Debunking the vitamin D fad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout the pandemic, many unproven miracle COVID-19 “cures” emerged, and vitamin D claims have been one of the most persistent. This is not new for the vitamin. It’s been touted in recent decades as a way to “boost” the immune system, improve overall health, prevent a host of diseases, and allegedly even substitute for vaccines.
But as with many internet-popular health “remedies,” the reality is far less flashy and far more nuanced.
What is vitamin D, and why is it important?
Vitamin D is a nutrient that helps the body absorb calcium, which is essential for bone health. In the sunlight, your skin naturally produces vitamin D that is then stored in fat cells until it is used.
The skin pigment melanin absorbs the UV rays necessary for vitamin D production, meaning that more highly pigmented or darker skin produces less vitamin D than lighter skin with the same amount of sun exposure. Thus, people with darker skin are at higher risk of vitamin D deficiency.
Most of our vitamin D comes from the sun. An additional 10 percent to 20 percent of our vitamin D comes from foods like fatty fish (such as salmon), eggs, and mushrooms. Vitamin D supplements are another source of the nutrient for people who are unable to get enough from sun exposure and diet.
Vitamin D deficiency is real, but there’s no epidemic
Some people who promote vitamin D supplements claim that vitamin D deficiency is an epidemic causing widespread health issues. There is little evidence to support this claim. A 2022 analysis of 2001-2018 data found that 2.6 percent of people in the U.S. had severe vitamin D deficiency.
Severe vitamin D deficiency can cause serious health issues, such as muscle weakness, bone loss in adults, and rickets (weak bones) in children. Some people are at higher risk for the deficiency, including individuals with certain disorders that prevent the body from absorbing or processing vitamin D or those with a family history of vitamin D deficiency.
Black Americans have the highest rates of severe vitamin D deficiency at nearly 12 percent. Severe vitamin D deficiency is also slightly higher in the U.S. during the winter when people get less sun exposure. Rates of moderate vitamin D deficiency are higher at 22 percent overall and are highest among Black Americans (49 percent) and Mexican Americans (35 percent).
Although severe vitamin D deficiency exists in the U.S., it is far from common. Most tellingly, conditions that are directly linked to vitamin D deficiency are not widespread. There is no epidemic of rickets, for example, or bone loss in adults.
There’s little evidence that vitamin D supplements improve overall health
Vitamin D supplements have clear, proven positive effects for people with vitamin D deficiency. Other health benefits of vitamin D supplements are less certain.
There is some evidence that the supplement may reduce the risk of fracture in adults with osteoporosis, a condition that causes weak, fragile bones. However, the benefit appears to be limited to people who have low vitamin D levels. In adults with normal vitamin D levels, supplements have no effect on fracture risk.
The largest randomized controlled trial of vitamin D, called VITAL, investigated the effects of vitamin D supplementation in people without an existing deficiency. The study found that vitamin D supplements had no effects on the risk of cancer, diabetes, or cardiovascular disease, including heart attack and stroke. The study concluded that more research is necessary to determine who may benefit from vitamin D supplements.
Independent analyses found that vitamin D supplementation may be associated with a long-term decrease in cancer mortality, but results are mixed and also require more investigation.
A 2021 analysis of past vitamin D trials found no overall health benefits from vitamin D supplements in people with normal vitamin D levels. Most large-scale studies have found no link between vitamin D supplements and lower all-cause mortality (deaths from any cause), except in older adults and those with vitamin D deficiency.
Vitamin D provides modest protection against respiratory infections
Vitamin D is important for immune function, but this is often misconstrued as vitamin D “boosting” the immune system.
Some people falsely believe that taking vitamin D supplements will keep them healthy and prevent infections like the flu or COVID-19. In reality, clinical trials and large-scale studies of vitamin D have found only minimal protective effects against respiratory infections.
A 2021 analysis of 46 trials found that 61.3 percent of participants who took daily vitamin D supplements got respiratory infections during the study periods—compared to 62.3 percent of people who did not take the supplements. A 2024 meta-analysis of 43 trials found no overall protective effect against respiratory infections, but it detected a slight decrease in risk among people who took specific doses daily.
In young children, there is some evidence that vitamin D supplementation may reduce the length of respiratory infections. However, it does not affect the number or severity of infections that children have.
Despite claims that taking vitamin D can protect against COVID-19, two clinical trials found that taking daily vitamin D supplements did not reduce the risk or severity of COVID-19 infections, even at high doses.
Context is key when considering vitamin D’s benefits
None of these studies contradict the well-established evidence that people with vitamin D deficiency benefit from vitamin D supplements. But it’s important to remember that many of the most popular health claims about vitamin D’s benefits are based on research in people with vitamin D deficiency.
Research in vitamin D-deficient populations is important, but it tells us little about how vitamin D will affect people with normal or close to normal vitamin D levels. A closer look at vitamin D research in people without low levels reveals little evidence to support the idea that the general population benefits from taking vitamin D supplements.
For more information, or to learn about your vitamin D levels, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Make Your Coffee Heart-Healthier!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health-Hack Your Coffee
We have previously written about the general health considerations (benefits and potential problems) of coffee:
The Bitter Truth About Coffee (or is it?)
Today, we will broadly assume that you are drinking coffee (in general, not necessarily right now, though if you are, same!) and would like to continue to do so. We also assume you’d like to do so as healthily as possible.
Not all coffees are created equal
If you order a coffee in France or Italy without specifying what kind, the coffee you receive will be short, dark,
and handsomeand without sugar. Healthwise, this is not a bad starting point. However…- It will usually be espresso
- Or it may be what in N. America is called a French press (in Europe it’s just called a cafetière)
Both of these kinds of coffee mean that cafestol, a compound found in the oily part of coffee and which is known to raise LDL (“bad” cholesterol”), stays in the drink.
Read: Cafestol and Kahweol: A Review on Their Bioactivities and Pharmacological Properties
Also: Cafestol extraction yield from different coffee brew mechanisms
If you’re reading that second one and wondering what a mocha pot or a Turkish coffee is, they are these things:
- Mocha pot: a stovetop device used for making espresso without an espresso machine
- Turkish coffee pot: also a stovetop device; this thing makes some of the strongest coffee you have ever encountered. Turks usually add sugar (this writer doesn’t; but my taste in coffee been described as “coffee like a punch in the face”)
So, wonderful as they are for those of us who love strong coffee, they also produce the highest in-drink levels of cafestol. If you’d like to cut the cafestol (for example, if you are keeping an eye on your LDL), we recommend…
The humble filter coffee
Whether by your favorite filter coffee machine or a pour-over low-tech coffee setup of the kind you could use even without an electricity supply, the filter keeps more than just the coffee grinds out; it keeps the cafestol out too; most of it, anyway, depending on what kind of filter you use, and the grind of the coffee:
Physical characteristics of the paper filter and low cafestol content filter coffee brews
What about instant coffee?
It has very little cafestol in it. It’s up to you whether that’s sufficient reason to choose it over any other form of coffee (this coffee-lover could never)
Want to make any coffee healthier?
This one isn’t about the cafestol, but…
If you take l-theanine (see here for our previous main feature about l-theanine), the l-theanine acts as a moderator and modulator of the caffeine, amongst other benefits:
The Cognitive-Enhancing Outcomes of Caffeine and L-theanine: A Systematic Review
As to where to get that, we don’t sell it, but here’s an example product on Amazon
Enjoy!
Share This Post
-
The Bare-Bones Truth About Osteoporosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
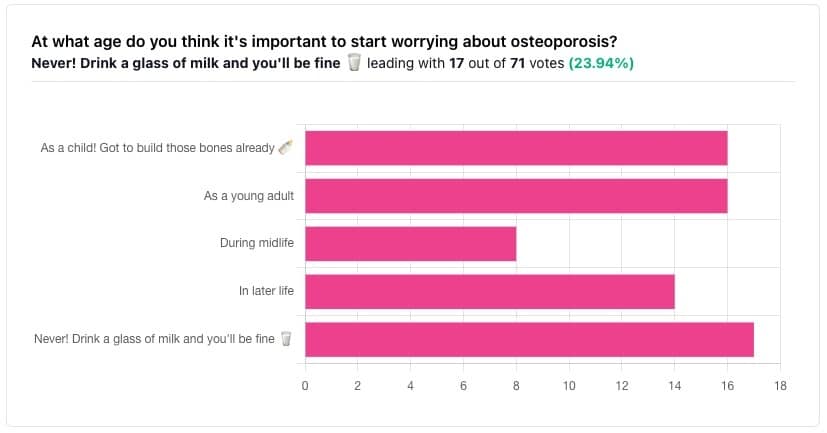
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
The Bare-bones Truth About Osteoporosis
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
At first glance it may seem shocking that a majority of respondents to a poll in a health-focused newsletter think it’ll never be an issue worth worrying about, but in fact this is partly a statistical quirk, because the vote of the strongest “early prevention” crowd was divided between “as a child” and “as a young adult”.
This poll also gave you the option to add a comment with your vote. Many subscribers chose to do so, explaining your choices… But, interestingly, not one single person who voted for “never” had any additional thoughts to add.
We loved reading your replies, by the way, and wish we had room to include them here, because they were very interesting and thought-provoking.
Let’s get to the myths and facts:
Top myth: “you will never need to worry about it; drink a glass of milk and you’ll be fine!”
The body is constantly repairing itself. Its ability to do that declines with age. Until about 35 on average, we can replace bone mineral as quickly as it is lost. After that, we lose it by up to 1% per year, and that rate climbs after 50, and climbs even more steeply for those who go through (untreated) menopause.
Losing 1% per year might not seem like a lot, but if you want to live to 100, there are some unfortunate implications!
About that menopause, by the way… Because declining estrogen levels late in life contribute significantly to osteoporosis, hormone replacement therapy (HRT) may be of value to many for the sake of bone health, never mind the more obvious and commonly-sought benefits.
On the topic of that glass of milk…
- Milk is a great source of calcium, which is useless to the body if you don’t also have good levels of vitamin D and magnesium.
- People’s vitamin D levels tend to directly correlate to the level of sun where they live, if supplementation isn’t undertaken.
- Plant-based milks are usually fortified with vitamin D (and calcium), by the way.
- Most people are deficient in magnesium, because green leafy things don’t form as big a part of most people’s diets as they should.
See also: An update on magnesium and bone health
Next most common myth: “bone health is all about calcium”
We spoke a little above about the importance of vitamin D and magnesium for being able to properly use that. But potassium is also critical:
Read more: The effects of potassium on bone health
While we’re on the topic…
People think of collagen as being for skin health. And it is important for that, but collagen’s benefits (and the negative effects of its absence) go much deeper, to include bone health. We’ve written about this before, so rather than take more space today, we’ll just drop the link:
We Are Such Stuff As Fish Are Made Of
Want to really maximize your bone health?
You might want to check out this well-sourced LiveStrong article:
Bone Health: Best and Worst Foods
(Teaser: leafy greens are in 2nd place, topped by sardines at #1—where do you think milk ranks?)
Share This Post
-
Cannabis Myths vs Reality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cannabis Myths vs Reality
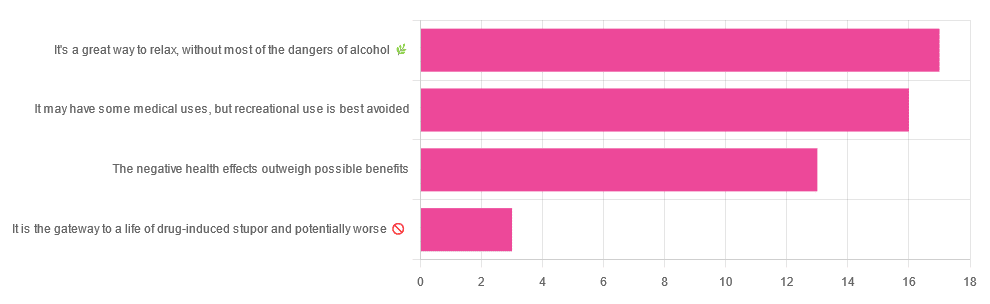
We asked you for your (health-related) opinion on cannabis use—specifically, the kind with psychoactive THC, not just CBD. We got the above-pictured, below-described, spread of responses:
- A little over a third of you voted for “It’s a great way to relax, without most of the dangers of alcohol”.
- A little under a third of you voted for “It may have some medical uses, but recreational use is best avoided”.
- About a quarter of you voted for “The negative health effects outweigh the possible benefits”
- Three of you voted for “It is the gateway to a life of drug-induced stupor and potentially worse”
So, what does the science say?
A quick legal note first: we’re a health science publication, and are writing from that perspective. We do not know your location, much less your local laws and regulations, and so cannot comment on such. Please check your own local laws and regulations in that regard.
Cannabis use can cause serious health problems: True or False?
True. Whether the risks outweigh the benefits is a personal and subjective matter (for example, a person using it to mitigate the pain of late stage cancer is probably unconcerned with many other potential risks), but what’s objectively true is that it can cause serious health problems.
One subscriber who voted for “The negative health effects outweigh the possible benefits” wrote:
❝At a bare minimum, you are ingesting SMOKE into your lungs!! Everyone SEEMS TO BE against smoking cigarettes, but cannabis smoking is OK?? Lung cancer comes in many forms.❞
Of course, that is assuming smoking cannabis, and not consuming it as an edible. But, what does the science say on smoking it, and lung cancer?
There’s a lot less research about this when it comes to cannabis, compared to tobacco. But, there is some:
❝Results from our pooled analyses provide little evidence for an increased risk of lung cancer among habitual or long-term cannabis smokers, although the possibility of potential adverse effect for heavy consumption cannot be excluded.❞
Read: Cannabis smoking and lung cancer risk: Pooled analysis in the International Lung Cancer Consortium
Another study agreed there appears to be no association with lung cancer, but that there are other lung diseases to consider, such as bronchitis and COPD:
❝Smoking cannabis is associated with symptoms of chronic bronchitis, and there may be a modest association with the development of chronic obstructive pulmonary disease. Current evidence does not suggest an association with lung cancer.❞
Read: Cannabis Use, Lung Cancer, and Related Issues
Cannabis edibles are much safer than smoking cannabis: True or False?
Broadly True, with an important caveat.
One subscriber who selected “It may have some medical uses, but recreational use is best avoided”, wrote:
❝I’ve been taking cannabis gummies for fibromyalgia. I don’t know if they’re helping but they’re not doing any harm. You cannot overdose you don’t become addicted.❞
Firstly, of course consuming edibles (rather than inhaling cannabis) eliminates the smoke-related risk factors we discussed above. However, other risks remain, including the much greater ease of accidentally overdosing.
❝Visits attributable to inhaled cannabis are more frequent than those attributable to edible cannabis, although the latter is associated with more acute psychiatric visits and more ED visits than expected.❞
Note: that “more frequent” for inhaled cannabis, is because more people inhale it than eat it. If we adjust the numbers to control for how much less often people eat it, suddenly we see that the numbers of hospital admissions are disproportionately high for edibles, compared to inhaled cannabis.
Or, as the study author put it:
❝There are more adverse drug events associated on a milligram per milligram basis of THC when it comes in form of edibles versus an inhaled cannabis. If 1,000 people smoked pot and 1,000 people at the same dose in an edible, then more people would have more adverse drug events from edible cannabis.❞
See the numbers: Acute Illness Associated With Cannabis Use, by Route of Exposure
Why does this happen?
- It’s often because edibles take longer to take effect, so someone thinks “this isn’t very strong” and has more.
- It’s also sometimes because someone errantly eats someone else’s edibles, not realising what they are.
- It’s sometimes a combination of the above problems: a person who is now high, may simply forget and/or make a bad decision when it comes to eating more.
On the other hand, that doesn’t mean inhaling it is necessarily safer. As well as the pulmonary issues we discussed previously, inhaling cannabis has a higher risk of cannabinoid hyperemesis syndrome (and the resultant cyclic vomiting that’s difficult to treat).
You can read about this fascinating condition that’s sometimes informally called “scromiting”, a portmanteau of screaming and vomiting:
Cannabinoid Hyperemesis Syndrome
You can’t get addicted to cannabis: True or False?
False. However, it is fair to say that the likelihood of developing a substance abuse disorder is lower than for alcohol, and much lower than for nicotine.
See: Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013
If you prefer just the stats without the science, here’s the CDC’s rendering of that:
Addiction (Marijuana or Cannabis Use Disorder)
However, there is an interesting complicating factor, which is age. One is 4–7 times more likely to develop a substance abuse disorder, if one starts use as an adolescent, rather than later in life:
Cannabis is the gateway to use of more dangerous drugs: True or False?
False, generally speaking. Of course, for any population there will be some outliers, but there appears to be no meaningful causal relation between cannabis use and other substance use:
Interestingly, the strongest association (where any existed at all) was between cannabis use and opioid use. However, rather than this being a matter of cannabis use being a gateway to opioid use, it seems more likely that this is a matter of people looking to both for the same purpose: pain relief.
As a result, growing accessibility of cannabis may actually reduce opioid problems:
- Cannabis as a Gateway Drug for Opioid Use Disorder
- Association between medical cannabis laws and opioid overdose mortality has reversed over time
Some final words…
Cannabis is a complex drug with complex mechanisms and complex health considerations, and research is mostly quite young, due to its historic illegality seriously cramping science by reducing sample sizes to negligible. Simply put, there’s a lot we still don’t know.
Also, we covered some important topics today, but there were others we didn’t have time to cover, such as the other potential psychological benefits—and risks. Likely we’ll revisit those another day.
Lastly, while we’ve covered a bunch of risks today, those of you who said it has fewer and lesser risks than alcohol are quite right—the only reason we couldn’t focus on that more, is because to talk about all the risks of alcohol would make this feature many times longer!
Meanwhile, whether you partake or not, stay safe and stay well.
Share This Post
Related Posts
-
Mung Beans vs Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to black beans, we picked the black beans.
Why?
Both are great! But…
In terms of macros, black beans have more protein, carbs, and fiber, as well as the lower glycemic index (although both are already low). So, a clear win for black beans here.
In the category of vitamins, mung beans have more of vitamins A, B5, B9, and C, while black beans have more of vitamins B1, B6, E, K, and choline. Thus, a slight win for black beans this time.
When it comes to minerals, mung beans have more selenium and zinc, while black beans have more calcium, copper, iron, magnesium, manganese, phosphorus, and potassium. An easy win for black beans.
Of course, enjoy either or both—but if you’re going to pick one, we say black beans win the day.
Want to learn more?
You might like to read:
Plant vs Animal Protein: Head-to-Head
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to carrot, we picked the carrot.
Why?
In terms of macros, carrot has more protein, carbs, and fiber, and is thus the “most food per food” option. The carb:fiber ratio is such that they have about the same glycemic index (when raw, anyway).
In the category of vitamins, celery has more of vitamins B9 and K, while carrot has more of vitamins A, B1, B2, B3, B5, B6, C, E, and choline. An easy win for carrot here.
When it comes to minerals, celery has more calcium and selenium, while carrot has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Another clear win for carrot.
In short, both are very respectable foods, but carrot simply has more in it, and it’s all good.
Enjoy!
Want to learn more?
You might like to read:
Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Insomnia Breakthrough – by Katherine Coleman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a massage therapist, knows plenty about relaxation. But how to put that to use when it comes to getting good quality sleep?
She takes a holistic approach, and yes, does start by covering all the things you’d expect to find in any guide to better sleep (aim for regular schedule, have darkness when you sleep, cool room, clean sheets, no alcohol or caffeine before bed, etc).
What she offers in particular beyond that, is the integration of calming routines, building in mindfulness for sleep (when very often people will go for the opposite!), and small cumulative lifestyle adjustments that are conducive to getting a better night’s rest every night.
The style is very light pop-science (as one might expect from someone who is not, in fact, a scientist), and while we do get a bibliography at the back, it’s a meagre 4 pages. Nevertheless, there’s a lot of interdisciplinary knowledge here, explained well.
Bottom line: if improving your sleep is something you’d like to do, this book can almost certainly get you on the right track.
Click here to check out The Insomnia Breakthrough, and don’t stay up too late reading it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: