Drug Metabolism (When You’re Not Average!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Your Medications Run Out… Of You
Everybody knows that alcohol can affect medications’ effects, but what of smoking, and what of obesity? And how does the alcohol thing work anyway?
It’s all about the enzymes
Medicines that are processed by the liver (which is: most medicines) are metabolized there by specialist enzymes, and the things we do can increase or decrease the quantity of those enzymes—and/or how active they are.
Dr. Kata Wolff Pederson and her team of researchers at Aarhus University in Denmark examined the livers of recently deceased donors in ways that can’t (ethically) be done with live patients, and were able to find the associations between various lifestyle factors and different levels of enzymes responsible for drug metabolism.
And it’s not always how you might think!
Some key things they found:
- Smokers have twice as high levels of enzyme CYP1A2 than non-smokers, which results in the faster metabolism of a lot of drugs.
- Drinkers have 30% higher levels of enzyme CYP2E1, which also results in a faster metabolism of a lot of drugs.
- Patients with obesity have 50% lower levels of enzyme CYP3A4, resulting in slower metabolism of many drugs
This gets particularly relevant when we take into account the next fact:
- Of the individuals in the study, 40% died from poisoning from a mixture of drugs (usually: prescription and otherwise)
Read in full: Sex- and Lifestyle-Related Factors are Associated with Altered Hepatic CYP Protein Levels
Read a pop-sci article about it: Your lifestyle can determine how well your medicine will work
How much does the metabolism speed matter?
It can matter a lot! If you’re taking drugs and carefully abiding by the dosage instructions, those instructions were assuming they know your speed of metabolism, and this is based on an average.
- If your metabolism is faster, you can get too much of a drug too quickly, and it can harm you
- If your metabolism is faster, it also means that while yes it’ll start working sooner, it’ll also stop working sooner
- If it’s a painkiller, that’s inconvenient. If it’s a drug that keeps you alive, then well, that’s especially unfortunate.
- If your metabolism is slower, it can mean your body is still processing the previous dose(s) when you take the next one, and you can overdose (and potentially die)
We touched on this previously when we talked about obesity in health care settings, and how people can end up getting worse care:
As for alcohol and drugs? Obviously we do not recommend, but here’s some of the science of it with many examples:
Why it’s a bad idea to mix alcohol with some medications
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do We Simply Not Care About Old People?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The covid-19 pandemic would be a wake-up call for America, advocates for the elderly predicted: incontrovertible proof that the nation wasn’t doing enough to care for vulnerable older adults.
The death toll was shocking, as were reports of chaos in nursing homes and seniors suffering from isolation, depression, untreated illness, and neglect. Around 900,000 older adults have died of covid-19 to date, accounting for 3 of every 4 Americans who have perished in the pandemic.
But decisive actions that advocates had hoped for haven’t materialized. Today, most people — and government officials — appear to accept covid as a part of ordinary life. Many seniors at high risk aren’t getting antiviral therapies for covid, and most older adults in nursing homes aren’t getting updated vaccines. Efforts to strengthen care quality in nursing homes and assisted living centers have stalled amid debate over costs and the availability of staff. And only a small percentage of people are masking or taking other precautions in public despite a new wave of covid, flu, and respiratory syncytial virus infections hospitalizing and killing seniors.
In the last week of 2023 and the first two weeks of 2024 alone, 4,810 people 65 and older lost their lives to covid — a group that would fill more than 10 large airliners — according to data provided by the CDC. But the alarm that would attend plane crashes is notably absent. (During the same period, the flu killed an additional 1,201 seniors, and RSV killed 126.)
“It boggles my mind that there isn’t more outrage,” said Alice Bonner, 66, senior adviser for aging at the Institute for Healthcare Improvement. “I’m at the point where I want to say, ‘What the heck? Why aren’t people responding and doing more for older adults?’”
It’s a good question. Do we simply not care?
I put this big-picture question, which rarely gets asked amid debates over budgets and policies, to health care professionals, researchers, and policymakers who are older themselves and have spent many years working in the aging field. Here are some of their responses.
The pandemic made things worse. Prejudice against older adults is nothing new, but “it feels more intense, more hostile” now than previously, said Karl Pillemer, 69, a professor of psychology and gerontology at Cornell University.
“I think the pandemic helped reinforce images of older people as sick, frail, and isolated — as people who aren’t like the rest of us,” he said. “And human nature being what it is, we tend to like people who are similar to us and be less well disposed to ‘the others.’”
“A lot of us felt isolated and threatened during the pandemic. It made us sit there and think, ‘What I really care about is protecting myself, my wife, my brother, my kids, and screw everybody else,’” said W. Andrew Achenbaum, 76, the author of nine books on aging and a professor emeritus at Texas Medical Center in Houston.
In an environment of “us against them,” where everybody wants to blame somebody, Achenbaum continued, “who’s expendable? Older people who aren’t seen as productive, who consume resources believed to be in short supply. It’s really hard to give old people their due when you’re terrified about your own existence.”
Although covid continues to circulate, disproportionately affecting older adults, “people now think the crisis is over, and we have a deep desire to return to normal,” said Edwin Walker, 67, who leads the Administration on Aging at the Department of Health and Human Services. He spoke as an individual, not a government representative.
The upshot is “we didn’t learn the lessons we should have,” and the ageism that surfaced during the pandemic hasn’t abated, he observed.
Ageism is pervasive. “Everyone loves their own parents. But as a society, we don’t value older adults or the people who care for them,” said Robert Kramer, 74, co-founder and strategic adviser at the National Investment Center for Seniors Housing & Care.
Kramer thinks boomers are reaping what they have sown. “We have chased youth and glorified youth. When you spend billions of dollars trying to stay young, look young, act young, you build in an automatic fear and prejudice of the opposite.”
Combine the fear of diminishment, decline, and death that can accompany growing older with the trauma and fear that arose during the pandemic, and “I think covid has pushed us back in whatever progress we were making in addressing the needs of our rapidly aging society. It has further stigmatized aging,” said John Rowe, 79, professor of health policy and aging at Columbia University’s Mailman School of Public Health.
“The message to older adults is: ‘Your time has passed, give up your seat at the table, stop consuming resources, fall in line,’” said Anne Montgomery, 65, a health policy expert at the National Committee to Preserve Social Security and Medicare. She believes, however, that baby boomers can “rewrite and flip that script if we want to and if we work to change systems that embody the values of a deeply ageist society.”
Integration, not separation, is needed. The best way to overcome stigma is “to get to know the people you are stigmatizing,” said G. Allen Power, 70, a geriatrician and the chair in aging and dementia innovation at the Schlegel-University of Waterloo Research Institute for Aging in Canada. “But we separate ourselves from older people so we don’t have to think about our own aging and our own mortality.”
The solution: “We have to find ways to better integrate older adults in the community as opposed to moving them to campuses where they are apart from the rest of us,” Power said. “We need to stop seeing older people only through the lens of what services they might need and think instead of all they have to offer society.”
That point is a core precept of the National Academy of Medicine’s 2022 report Global Roadmap for Healthy Longevity. Older people are a “natural resource” who “make substantial contributions to their families and communities,” the report’s authors write in introducing their findings.
Those contributions include financial support to families, caregiving assistance, volunteering, and ongoing participation in the workforce, among other things.
“When older people thrive, all people thrive,” the report concludes.
Future generations will get their turn. That’s a message Kramer conveys in classes he teaches at the University of Southern California, Cornell, and other institutions. “You have far more at stake in changing the way we approach aging than I do,” he tells his students. “You are far more likely, statistically, to live past 100 than I am. If you don’t change society’s attitudes about aging, you will be condemned to lead the last third of your life in social, economic, and cultural irrelevance.”
As for himself and the baby boom generation, Kramer thinks it’s “too late” to effect the meaningful changes he hopes the future will bring.
“I suspect things for people in my generation could get a lot worse in the years ahead,” Pillemer said. “People are greatly underestimating what the cost of caring for the older population is going to be over the next 10 to 20 years, and I think that’s going to cause increased conflict.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
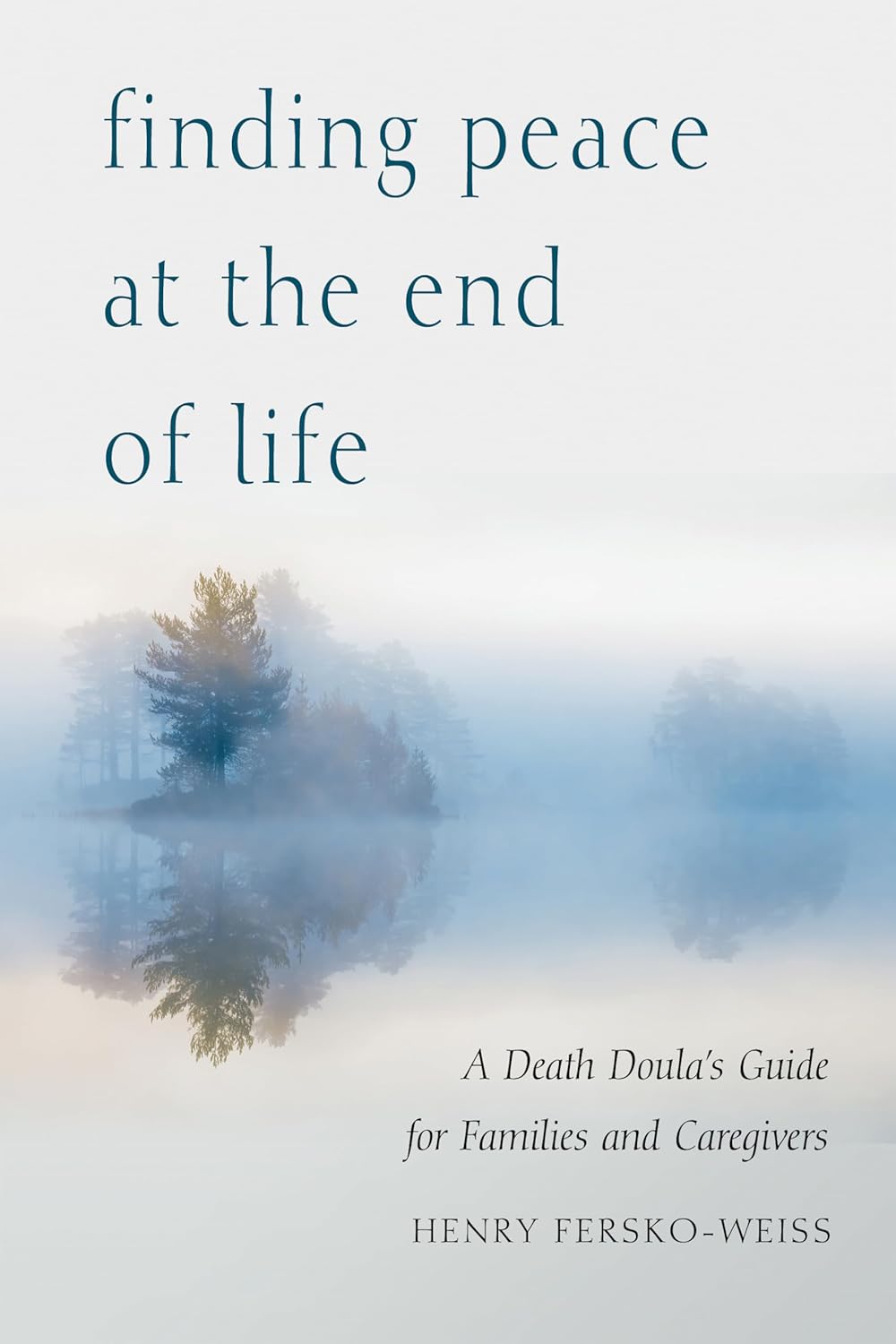
Finding Peace at the End of Life – by Henry Fersko-Weiss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not the most cheery book we’ve reviewed, but it is an important one. From its first chapter, with “a tale of two deaths”, one that went as well as can be reasonably expected, and the other one not so much, it presents a lot of choices.
The book is not prescriptive in its advice regarding how to deal with these choices, but rather, investigative. It’s thought-provoking, and asks questions—tacitly and overtly.
While the subtitle says “for families and caregivers”, it’s as much worth when it comes to managing one’s own mortality, too, by the way.
As for the scope of the book, it covers everything from terminal diagnosis, through the last part of life, to the death itself, to all that goes on shortly afterwards.
Stylewise, it’s… We’d call it “easy-reading” for style, but obviously the content is very heavy, so you might want to read it a bit at a time anyway, depending on how sensitive to such topics you are.
Bottom line: this book is not exactly a fun read, but it’s a very worthwhile one, and a good way to avoid regrets later.
Share This Post
-
Track Your Blood Sugars For Better Personalized Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There Will Be Blood
Are you counting steps? Counting calories? Monitoring your sleep? Heart rate zones? These all have their merits:
- Steps: One More Resource Against Osteoporosis!
- Calories: Is Cutting Calories The Key To Healthy Long Life?
- Sleep: A Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
- Heart Rate Zones: Heart Rate Zones, Oxalates, & More
About calories: this writer (it’s me, hi) opines that intermittent fasting has the same benefits as caloric restriction, without the hassle of counting, and is therefore superior. I also personally find fasting psychologically more pleasant. However, our goal here is to be informative, not prescriptive, and some people may have reasons to prefer CR to IF!
Examples that come to mind include ease of adherence in the case of diabetes management, especially Type 1, or if one’s schedule (and/or one’s “medications that need to be taken with food” schedule) does not suit IF.
And now for the blood…
A rising trend in health enthusiasts presently is the use of Continuous Glucose Monitors (CGMs), which do exactly what is sounds like they do: they continually monitor glucose. Specifically, the amount of it in your blood.
Of course, these have been in use in diabetes management for years; the technology is not new, but the application of the technology is.
A good example of what benefits a non-diabetic person can gain from the use of a CGM is Jessie Inchauspé, the food scientist of “Glucose Revolution” and “The Glucose Goddess Method” fame.
By wearing a CGM, she was able to notice what things did and didn’t spike her blood sugars, and found that a lot of the things were not stuff that people knew/advised about!
For example, much of diabetes management (including avoiding diabetes in the first place) is based around paying attention to carbs and little else, but she found that it made a huge difference what she ate (or didn’t) with the carbs. By taking many notes over the course of her daily life, she was eventually able to isolate these patterns, showed her working-out in The Glucose Revolution (there’s a lot of science in that book), and distilled that information into bite-size (heh) advice such as:
10 Ways To Balance Blood Sugars
That’s great, but since people like Inchauspé have done the work, I don’t have to, right?
You indeed don’t have to! But you can still benefit from it. For example, fastidious as her work was, it’s a sample size of one. If you’re not a slim white 32-year-old French woman, there may be some factors that are different for you.
All this to say: glucose responses, much like nutrition in general, are not a one-size-fits-all affair.
With a CGM, you can start building up your own picture of what your responses to various foods are like, rather than merely what they “should” be like.
This, by the way, is also one of the main aims of personalized health company ZOE, which crowdsourced a lot of scientific data about personalized metabolic responses to standardized meals:
Not knowing these things can be dangerous
We don’t like to scaremonger here, but we do like to point out potential dangers, and in this case, blindly following standardized diet advice, if your physiology is not standard, can have harmful effects, see for example:
Diabetic-level glucose spikes seen in non-diabetic people
Where can I get a CGM?
We don’t sell them, and neither does Amazon, but you can check out some options here:
The 4 Best CGM Devices For Measuring Blood Sugar in 2024
…and if your doctor is not obliging with a prescription, note that the device that came out top in the above comparisons, will be available OTC soon:
The First OTC Continuous Glucose Monitor Will Be Available Summer 2024
Take care!
Share This Post
Related Posts
-
Psychedelics and Psychotherapy – Edited by Dr. Tim Read & Maria Papaspyrou
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note on authorship, first: this book is edited by the psychiatrist and psychotherapist credited above, but after the introductory section, the rest of the chapters are written by experts on the individual topics.As such, the style will vary somewhat, from chapter to chapter.
What this book isn’t: “try drugs and feel better!”
Rather, the book explores the various ways in which assorted drugs can help people to—even if just briefly—shed things they didn’t know they were carrying, or otherwise couldn’t put down, and access parts of themselves they otherwise couldn’t.
We also get to read a lot about the different roles the facilitator can play in guiding the therapeutic process, and what can be expected out of each kind of experience. This varies a lot from one drug to another, so it makes for very worthwhile reading, if that’s something you might consider pursuing. Knowledge makes for much more informed choices!
Bottom line: if you’re curious about the therapeutic potential of psychedelics, and want a reference that’s more personal than dry clinical studies, but still more “safe and removed” than diving in by yourself, this is the book for you.
Click here to check out Psychedelics and Psychotherapy, and expand your understanding!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High Histamine Foods To Avoid (And Low Histamine Foods To Eat Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nour Zibdeh is an Integrative and Functional Dietician, and she helps people overcome food intolerances. Today, it’s about getting rid of the underdiagnosed condition that is histamine intolerance, by first eliminating the triggers, and then not getting stuck on the low-histamine diet
The recommendations
High histamine foods to avoid include:
- Alcohol (all types)
- Fermented foods—normally great for the gut, but bad in this case
- That includes most cheeses and yogurts
- Aged, cured, or otherwise preserved meat
- Some plants, e.g. tomato, spinach, eggplant, banana, avocado. Again, normally all great, but not in this case.
Low histamine foods to eat include:
- Fruits and vegetables not mentioned above
- Minimally processed meat and fish, either fresh from the butcher/fishmonger, or frozen (not from the chilled food section of the supermarket), and eaten the same day they were purchased or defrosted, because otherwise histamine builds up over time (and quite quickly)
- Grains, but she recommends skipping gluten, given the high likelihood of a comorbid gluten intolerance. So instead she recommends for example quinoa, oats, rice, buckwheat, millet, etc.
For more about these (and more examples), as well as how to then phase safely off the low histamine diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Food intolerances often gang up on a person (i.e., comorbidity is high), so you might also like to read about:
- Gluten: What’s The Truth?
- Fiber For FODMAP-Avoiders
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Crohn’s, Food Intolerances, & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Flax Seeds vs Pumpkin Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing flax seeds to pumpkin seeds, we picked the flax.
Why?
Looking at the macros first, they are equal on protein, and flax seeds have a lot more fiber while pumpkin seeds have a lot more carbs. We’re going to prioritise fiber over carbs and call this a win for flax.
In terms of vitamins, flax seeds have a lot more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while pumpkin seeds have a tiny bit more vitamin A. An easy win for flax here.
When it comes to minerals, flax has multiples more calcium, copper, iron, magnesium, manganese, phosphorus, and selenium, while pumpkin seeds have more zinc. Another win for flax.
Adding up the sections makes for a clear overall win for flax, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score? ← seeds count as plants!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: