Fix Tight Hamstrings In Just 3 Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a better way to increase your flexibility than just stretching and stretching and hoping for the best. Here’s a 3-step method that will transform your flexibility:
As easy as 1-2-3
Only one part actually involves stretching:
Step 1: reciprocal inhibition
- Concept: when one muscle contracts, the opposing muscle relaxes—which is what we need.
- Goal: engage hip flexors to encourage hamstring relaxation.
- Method:
- Kneeling hamstring stretch position with one leg forward.
- Support with yoga blocks or a chair; use a cushion for comfort.
- Maintain a slight arch in the lower back and hinge forward slightly.
- Attempt to lift the foot off the floor, even if it doesn’t move.
- Hold for around 10 seconds.
Step 2: engaging more muscle fibers
- Concept: our muscles contain a lot of fibers, and often not all of them come along for the ride when we do something (exercising, stretching, etc), and those fibers that weren’t engaged will hold back the whole process.
- Goal: activate more fibers in the hamstring for a deeper stretch.
- Method:
- Same kneeling position, slight back arch, and forward hinge.
- Drive the heel into the floor as if trying to dent it.
- Apply significant effort but hold for only 10 seconds.
- A small bend in the knee is acceptable.
Step 3: manipulating the nervous system
- Concept: the nervous system often limits flexibility due to safety signals (causing sensations of discomfort to tell us to stop a lot sooner than we really need to).
- Goal: passive stretching to reduce nervous system resistance.
- Method:
- Avoid muscle engagement or movement—stay completely relaxed.
- Focus on calmness, with slow, steady breaths.
- Avoid signs of tension (e.g. clenched fists, short/sharp breathing). While your nervous system is trying to communicate to you that you are in danger, you need to communicate to your nervous system that this is fine actually, so in order to reassure your nervous system you need to avoid signs that will tip it off that you’re worried too.
- Don’t overstretch; prioritize a relaxed, safe feeling.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strategic Wellness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strategic Wellness: planning ahead for a better life!
This is Dr. Michael Roizen. With hundreds of peer-reviewed publications and 14 US patents, his work has been focused on the importance of lifestyle factors in healthy living. He’s the Chief Wellness Officer at the world-famous Cleveland Clinic, and is known for his “RealAge” test and related personalized healthcare services.
If you’re curious about that, you can take the RealAge test here.
(they will require you inputting your email address if you do, though)
What’s his thing?
Dr. Roizen is all about optimizing health through lifestyle factors—most notably, diet and exercise. Of those, he is particularly keen on optimizing nutritional habits.
Is this just the Mediterranean Diet again?
Nope! Although: he does also advocate for that. But there’s more, he makes the case for what he calls “circadian eating”, optimally timing what we eat and when.
Is that just Intermittent Fasting again?
Nope! Although: he does also advocate for that. But there’s more:
Dr. Roizen takes a more scientific approach. Which isn’t to say that intermittent fasting is unscientific—on the contrary, there’s mountains of evidence for it being a healthful practice for most people. But while people tend to organize their intermittent fasting purely according to convenience, he notes some additional factors to take into account, including:
- We are evolved to eat when the sun is up
- We are evolved to be active before eating (think: hunting and gathering)
- Our insulin resistance increases as the day goes on
Now, if you’ve a quick mind about you, you’ll have noticed that this means:
- We should keep our eating to a particular time window (classic intermittent fasting), and/but that time window should be while the sun is up
- We should not roll out of bed and immediately breakfast; we need to be active for a bit first (moderate exercise is fine—this writer does her daily grocery-shopping trip on foot before breakfast, for instance… getting out there and hunting and gathering those groceries!)
- We should not, however, eat too much later in the day (so, dinner should be the smallest meal of the day)
The latter item is the one that’s perhaps biggest change for most people. His tips for making this as easy as possible include:
- Over-cater for dinner, but eat only one portion of it, and save the rest for an early-afternoon lunch
- First, however, enjoy a nutrient-dense protein-centric breakfast with at least some fibrous vegetation, for example:
- Salmon and asparagus
- Scrambled tofu and kale
- Yogurt and blueberries
Enjoy!
Share This Post
-
Accidental falls in the older adult population: What academic research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Accidental falls are among the leading causes of injury and death among adults 65 years and older worldwide. As the aging population grows, researchers expect to see an increase in the number of fall injuries and related health spending.
Falls aren’t unique to older adults. Nealy 684,000 people die from falls each year globally. Another 37.3 million people each year require medical attention after a fall, according to the World Health Organization. But adults 65 and older account for the greatest number of falls.
In the United States, more than 1 in 4 older adults fall each year, according to the National Institute on Aging. One in 10 report a fall injury. And the risk of falling increases with age.
In 2022, health care spending for nonfatal falls among older adults was $80 billion, according to a 2024 study published in the journal Injury Prevention.
Meanwhile, the fall death rate in this population increased by 41% between 2012 and 2021, according to the latest CDC data.
“Unfortunately, fall-related deaths are increasing and we’re not sure why that is,” says Dr. Jennifer L. Vincenzo, an associate professor at the University of Arkansas for Medical Sciences in the department of physical therapy and the Center for Implementation Research. “So, we’re trying to work more on prevention.”
Vincenzo advises journalists to write about how accidental falls can be prevented. Remind your audiences that accidental falls are not an inevitable consequence of aging, and that while we do decline in many areas with age, there are things we can do to minimize the risk of falls, she says. And expand your coverage beyond the national Falls Prevention Awareness Week, which is always during the first week of fall — Sept. 23 to 27 this year.
Below, we explore falls among older people from different angles, including injury costs, prevention strategies and various disparities. We have paired each angle with data and research studies to inform your reporting.
Falls in older adults
In 2020, 14 million older adults in the U.S. reported falling during the previous year. In 2021, more than 38,700 older adults died due to unintentional falls, according to the CDC.
A fall could be immediately fatal for an older adult, but many times it’s the complications from a fall that lead to death.
The majority of hip fractures in older adults are caused by falls, Vincenzo says, and “it could be that people aren’t able to recover [from the injury], losing function, maybe getting pneumonia because they’re not moving around, or getting pressure injuries,” she says.
In addition, “sometimes people restrict their movement and activities after a fall, which they think is protective, but leads to further functional declines and increases in fall risk,” she adds.
Factors that can cause a fall include:
- Poor eyesight, reflexes and hearing. “If you cannot hear as well, anytime you’re doing something in your environment and there’s a noise, it will be really hard for you to focus on hearing what that noise is and what it means and also moving at the same time,” Vincenzo says.
- Loss of strength, balance, and mobility with age, which can lessen one’s ability to prevent a fall when slipping or tripping.
- Fear of falling, which usually indicates decreased balance.
- Conditions such as diabetes, heart disease, or problems with nerves or feet that can affect balance.
- Conditions like incontinence that cause rushed movement to the bathroom.
- Cognitive impairment or certain types of dementia.
- Unsafe footwear such as backless shoes or high heels.
- Medications or medication interactions that can cause dizziness or confusion.
- Safety hazards in the home or outdoors, such as poor lighting, steps and slippery surfaces.
Related Research
Nonfatal and Fatal Falls Among Adults Aged ≥65 Years — United States, 2020–2021
Ramakrishna Kakara, Gwen Bergen, Elizabeth Burns and Mark Stevens. Morbidity and Mortality Weekly Report, September 2023.Summary: Researchers analyzed data from the 2020 Behavioral Risk Factor Surveillance System — a landline and mobile phone survey conducted each year in all 50 U.S. states and the District of Columbia — and data from the 2021 National Vital Statistics System to identify patterns of injury and death due to falls in the U.S. by sex and state for adults 65 years and older. Among the findings:
- The percentage of women who reported falling was 28.9%, compared with 26.1% of men.
- Death rates from falls were higher among white and American Indian or Alaska Native older adults than among older adults from other racial and ethnic groups.
- In 2020, the percentage of older adults who reported falling during the past year ranged from 19.9% in Illinois to 38.0% in Alaska. The national estimate for 18 states was 27.6%.
- In 2021, the unintentional fall-related death rate among older adults ranged from 30.7 per 100,000 older adults in Alabama to 176.5 in Wisconsin. The national estimate for 26 states was 78.
“Although common, falls among older adults are preventable,” the authors write. “Health care providers can talk with patients about their fall risk and how falls can be prevented.”
Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years — United States, 2012-2018
Briana Moreland, Ramakrishna Kakara and Ankita Henry. Morbidity and Mortality Weekly Report, July 2020.Summary: Researchers compared data from the 2018 Behavioral Risk Factor Surveillance System. Among the findings:
- The percentage of older adults reporting a fall increased from 2012 to 2016, then slightly decreased from 2016 to 2018.
- Even with this decrease in 2018, older adults reported 35.6 million falls. Among those falls, 8.4 million resulted in an injury that limited regular activities for at least one day or resulted in a medical visit.
“Despite no significant changes in the rate of fall-related injuries from 2012 to 2018, the number of fall-related injuries and health care costs can be expected to increase as the proportion of older adults in the United States grows,” the authors write.
Understanding Modifiable and Unmodifiable Older Adult Fall Risk Factors to Create Effective Prevention Strategies
Gwen Bergen, et al. American Journal of Lifestyle Medicine, October 2019.Summary: Researchers used data from the 2016 U.S. Behavioral Risk Factor Surveillance System to better understand the association between falls and fall injuries in older adults and factors such as health, state and demographic characteristics. Among the findings:
- Depression had the strongest association with falls and fall injuries. About 40% of older adults who reported depression also reported at least one fall; 15% reported at least one fall injury.
- Falls and depression have several factors in common, including cognitive impairment, slow walking speed, poor balance, slow reaction time, weakness, low energy and low levels of activity.
- Other factors associated with an increased risk of falling include diabetes, vision problems and arthritis.
“The multiple characteristics associated with falls suggest that a comprehensive approach to reducing fall risk, which includes screening and assessing older adult patients to determine their unique, modifiable risk factors and then prescribing tailored care plans that include evidence-based interventions, is needed,” the authors write.
Health care use and cost
In addition to being the leading cause of injury, falls are the leading cause of hospitalization in older adults. Each year, about 3 million older adults visit the emergency department due to falls. More than 1 million get hospitalized.
In 2021, falls led to more than 38,000 deaths in adults 65 and older, according to the CDC.
The annual financial medical toll of falls among adults 65 years and older is expected to be more than $101 billion by 2030, according to the National Council on Aging, an organization advocating for older Americans.
Related research
Healthcare Spending for Non-Fatal Falls Among Older Adults, USA
Yara K. Haddad, et al. Injury Prevention, July 2024.Summary: In 2015, health care spending related to falls among older adults was roughly $50 billion. This study aims to update the estimate, using the 2017, 2019 and 2021 Medicare Current Beneficiary Survey, the most comprehensive and complete survey available on the Medicare population. Among the findings:
- In 2020, health care spending for non-fatal falls among older adults was $80 billion.
- Medicare paid $53.3 billion of the $80 billion, followed by $23.2 billion paid by private insurance or patients and $3.5 billion by Medicaid.
“The burden of falls on healthcare systems and healthcare spending will continue to rise if the risk of falls among the aging population is not properly addressed,” the authors write. “Many older adult falls can be prevented by addressing modifiable fall risk factors, including health and functional characteristics.”
Cost of Emergency Department and Inpatient Visits for Fall Injuries in Older Adults Lisa Reider, et al. Injury, February 2024.
Summary: The researchers analyzed data from the 2016-2018 National Inpatient Sample and National Emergency Department Sample, which are large, publicly available patient databases in the U.S. that include all insurance payers such as Medicare and private insurance. Among the findings:
- During 2016-2018, more than 920,000 older adults were admitted to the hospital and 2.3 million visited the emergency department due to falls. The combined annual cost was $19.2 billion.
- More than half of hospital admissions were due to bone fractures. About 14% of these admissions were due to multiple fractures and cost $2.5 billion.
“The $20 billion in annual acute treatment costs attributed to fall injury indicate an urgent need to implement evidence-based fall prevention interventions and underscores the importance of newly launched [emergency department]-based fall prevention efforts and investments in geriatric emergency departments,” the authors write.
Hip Fracture-Related Emergency Department Visits, Hospitalizations and Deaths by Mechanism of Injury Among Adults Aged 65 and Older, United States 2019
Briana L. Moreland, Jaswinder K. Legha, Karen E. Thomas and Elizabeth R. Burns. Journal of Aging and Health, June 2024.Summary: The researchers calculated hip fracture-related U.S. emergency department visits, hospitalizations and deaths among older adults, using data from the Healthcare Cost and Utilization Project and the National Vital Statistics System. Among the findings:
- In 2019, there were 318,797 emergency department visits, 290,130 hospitalizations and 7,731 deaths related to hip fractures among older adults.
- Nearly 88% of emergency department visits and hospitalizations and 83% of deaths related to hip fractures were caused by falls.
- These rates were highest among those living in rural areas and among adults 85 and older. More specifically, among adults 85 and older, the rate of hip fracture-related emergency department visits was nine times higher than among adults between 65 and 74 years old.
“Falls are common among older adults, but many are preventable,” the authors write. “Primary care providers can prevent falls among their older patients by screening for fall risk annually or after a fall, assessing modifiable risk factors such as strength and balance issues, and offering evidence-based interventions to reduce older adults’ risk of falls.”
Fall prevention
Several factors, including exercising, managing medication, checking vision and making homes safer can help prevent falls among older adults.
“Exercise is one of the best interventions we know of to prevent falls,” Vincenzo says. But “walking in and of itself will not help people to prevent falls and may even increase their risk of falling if they are at high risk of falls.”
The National Council on Aging also has a list of evidence-based fall prevention programs, including activities and exercises that are shown to be effective.
The National Institute on Aging has a room-by-room guide on preventing falls at home. Some examples include installing grab bars near toilets and on the inside and outside of the tub and shower, sitting down while preparing food to prevent fatigue, and keeping electrical cords near walls and away from walking paths.
There are also national and international initiatives to help prevent falls.
Stopping Elderly Accidents, Deaths and Injuries, or STEADI, is an initiative by the CDC’s Injury Center to help health care providers who treat older adults. It helps providers screen patients for fall risk, assess their fall risk factors and reduce their risk by using strategies that research has shown to be effective. STEADI’s guidelines are in line with the American and British Geriatric Societies’ Clinical Practice Guidelines for fall prevention.
“We’re making some iterations right now to STEADI that will come out in the next couple of years based on the World Falls Guidelines, as well as based on clinical providers’ feedback on how to make [STEADI] more feasible,” Vincenzo says.
The World Falls Guidelines is an international initiative to prevent falls in older adults. The guidelines are the result of the work of 14 international experts who came together in 2019 to consider whether new guidelines on fall prevention were needed. The task force then brought together 96 experts from 39 countries across five continents to create the guidelines.
The CDC’s STEADI initiative has a screening questionnaire for consumers to check their risk of falls, as does the National Council on Aging.
On the policy side, U.S. Rep. Carol Miller, R-W.V., and Melanie Stansbury, D-N.M., introduced the Stopping Addiction and Falls for the Elderly (SAFE) Act in March 2024. The bill would allow occupational and physical therapists to assess fall risks in older adults as part of the Medicare Annual Wellness Benefit. The bill was sent to the House Subcommittee on Health in the same month.
Meanwhile, older adults’ attitudes toward falls and fall prevention are also pivotal. For many, coming to terms with being at risk of falls and making changes such as using a cane, installing railings at home or changing medications isn’t easy for all older adults, studies show.
“Fall is a four-letter F-word in a way to older adults,” says Vincenzo, who started her career as a physical therapist. “It makes them feel ‘old.’ So, it’s a challenge on multiple fronts: U.S. health care infrastructure, clinical and community resources and facilitating health behavior change.”
Related research
Environmental Interventions for Preventing Falls in Older People Living in the Community
Lindy Clemson, et al. Cochrane Database of Systematic Reviews, March 2023.Summary: This review includes 22 studies from 10 countries involving a total of 8,463 older adults who live in the community, which includes their own home, a retirement facility or an assisted living facility, but not a hospital or nursing home. Among the findings:
- Removing fall hazards at home reduced the number of falls by 38% among older adults at a high risk of having a fall, including those who have had a fall in the past year, have been hospitalized or need support with daily activities. Examples of fall hazards at home include a stairway without railings, a slippery pathway or poor lighting.
- It’s unclear whether checking prescriptions for eyeglasses, wearing special footwear or installing bed alarm systems reduces the rate of falls.
- It’s also not clear whether educating older adults about fall risks reduces their fall risk.
The Influence of Older Adults’ Beliefs and Attitudes on Adopting Fall Prevention Behaviors
Judy A. Stevens, David A. Sleet and Laurence Z. Rubenstein. American Journal of Lifestyle Medicine. January 2017.Summary: Persuading older adults to adopt interventions that reduce their fall risk is challenging. Their attitudes and beliefs about falls play a large role in how well they accept and adopt fall prevention strategies, the authors write. Among the common attitudes and beliefs:
- Many older adults believe that falls “just happen,” are a normal result of aging or are simply due to bad luck.
- Many don’t acknowledge or recognize their fall risk.
- For many, falls are considered to be relevant only for frail or very old people.
- Many believe that their home environment or daily activities can be a risk for fall, but do not consider biological factors such as dizziness or muscle weakness.
- For many, fall prevention simply consists of “being careful” or holding on to things when moving about the house.
“To reduce falls, health care practitioners have to help patients understand and acknowledge their fall risk while emphasizing the positive benefits of fall prevention,” the authors write. “They should offer patients individualized fall prevention interventions as well as provide ongoing support to help patients adopt and maintain fall prevention strategies and behaviors to reduce their fall risk. Implementing prevention programs such as CDC’s STEADI can help providers discuss the importance of falls and fall prevention with their older patients.”
Reframing Fall Prevention and Risk Management as a Chronic Condition Through the Lens of the Expanded Chronic Care Model: Will Integrating Clinical Care and Public Health Improve Outcomes?
Jennifer L. Vincenzo, Gwen Bergen, Colleen M. Casey and Elizabeth Eckstrom. The Gerontologist, June 2024.Summary: The authors recommend approaching fall prevention from the lens of chronic disease management programs because falls and fall risk are chronic issues for many older adults.
“Policymakers, health systems, and community partners can consider aligning fall risk management with the [Expanded Chronic Care Model], as has been done for diabetes,” the authors write. “This can help translate high-quality research on the effectiveness of fall prevention interventions into daily practice for older adults to alter the trajectory of older adult falls and fall-related injuries.”
Disparities
Older adults face several barriers to reducing their fall risk. Accessing health care services and paying for services such as physical therapy is not feasible for everyone. Some may lack transportation resources to go to and from medical appointments. Social isolation can increase the risk of death from falls. In addition, physicians may not have the time to fit in a fall risk screening while treating older patients for other health concerns.
Moreover, implementing fall risk screening, assessment and intervention in the current U.S. health care structure remains a challenge, Vincenzo says.
Related research
Mortality Due to Falls by County, Age Group, Race, and Ethnicity in the USA, 2000-19: A Systematic Analysis of Health Disparities
Parkes Kendrick, et al. The Lancet Public Health, August 2024.Summary: Researchers analyzed death registration data from the U.S. National Vital Statistics System and population data from the U.S. National Center for Health Statistics to estimate annual fall-related mortality. The data spanned from 2000 to 2019 and includes all age groups. Among the findings:
- The disparities between racial and ethnic populations varied widely by age group. Deaths from falls among younger adults were highest for the American Indian/Alaska Native population, while among older adults it was highest for the white population.
- For older adults, deaths from falls were particularly high in the white population within clusters of counties across states including Florida, Minnesota and Wisconsin.
- One factor that could contribute to higher death rates among white older adults is social isolation, the authors write. “Studies suggest that older Black and Latino adults are more likely to have close social support compared with older white adults, while AIAN and Asian individuals might be more likely to live in multigenerational households,” they write.
“Among older adults, current prevention techniques might need to be restructured to reduce frailty by implementing early prevention and emphasizing particularly successful interventions. Improving social isolation and evaluating the effectiveness of prevention programs among minoritized populations are also key,” the authors write.
Demographic Comparisons of Self-Reported Fall Risk Factors Among Older Adults Attending Outpatient Rehabilitation
Mariana Wingood, et al. Clinical Interventions in Aging, February 2024.Summary: Researchers analyzed the electronic health record data of 108,751 older adults attending outpatient rehabilitation within a large U.S. health care system across seven states, between 2018 and 2022. Among the findings:
- More than 44% of the older adults were at risk of falls; nearly 35% had a history of falls.
- The most common risk factors for falls were diminished strength, gait and balance.
- Compared to white older adults, Native American/Alaska Natives had the highest prevalence of fall history (43.8%) and Hispanics had the highest prevalence of falls with injury (56.1%).
“Findings indicate that rehabilitation providers should perform screenings for these impairments, including incontinence and medication among females, loss of feeling in the feet among males, and all Stay Independent Questionnaire-related fall risk factors among Native American/Alaska Natives, Hispanics, and Blacks,” the authors write.
Resources and articles
- National Institute on Aging
- National Council on Aging
- Gerontological Society of America
- Home Health Agencies Failed To Report Over Half of Falls With Major Injury and Hospitalization Among Their Medicare Patients, a 2023 report from the U.S Department of Health and Human Services’ Office of Inspector General.
- 6 tips for improving new coverage of older people, a tip sheet from The Journalist’s Resource.
- Crosswalk and pedestrian safety: What you need to know from recent research, from The Journalist’s Resource.
- Aging-in-place technology challenges and trends, a resource from the Association of Health Care Journalists.
- Successful aging at home: what reporters should know, a resource from the Association of Health Care Journalists.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
-
Easing Election Stress & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At the time of writing, the US is about to have a presidential election. Most of our readers are Americans, and in any case, what the US does tends to affect most of the world, so certainly many readers in other countries will be experiencing stress and anxiety about it too.
We’re a health science publication, not a political outlet, so we’ll refrain from commenting on any candidates or campaign policies, and we’d also like to be clear we are not urging you to any particular action politically—our focus today is simply about mental health.
First, CBT what can be CBT’d
Cognitive Behavioral Therapy (CBT) is far from a panacea, but it’s often a very good starting point. And when it seems the stakes are high, it’s easy to fall into such cognitive distortions as “crystal ball” and “catastrophization”, that is to say, predicting the future and feeling the impact of that (probably undesired version of the) future, and also feeling like it will be the end of the world.
Recognizing these processes and how they work, is the first step to managing our feelings about them.
Learn more: The Art of Being Unflappable (Tricks For Daily Life)
Next, DBT what can be DBT’d
A lot of CBT hinges on the assumption that our assumptions are incorrect. For example, that our friend does not secretly despise us, that our spouse is not about to leave us, that the symptoms we are experiencing are not cancer, and in this case, that the election outcome will not go badly, and if it does, the consequences will be less severe than imagined.
But… What if our concerns are, in fact, fully justified? Here’s where Dialectic Behavior Therapy (DBT) comes in, and with it, what therapists call “radical acceptance”.
In other words, we accept up front the idea that maybe it’s going to be terrible and that will truly suck, and then either:
- there’s nothing we can reasonably do about it now (so worrying just means you’ll suffer twice), or
- there is something we can reasonably do about it now (so we can go do that thing)
After doing the thing (if appropriate), defer processing the outcome of the election until after the election. There is no point in wasting energy to worry before then. In a broadly two-party system where things are usually close between those two largest parties, there’s something close to a 50% chance of an outcome that’s, at least, not the worst you feared.
Learn more: CBT, DBT, & Radical Acceptance
Lastly, empower yourself with Behavioral Activation (BA)
Whatever the outcome of any given election, the world will keep turning, and the individual battles about any given law or policy or such will continue to go on. That’s not to say an election won’t change things—it will—but there will always still be stuff to do on a grassroots level to make the world a better place, no matter what politician has been elected.
Being involved in doing things on a community level will not only help banish any feelings of despair (and if you got the election outcome you wanted, it’ll help you feel involved), but also, it can give you a sense of control, and can even form a part of the “ikigai” that is often talked about as one of the pillars of healthy longevity.
Learn more: What’s Your Ikigai?
And if you like videos, then enjoy this one (narrated by the ever soothing-voiced Alain de Botton):
Watch now: How To Escape From A Despairing Mood (4:46) ← it also has a text version if you prefer that
Take care!
Share This Post
Related Posts
-
What will aged care look like for the next generation? More of the same but higher out-of-pocket costs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged care financing is a vexed problem for the Australian government. It is already underfunded for the quality the community expects, and costs will increase dramatically. There are also significant concerns about the complexity of the system.
In 2021–22 the federal government spent A$25 billion on aged services for around 1.2 million people aged 65 and over. Around 60% went to residential care (190,000 people) and one-third to home care (one million people).
The final report from the government’s Aged Care Taskforce, which has been reviewing funding options, estimates the number of people who will need services is likely to grow to more than two million over the next 20 years. Costs are therefore likely to more than double.
The taskforce has considered what aged care services are reasonable and necessary and made recommendations to the government about how they can be paid for. This includes getting aged care users to pay for more of their care.
But rather than recommending an alternative financing arrangement that will safeguard Australians’ aged care services into the future, the taskforce largely recommends tidying up existing arrangements and keeping the status quo.
No Medicare-style levy
The taskforce rejected the aged care royal commission’s recommendation to introduce a levy to meet aged care cost increases. A 1% levy, similar to the Medicare levy, could have raised around $8 billion a year.
The taskforce failed to consider the mix of taxation, personal contributions and social insurance which are commonly used to fund aged care systems internationally. The Japanese system, for example, is financed by long-term insurance paid by those aged 40 and over, plus general taxation and a small copayment.
Instead, the taskforce puts forward a simple, pragmatic argument that older people are becoming wealthier through superannuation, there is a cost of living crisis for younger people and therefore older people should be required to pay more of their aged care costs.
Separating care from other services
In deciding what older people should pay more for, the taskforce divided services into care, everyday living and accommodation.
The taskforce thought the most important services were clinical services (including nursing and allied health) and these should be the main responsibility of government funding. Personal care, including showering and dressing were seen as a middle tier that is likely to attract some co-payment, despite these services often being necessary to maintain independence.
The task force recommended the costs for everyday living (such as food and utilities) and accommodation expenses (such as rent) should increasingly be a personal responsibility.
Aged care users will pay more of their share for cooking and cleaning.
Lizelle Lotter/ShutterstockMaking the system fairer
The taskforce thought it was unfair people in residential care were making substantial contributions for their everyday living expenses (about 25%) and those receiving home care weren’t (about 5%). This is, in part, because home care has always had a muddled set of rules about user co-payments.
But the taskforce provided no analysis of accommodation costs (such as utilities and maintenance) people meet at home compared with residential care.
To address the inefficiencies of upfront daily fees for packages, the taskforce recommends means testing co-payments for home care packages and basing them on the actual level of service users receive for everyday support (for food, cleaning, and so on) and to a lesser extent for support to maintain independence.
It is unclear whether clinical and personal care costs and user contributions will be treated the same for residential and home care.
Making residential aged care sustainable
The taskforce was concerned residential care operators were losing $4 per resident day on “hotel” (accommodation services) and everyday living costs.
The taskforce recommends means tested user contributions for room services and everyday living costs be increased.
It also recommends that wealthier older people be given more choice by allowing them to pay more (per resident day) for better amenities. This would allow providers to fully meet the cost of these services.
Effectively, this means daily living charges for residents are too low and inflexible and that fees would go up, although the taskforce was clear that low-income residents should be protected.
Moving from buying to renting rooms
Currently older people who need residential care have a choice of making a refundable up-front payment for their room or to pay rent to offset the loans providers take out to build facilities. Providers raise capital to build aged care facilities through equity or loan financing.
However, the taskforce did not consider the overall efficiency of the private capital market for financing aged care or alternative solutions.
Instead, it recommended capital contributions be streamlined and simplified by phasing out up-front payments and focusing on rental contributions. This echoes the royal commission, which found rent to be a more efficient and less risky method of financing capital for aged care in private capital markets.
It’s likely that in a decade or so, once the new home care arrangements are in place, there will be proportionally fewer older people in residential aged care. Those who do go are likely to be more disabled and have greater care needs. And those with more money will pay more for their accommodation and everyday living arrangements. But they may have more choice too.
Although the federal government has ruled out an aged care levy and changes to assets test on the family home, it has yet to respond to the majority of the recommendations. But given the aged care minister chaired the taskforce, it’s likely to provide a good indication of current thinking.
Hal Swerissen, Emeritus Professor, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cold Truth About Respiratory Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Pathogens That Came In From The Cold
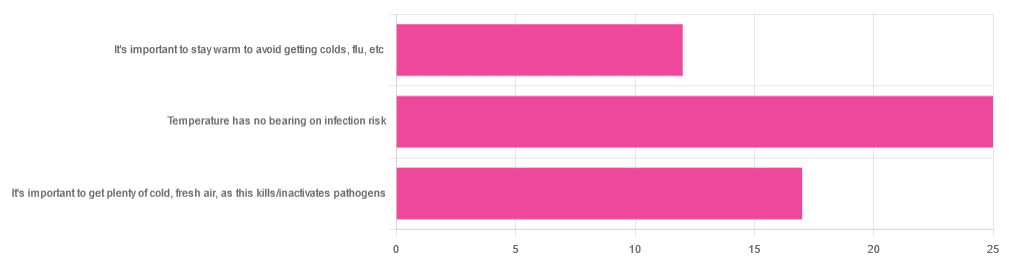
Yesterday, we asked you about your climate-themed policy for avoiding respiratory infections, and got the above-depicted, below-described, set of answers:
- About 46% of respondents said “Temperature has no bearing on infection risk”
- About 31% of respondents said “It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens”
- About 22% of respondents said “It’s important to stay warm to avoid getting colds, flu, etc”
Some gave rationales, including…
For “stay warm”:
❝Childhood lessons❞
For “get cold, fresh air”:
❝I just feel that it’s healthy to get fresh air daily. Whether it kills germs, I don’t know❞
For “temperature has no bearing”:
❝If climate issue affected respiratory infections, would people in the tropics suffer more than those in colder climates? Pollutants may affect respiratory infections, but I doubt just temperature would do so.❞
So, what does the science say?
It’s important to stay warm to avoid getting colds, flu, etc: True or False?
False, simply. Cold weather does increase the infection risk, but for reasons that a hat and scarf won’t protect you from. More on this later, but for now, let’s lay to rest the idea that bodily chilling will promote infection by cold, flu, etc.
In a small-ish but statistically significant study (n=180), it was found that…
❝There was no evidence that chilling caused any acute change in symptom scores❞
Read more: Acute cooling of the feet and the onset of common cold symptoms
Note: they do mention in their conclusion that chilling the feet “causes the onset of cold symptoms in about 10% of subjects who are chilled”, but the data does not support that conclusion, and the only clear indicator is that people who are more prone to colds generally, were more prone to getting a cold after a cold water footbath.
In other words, people who were more prone to colds remained more prone to colds, just the same.
It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens: True or False?
Broadly False, though most pathogens do have an optimal operating temperature that (for obvious reasons) is around normal human body temperature.
However, given that they don’t generally have to survive outside of a host body for long to get passed on, the fact that the pathogens may be a little sluggish in the great outdoors will not change the fact that they will be delighted by the climate in your respiratory tract as soon as you get back into the warm.
With regard to the cold air not being a reliable killer/inactivator of pathogens, we call to the witness stand…
Polar Bear Dies From Bird Flu As H5N1 Spreads Across Globe
(it was found near Utqiagvik, one of the northernmost communities in Alaska)
Because pathogens like human body temperature, raising the body temperature is a way to kill/inactivate them: True or False?
True! Unfortunately, it’s also a way to kill us. Because we, too, cannot survive for long above our normal body temperature.
So, for example, bundling up warmly and cranking up the heating won’t necessarily help, because:
- if the temperature is comfortable for you, it’s comfortable for the pathogen
- if the temperature is dangerous to the pathogen, it’s dangerous to you too
This is why the fever response evolved, and/but why many people with fevers die anyway. It’s the body’s way of playing chicken with the pathogen, challenging “guess which of us can survive this for longer!”
Temperature has no bearing on infection risk: True or False?
True and/or False, circumstantially. This one’s a little complex, but let’s break it down to the essentials.
- Temperature has no direct effect, for the reasons we outlined above
- Temperature is often related to humidity, which does have an effect
- Temperature does tend to influence human behavior (more time spent in open spaces with good ventilation vs more time spent in closed quarters with poor ventilation and/or recycled air), which has an obvious effect on transmission rates
The first one we covered, and the third one is self-evident, so let’s look at the second one:
Temperature is often related to humidity, which does have an effect
When the environmental temperature is warmer, water droplets in the air will tend to be bigger, and thus drop to the ground much more quickly.
When the environmental temperature is colder, water droplets in the air will tend to be smaller, and thus stay in the air for longer (along with any pathogens those water droplets may be carrying).
Some papers on the impact of this:
- Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections
- A Decrease in Temperature and Humidity Precedes Human Rhinovirus Infections in a Cold Climate
So whatever temperature you like to keep your environment, humidity is a protective factor against respiratory infections, and dry air is a risk factor.
So, for example:
- If the weather doesn’t suit having good ventilation, a humidifier is a good option
- Being in an airplane is one of the worst places to be for this, outside of a hospital
Don’t have a humidifier? Here’s an example product on Amazon, but by all means shop around.
A crock pot with hot water in and the lid off is also a very workable workaround too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Rebuild Your Cartilage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve covered before the topic of wear-and-tear on joints such as:
Avoiding/Managing Osteoarthritis
But what of cartilage, in particular? A common belief is “once it’s gone, it’s gone”, but that’s not quite right.
Cartilage is living tissue (metabolically active, with living cells). Within this tissue, specialist cells called chondrocytes produce extracellular cartilage matrix and collagen fibers, which provide smooth joint gliding as well as shock absorption.
Is exercise good or bad for cartilage?
Yes, yes it is. Exercise is good or bad for cartilage depending on the details:
- High-impact exercise e.g. running, jumping) places stress on cartilage, which is broadly bad
- However, impact loading strengthens the subchondral bone plate (layer under cartilage)
Strengthening this bone layer can help in long-term adaptation for high-impact sports.
See also: Resistance Is Useful! (Especially As We Get Older)
So, how to do that without wiping out your cartilage first?
Building up
A gradual process is what’s called-for here:
- Start with cyclic, non-impact moderate resistance exercises (e.g. cycling, rowing, swimming).
- Gradually add soft-impact loading (e.g. fast walking, soft jogging).
- Incorporate strength training to improve overall joint stability (e.g. leg press, for lower body joints)
- Slowly transition to running and jumping over a long period to allow tissues to adapt.
How exactly you go about that is a matter of personal taste, but here are some illustrative examples:
- Indoor* cycling
- Cross trainer
- Leg press machine
- Tennis
*Why indoor? It’s so that you can control the resistance level at the twist of a knob, and get on and off when you want.
See also: Treadmill vs Road ← for similar considerations when it comes to walking/running. Outdoor definitely has its advantages, but so does indoor!
And the very related: How To Do HIIT (Without Wrecking Your Body)
Note that HIIT is High Intensity Interval Training, not High Impact Interval Training!
Strength from the inside
One of the most important things for cartilage is collagen. You can supplement that, or if you’re vegetarian/vegan, you can take its constituent parts to improve your own synthesis of it.
See: Collagen For Your Skin, Joints, & Bones: We Are Such Stuff As Fish Are Made Of
Another supplement that can be helpful is glucosamine & chondroitin, which is best taken alongside a good omega-3 intake:
Want to know more?
This book is technically about (re)building strength and mobility in the case of arthritis specifically, but if your joints have more wear than you’d like, you may find this one an invaluable resource:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: