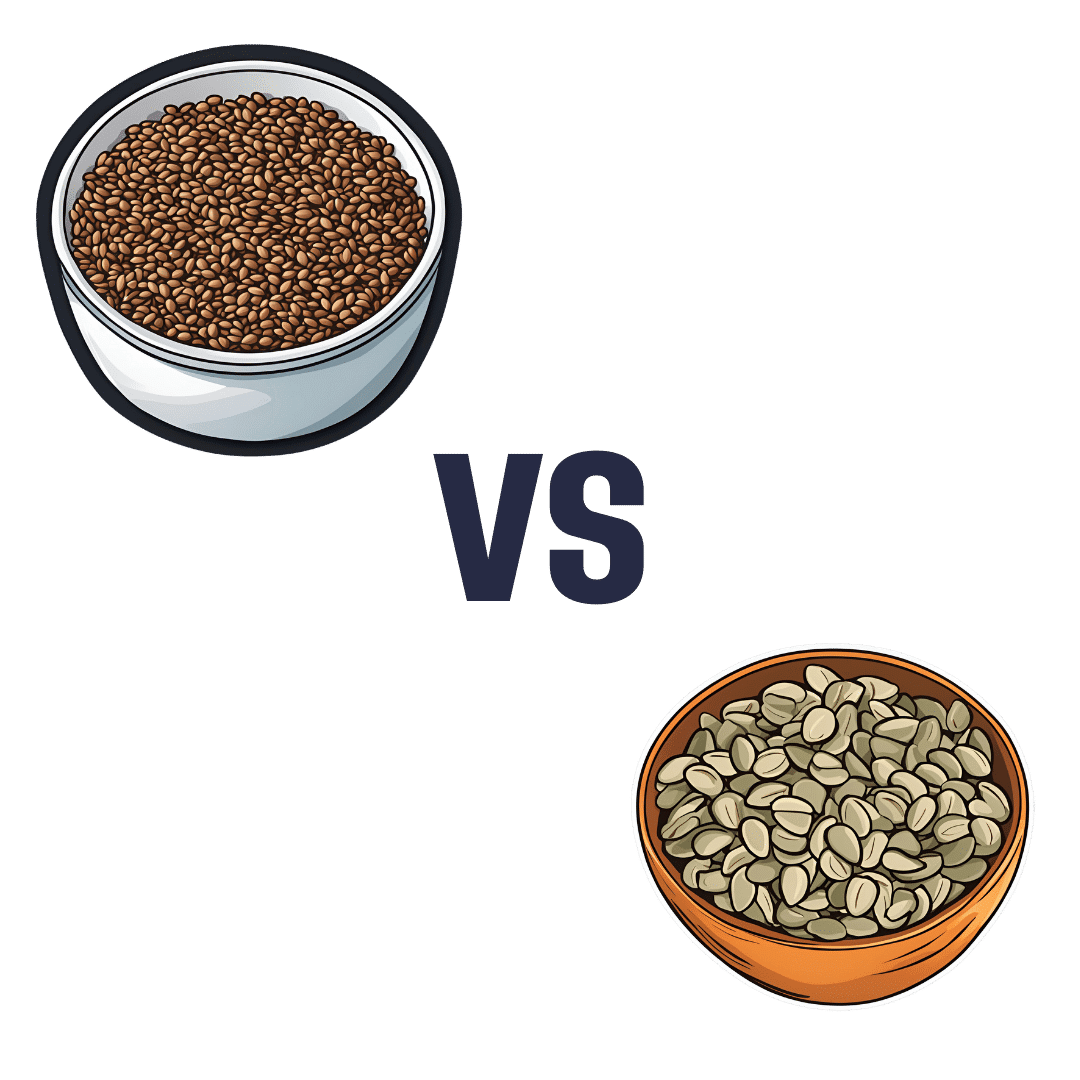
Flax Seeds vs Pumpkin Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing flax seeds to pumpkin seeds, we picked the flax.
Why?
Looking at the macros first, they are equal on protein, and flax seeds have a lot more fiber while pumpkin seeds have a lot more carbs. We’re going to prioritise fiber over carbs and call this a win for flax.
In terms of vitamins, flax seeds have a lot more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while pumpkin seeds have a tiny bit more vitamin A. An easy win for flax here.
When it comes to minerals, flax has multiples more calcium, copper, iron, magnesium, manganese, phosphorus, and selenium, while pumpkin seeds have more zinc. Another win for flax.
Adding up the sections makes for a clear overall win for flax, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score? ← seeds count as plants!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What you need to know about FLiRT, an emerging group of COVID-19 variants
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- COVID-19 wastewater levels are currently low, but a recent group of variants called FLiRT is making headlines.
- KP.2 is one of several FLiRT variants, and early lab tests suggest that it’s more infectious than JN.1.
- Getting infected with any COVID-19 variant can cause severe illness, heart problems, and death.
KP.2, a new COVID-19 variant, is now dominant in the United States. Lab tests suggest that it may be more infectious than JN.1, the variant that was dominant earlier this year.
Fortunately, there’s good news: Current wastewater data shows that COVID-19 infection rates are low. Still, experts are closely watching KP.2 to see if it will lead to an uptick in infections.
Read on to learn more about KP.2 and how to stay informed about COVID-19 cases in your area.
Where can I find data on COVID-19 cases in my area?
Hospitals are no longer required to report COVID-19 hospital admissions or hospital capacity to the Department of Health and Human Services. However, wastewater-based epidemiology (WBE) estimates the number of COVID-19 infections in a community based on the amount of COVID-19 viral particles detected in local wastewater.
View this map of wastewater data from the CDC to visualize COVID-19 infection rates throughout the U.S., or look up COVID-19 wastewater trends in your state.
What do we know so far about the new variant?
Early lab tests suggest that KP.2—one of a group of emerging variants called FLiRT—is similar to the previously dominant variant, JN.1, but it may be more infectious. If you had JN.1, you may still get reinfected with KP.2, especially if it’s been several months or longer since your last COVID-19 infection.
A CDC spokesperson said they have no reason to believe that KP.2 causes more severe illness than other variants. Experts are closely watching KP.2 to see if it will lead to an uptick in COVID-19 cases.
How can I protect myself from COVID-19 variants?
Staying up to date on COVID-19 vaccines reduces your risk of severe illness, long COVID, heart problems, and death. The CDC recommends that people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring.
Wearing a high-quality, well-fitting mask reduces your risk of contracting COVID-19 and spreading it to others. At indoor gatherings, improving ventilation by opening doors and windows, using high-efficiency particulate air (HEPA) filters, and building your own Corsi-Rosenthal box can also reduce the spread of COVID-19.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Why Do We Have Pores, And Could We Not?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Do we really need pores, and why are they bigger on the face?❞
Pores secrete sweat or sebum (there are different kinds of pores for each).
If we didn’t have sweat pores, we’d be unable to sweat, which superficially may seem like a bonus, but it’d make us prone to overheating (like dogs, pigs, and other mammals that cannot sweat).
If we didn’t have sebum pores (usually called hair follicles, which are supplied by a sebaceous gland), we’d be completely hairless, and also unable to supply our skin with natural oils that keep it healthy. So we’d have no hair and very unhappy skin.
Which is ironic, because to believe beauty magazines, we must at all costs minimize our pores (and indeed, interventions like botox* can kill them).
*Let’s give that its full name though:
Suffice it to say, we do not recommend getting injected with neurotoxins unless it is truly necessary to ward off a greater harm.
As for being bigger on the face, they need not be, but sebaceous glands are more active and numerous there, being most active and numerous in the face/forehead—which is why oily skin is more likely to appear there than other parts of the body.
If your facial sebaceous glands are too active for your liking…
…there are ways to reduce that, a simple and relatively gentle way (relative, for example, botox) is with retinoids, including retinols or retinoic acids. Here’s some of the science of that; the paper is about treating acne, but the mechanism of action is the same (down-regulating the sebaceous glands’ action):
The potential side-effects, however were noted as:
- Cheilitis
- Desquamation of the skin
- Pruritus
Which, in translation from sciencese, means:
- Chapped lips
- Flaky skin
- Itchiness
Which aren’t necessarily fun, which is why with retinoids are best taken in very small doses at first to see how your skin reacts.
Remember when we said what your skin would be like without pores? This is what would happen, only much worse.
Take care!
Share This Post
-
What’s the difference between period pain and endometriosis pain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menstruation, or a period, is the bleeding that occurs about monthly in healthy people born with a uterus, from puberty to menopause. This happens when the endometrium, the tissue that lines the inside of the uterus, is shed.
Endometriosis is a condition that occurs when endometrium-like tissue is found outside the uterus, usually within the pelvic cavity. It is often considered a major cause of pelvic pain.
Pelvic pain significantly impacts quality of life. But how can you tell the difference between period pain and endometriosis?
Polina Zimmerman/Pexels Periods and period pain
Periods involve shedding the 4-6 millimetre-thick endometrial lining from the inside of the uterus.
As the lining detaches from the wall of the uterus, the blood vessels which previously supplied the lining bleed. The uterine muscles contract, expelling the blood and crumbled endometrium.
The crumbled endometrium and blood mostly pass through the cervix and vagina. But almost everyone back-bleeds via their fallopian tubes into their pelvic cavity. This is known as “retrograde menstruation”.
Most of the lining is shed through the vagina. Andrey_Popov/Shutterstock The process of menstrual shedding is caused by inflammatory substances, which also cause nausea, vomiting, diarrhoea, headaches, aches, pains, dizziness, feeling faint, as well as stimulating pain receptors.
These inflammatory substances are responsible for the pain and symptoms in the week before a period and the first few days.
For women with heavy periods, their worst days of pain are usually the heaviest days of their period, coinciding with more cramps to expel clots and more retrograde bleeding.
Many women also have pain when they are releasing an egg from their ovary at the time of ovulation. Ovulation or mid-cycle pain can be worse in those who bleed more, as those women are more likely to bleed into the ovulation follicle.
Around 90% of adolescents experience period pain. Among these adolescents, 20% will experience such severe period pain they need time off from school and miss activities. These symptoms are too often normalised, without validation or acknowledgement.
What about endometriosis?
Many symptoms have been attributed to endometriosis, including painful periods, pain with sex, bladder and bowel-related pain, low back pain and thigh pain.
Other pain-related conditions such migraines and chronic fatigue have also been linked to endometriosis. But these other pain-related symptoms occur equally often in people with pelvic pain who don’t have endometriosis.
One in five adolescents who menstrate experience severe symptoms. CGN089/Shutterstock Repeated, significant period and ovulation pain can eventually lead some people to develop persistent or chronic pelvic pain, which lasts longer than six months. This appears to occur through a process known as central sensitisation, where the brain becomes more sensitive to pain and other sensory stimuli.
Central sensitisation can occur in people with persistent pain, independent of the presence or absence of endometriosis.
Eventually, many people with period and/or persistent pelvic pain will have an operation called a laparoscopy, which allows surgeons to examine organs in the pelvis and abdomen, and diagnose and treat endometriosis.
Yet only 50% of those with identical pain symptoms who undergo a laparoscopy will end up having endometriosis.
Endometriosis is also found in pain-free women. So we cannot predict who does and doesn’t have endometriosis from symptoms alone.
How is this pain managed?
Endometriosis surgery usually involves removing lesions and adhesions. But at least 30% of people return to pre-surgery pain levels within six months or have more pain than before.
After surgery, emergency department presentations for pain are unchanged and 50% have repeat surgery within a few years.
Suppressing periods using hormonal therapies (such as continuous oral contraceptive pills or progesterone-only approaches) can suppress endometriosis and reduce or eliminate pain, independent of the presence or absence of endometriosis.
Not every type or dose of hormonal medications suits everyone, so medications need to be individualised.
The current gold-standard approach to manage persistent pelvic pain involves a multidisciplinary team approach, with the aim of achieving sustained remission and improving quality of life. This may include:
- physiotherapy for pelvic floor and other musculoskeletal problems
- management of bladder and bowel symptoms
- support for self-managing pain
- lifestyle changes including diet and exercise
- psychological or group therapy, as our moods, stress levels and childhood events can affect how we feel and experience pain.
Whether you have period pain, chronic pelvic pain or pain you think is associated with endometriosis, if you feel pain, it’s real. If it’s disrupting your life, you deserve to be taken seriously and treated as the whole person you are.
Sonia R. Grover, Senior Research Fellow, Murdoch Children’s Research Institute; Clinical Professor of Gynaecology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
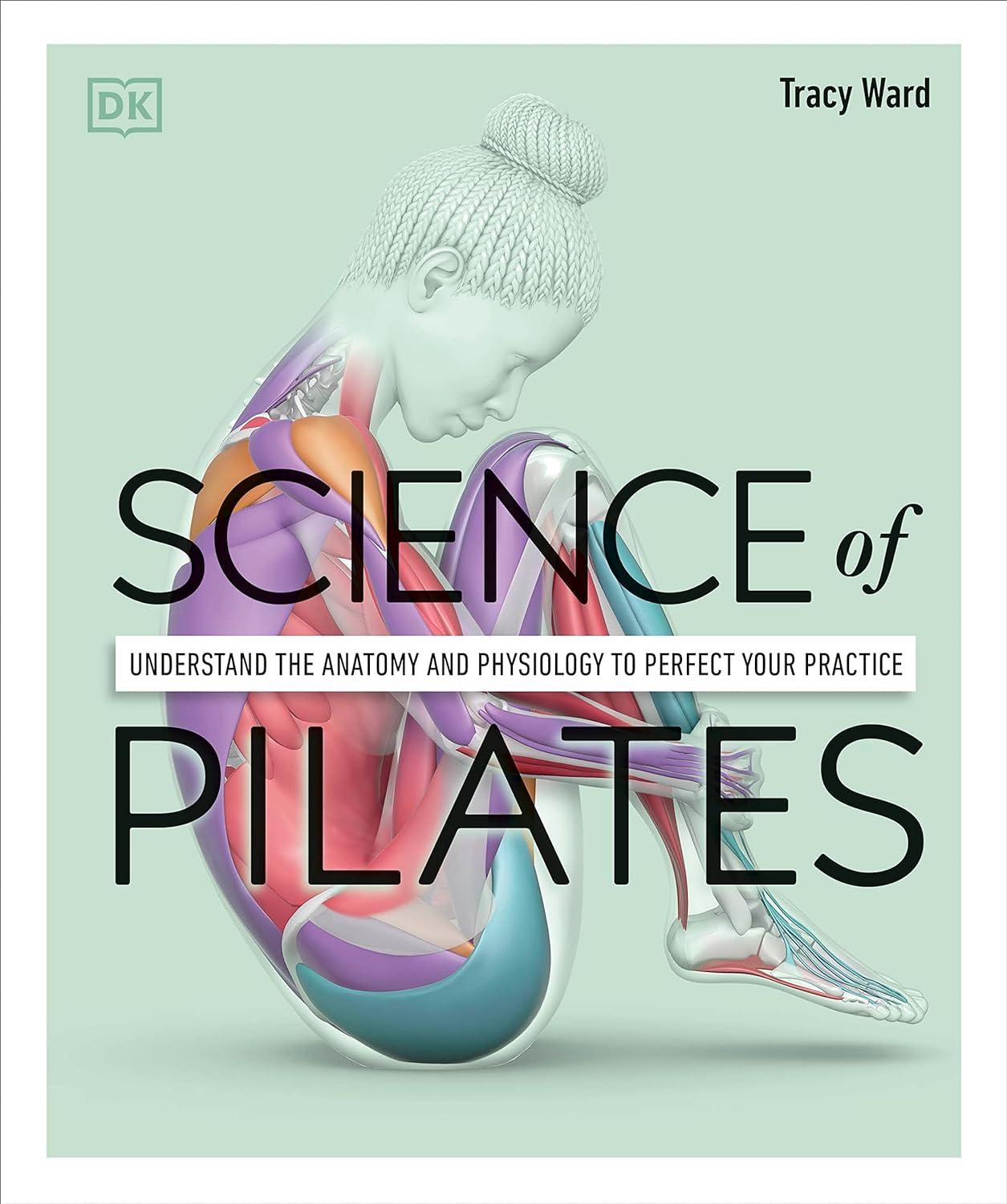
Science of Pilates – by Tracy Ward
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other books in this series, “Science of Yoga” and “Science of HIIT” (they’re great too; check them out!). What does this one add to the mix?
Pilates is a top-tier “combination exercise” insofar as it checks a lot of boxes, e.g:
- Strength—especially core strength, but also limbs
- Mobility—range of motion and resultant reduction in injury risk
- Stability—impossible without the above two things, but Pilates trains this too
- Fitness—many dynamic Pilates exercises can be performed as cardio and/or HIIT.
The author, a physiotherapist, explains (as the title promises!) the science of Pilates, with:
- the beautifully clear diagrams we’ve come to expect of this series,
- equally clear explanations, with a great balance of simplicity of terms and depth where necessary, and
- plenty of citations for the claims made, linking to lots of the best up-to-date science.
Bottom line: if you are in a position to make a little time for Pilates (if you don’t already), then there is nobody who would not benefit from reading this book.
Click here to check out Science of Pilates, and keep your body well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ricezempic: is there any evidence this TikTok trend will help you lose weight?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you spend any time looking at diet and lifestyle content on social media, you may well have encountered a variety of weight loss “hacks”.
One of the more recent trends is a home-made drink called ricezempic, made by soaking uncooked rice and then straining it to drink the leftover starchy water. Sounds delicious, right?
Its proponents claim it leads to weight loss by making you feel fuller for longer and suppressing your appetite, working in a similar way to the sought-after drug Ozempic – hence the name.
So does this drink actually mimic the weight loss effects of Ozempic? Spoiler alert – probably not. But let’s look at what the evidence tells us.
New Africa/Shutterstock How do you make ricezempic?
While the recipe can vary slightly depending on who you ask, the most common steps to make ricezempic are:
- soak half a cup of white rice (unrinsed) in one cup of warm or hot water up to overnight
- drain the rice mixture into a fresh glass using a strainer
- discard the rice (but keep the starchy water)
- add the juice of half a lime or lemon to the starchy water and drink.
TikTokers advise that best results will happen if you drink this concoction once a day, first thing in the morning, before eating.
The idea is that the longer you consume ricezempic for, the more weight you’ll lose. Some claim introducing the drink into your diet can lead to a weight loss of up to 27 kilograms in two months.
Resistant starch
Those touting ricezempic argue it leads to weight loss because of the resistant starch rice contains. Resistant starch is a type of dietary fibre (also classified as a prebiotic). There’s no strong evidence it makes you feel fuller for longer, but it does have proven health benefits.
Studies have shown consuming resistant starch may help regulate blood sugar, aid weight loss and improve gut health.
Research has also shown eating resistant starch reduces the risk of obesity, diabetes, heart disease and other chronic diseases.
Ricezempic is made by soaking rice in water. Kristi Blokhin/Shutterstock Resistant starch is found in many foods. These include beans, lentils, wholegrains (oats, barley, and rice – particularly brown rice), bananas (especially when they’re under-ripe or green), potatoes, and nuts and seeds (particularly chia seeds, flaxseeds and almonds).
Half a cup of uncooked white rice (as per the ricezempic recipe) contains around 0.6 grams of resistant starch. For optimal health benefits, a daily intake of 15–20 grams of resistant starch is recommended. Although there is no concrete evidence on the amount of resistant starch that leaches from rice into water, it’s likely to be significantly less than 0.6 grams as the whole rice grain is not being consumed.
Ricezempic vs Ozempic
Ozempic was originally developed to help people with diabetes manage their blood sugar levels but is now commonly used for weight loss.
Ozempic, along with similar medications such as Wegovy and Trulicity, is a glucagon-like peptide-1 (GLP-1) receptor agonist. These drugs mimic the GLP-1 hormone the body naturally produces. By doing so, they slow down the digestive process, which helps people feel fuller for longer, and curbs their appetite.
While the resistant starch in rice could induce some similar benefits to Ozempic (such as feeling full and therefore reducing energy intake), no scientific studies have trialled ricezempic using the recipes promoted on social media.
Ozempic has a long half-life, remaining active in the body for about seven days. In contrast, consuming one cup of rice provides a feeling of fullness for only a few hours. And simply soaking rice in water and drinking the starchy water will not provide the same level of satiety as eating the rice itself.
Other ways to get resistant starch in your diet
There are several ways to consume more resistant starch while also gaining additional nutrients and vitamins compared to what you get from ricezempic.
1. Cooked and cooled rice
Letting cooked rice cool over time increases its resistant starch content. Reheating the rice does not significantly reduce the amount of resistant starch that forms during cooling. Brown rice is preferable to white rice due to its higher fibre content and additional micronutrients such as phosphorus and magnesium.
2. More legumes
These are high in resistant starch and have been shown to promote weight management when eaten regularly. Why not try a recipe that has pinto beans, chickpeas, black beans or peas for dinner tonight?
3. Cooked and cooled potatoes
Cooking potatoes and allowing them to cool for at least a few hours increases their resistant starch content. Fully cooled potatoes are a rich source of resistant starch and also provide essential nutrients like potassium and vitamin C. Making a potato salad as a side dish is a great way to get these benefits.
In a nutshell
Although many people on social media have reported benefits, there’s no scientific evidence drinking rice water or “ricezempic” is effective for weight loss. You probably won’t see any significant changes in your weight by drinking ricezempic and making no other adjustments to your diet or lifestyle.
While the drink may provide a small amount of resistant starch residue from the rice, and some hydration from the water, consuming foods that contain resistant starch in their full form would offer significantly more nutritional benefits.
More broadly, be wary of the weight loss hacks you see on social media. Achieving lasting weight loss boils down to gradually adopting healthy eating habits and regular exercise, ensuring these changes become lifelong habits.
Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University and Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your friend has been diagnosed with cancer. Here are 6 things you can do to support them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Across the world, one in five people are diagnosed with cancer during their lifetime. By age 85, almost one in two Australians will be diagnosed with cancer.
When it happens to someone you care about, it can be hard to know what to say or how to help them. But providing the right support to a friend can make all the difference as they face the emotional and physical challenges of a new diagnosis and treatment.
Here are six ways to offer meaningful support to a friend who has been diagnosed with cancer.
1. Recognise and respond to emotions
When facing a cancer diagnosis and treatment, it’s normal to experience a range of emotions including fear, anger, grief and sadness. Your friend’s moods may fluctuate. It is also common for feelings to change over time, for example your friend’s anxiety may decrease, but they may feel more depressed.
Spending time together can mean a lot to someone who is feeling isolated during cancer treatment. Chokniti-Studio/Shutterstock Some friends may want to share details while others will prefer privacy. Always ask permission to raise sensitive topics (such as changes in physical appearance or their thoughts regarding fears and anxiety) and don’t make assumptions. It’s OK to tell them you feel awkward, as this acknowledges the challenging situation they are facing.
When they feel comfortable to talk, follow their lead. Your support and willingness to listen without judgement can provide great comfort. You don’t have to have the answers. Simply acknowledging what has been said, providing your full attention and being present for them will be a great help.
2. Understand their diagnosis and treatment
Understanding your friend’s diagnosis and what they’ll go through when being treated may be helpful.
Being informed can reduce your own worry. It may also help you to listen better and reduce the amount of explaining your friend has to do, especially when they’re tired or overwhelmed.
Explore reputable sources such as the Cancer Council website for accurate information, so you can have meaningful conversations. But keep in mind your friend has a trusted medical team to offer personalised and accurate advice.
3. Check in regularly
Cancer treatment can be isolating, so regular check-ins, texts, calls or visits can help your friend feel less alone.
Having a normal conversation and sharing a joke can be very welcome. But everyone copes with cancer differently. Be patient and flexible in your support – some days will be harder for them than others.
Remembering key dates – such as the next round of chemotherapy – can help your friend feel supported. Celebrating milestones, including the end of treatment or anniversary dates, may boost morale and remind your friend of positive moments in their cancer journey.
Always ask if it’s a good time to visit, as your friend’s immune system may be compromised by their cancer or treatments such as chemotherapy or radiotherapy. If you’re feeling unwell, it’s best to postpone visits – but they may still appreciate a call or text.
4. Offer practical support
Sometimes the best way to show your care is through practical support. There may be different ways to offer help, and what your friend needs might change at the beginning, during and after treatment.
For example, you could offer to pick up prescriptions, drive them to appointments so they have transport and company to debrief, or wait with them at appointments.
Meals will always be welcome. However it’s important to remember cancer and its treatments may affect taste, smell and appetite, as well as your friend’s ability to eat enough or absorb nutrients. You may want to check first if there are particular foods they like. Good nutrition can help boost their strength while dealing with the side effects of treatment.
There may also be family responsibilities you can help with, for example, babysitting kids, grocery shopping or taking care of pets.
There may be practical ways you can help, such as dropping off meals. David Trinks/Unsplash 5. Explore supports together
Studies have shown mindfulness practices can be an effective way for people to manage anxiety associated with a cancer diagnosis and its treatment.
If this is something your friend is interested in, it may be enjoyable to explore classes (either online or in-person) together.
You may also be able to help your friend connect with organisations that provide emotional and practical help, such as the Cancer Council’s support line, which offers free, confidential information and support for anyone affected by cancer, including family, friends and carers.
Peer support groups can also reduce your friend’s feelings of isolation and foster shared understanding and empathy with people who’ve gone through a similar experience. GPs can help with referrals to support programs.
6. Stick with them
Be committed. Many people feel isolated after their treatment. This may be because regular appointments have reduced or stopped – which can feel like losing a safety net – or because their relationships with others have changed.
Your friend may also experience emotions such as worry, lack of confidence and uncertainty as they adjust to a new way of living after their treatment has ended. This will be an important time to support your friend.
But don’t forget: looking after yourself is important too. Making sure you eat well, sleep, exercise and have emotional support will help steady you through what may be a challenging time for you, as well as the friend you love.
Our research team is developing new programs and resources to support carers of people who live with cancer. While it can be a challenging experience, it can also be immensely rewarding, and your small acts of kindness can make a big difference.
Stephanie Cowdery, Research Fellow, Carer Hub: A Centre of Excellence in Cancer Carer Research, Translation and Impact, Deakin University; Anna Ugalde, Associate Professor & Victorian Cancer Agency Fellow, Deakin University; Trish Livingston, Distinguished Professor & Director of Special Projects, Faculty of Health, Deakin University, and Victoria White, Professor of Pyscho-Oncology, School of Psychology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: