The Bitter Truth About Coffee (or is it?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Bitter Truth About Coffee (or is it?)
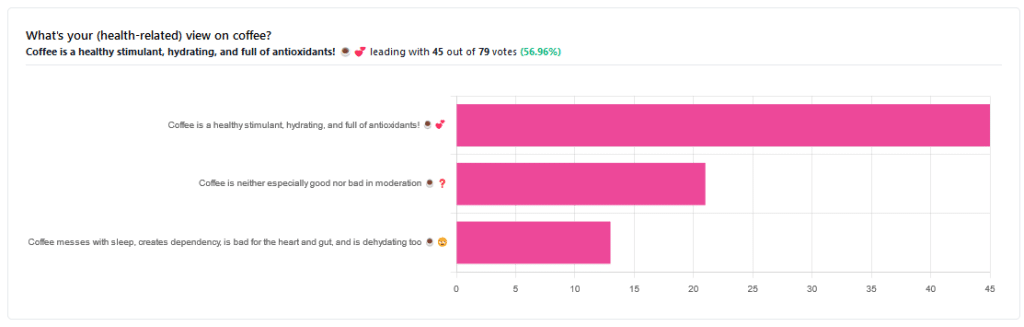
Yesterday, we asked you for your (health-related) views on coffee. The results were clear: if we assume the responses to be representative, we’re a large group of coffee-enthusiasts!
One subscriber who voted for “Coffee is a healthy stimulant, hydrating, and full of antioxidants” wrote:
❝Not so sure about how hydrating it is! Like most food and drink, moderation is key. More than 2 or 3 cups make me buzz! Just too much.❞
And that fine point brings us to our first potential myth:
Coffee is dehydrating: True or False?
False. With caveats…
Coffee, in whatever form we drink it, is wet. This may not come as a startling revelation, but it’s an important starting point. It’s mostly water. Water itself is not dehydrating.
Caffeine, however, is a diuretic—meaning you will tend to pee more. It achieves its diuretic effect by increasing blood flow to your kidneys, which prompts them to release more water through urination.
See: Effect of caffeine on bladder function in patients with overactive bladder symptoms
How much caffeine is required to have a diuretic effect? About 4.5 mg/kg.
What this means in practical terms: if you weigh 70kg (a little over 150lbs), 4.5×70 gives us 315.
315mg is about how much caffeine might be in six shots of espresso. We say “might” because while dosage calculations are an exact science, the actual amount in your shot of espresso can vary depending on many factors, including:
- The kind of coffee bean
- How and when it was roasted
- How and when it was ground
- The water used to make the espresso
- The pressure and temperature of the water
…and that’s all without looking at the most obvious factor: “is the coffee decaffeinated?”
If it doesn’t contain caffeine, it’s not diuretic. Decaffeinated coffee does usually contain tiny amounts of caffeine still, but with nearer 3mg than 300mg, it’s orders of magnitude away from having a diuretic effect.
If it does contain caffeine, then the next question becomes: “and how much water?”
For example, an Americano (espresso, with hot water added to make it a long drink) will be more hydrating than a ristretto (espresso, stopped halfway through pushing, meaning it is shorter and stronger than a normal espresso).
A subscriber who voted for “Coffee messes with sleep, creates dependency, is bad for the heart and gut, and is dehydrating too” wrote:
❝Coffee causes tachycardia for me so staying away is best. People with colon cancer are urged to stay away from coffee completely.❞
These are great points! It brings us to our next potential myth:
Coffee is bad for the heart: True or False?
False… For most people.
Some people, like our subscriber above, have an adverse reaction to caffeine, such as tachycardia. An important reason (beyond basic decency) for anyone providing coffee to honor requests for decaff.
For most people, caffeine is “heart neutral”. It doesn’t provide direct benefits or cause direct harm, provided it is enjoyed in moderation.
See also: Can you overdose on caffeine?
Some quick extra notes…
That’s all we have time for in myth-busting, but it’s worth noting before we close that coffee has a lot of health benefits; we didn’t cover them today because they’re not contentious, but they are interesting nevertheless:
- Coffee is the world’s biggest source of antioxidants
- 65% reduced risk of Alzheimer’s for coffee-drinkers
- 67% reduced risk of type 2 diabetes for coffee-drinkers
- 43% reduced risk of liver cancer for coffee-drinkers
- 53% reduced suicide risk for coffee-drinkers
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
MSG vs. Salt: Sodium Comparison
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Is MSG healthier than salt in terms of sodium content or is it the same or worse?
Great question, and for that matter, MSG itself is a great topic for another day. But your actual question, we can readily answer here and now:
- Firstly, by “salt” we’re assuming from context that you mean sodium chloride.
- Both salt and MSG do contain sodium. However…
- MSG contains only about a third of the sodium that salt does, gram-for-gram.
- It’s still wise to be mindful of it, though. Same with sodium in other ingredients!
- Baking soda contains about twice as much sodium, gram for gram, as MSG.
Wondering why this happens?
Salt (sodium chloride, NaCl) is equal parts sodium and chlorine, by atom count, but sodium’s atomic mass is lower than chlorine’s, so 100g of salt contains only 39.34g of sodium.
Baking soda (sodium bicarbonate, NaHCO₃) is one part sodium for one part hydrogen, one part carbon, and three parts oxygen. Taking each of their diverse atomic masses into account, we see that 100g of baking soda contains 27.4g sodium.
MSG (monosodium glutamate, C₅H₈NO₄Na) is only one part sodium for 5 parts carbon, 8 parts hydrogen, 1 part nitrogen, and 4 parts oxygen… And all those other atoms put together weigh a lot (comparatively), so 100g of MSG contains only 12.28g sodium.
Share This Post
-
Fix Your Upper Back With These Three Steps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to back pain, the lower back gets a lot of attention, but what about when it’s nearer the neck and shoulders?
Reaching for better health
In this short video, Liv describes and shows three exercises:
Exercise 1: Thoracic Pullover (Dumbbell Pullover)
Purpose: Improves overhead reach and shoulder mobility.
Equipment: light weight, yoga block, or foam roller.
Steps:- Lie on the floor with the foam roller/block beneath the upper back.
- Hold the weight in both hands, arms extended upward.
- Inhale deeply and reach the weight toward the ceiling.
- Exhale and arc your spine over the block, moving the weight backward.
- Keep core tension to maintain a neutral lower back position.
- Perform 10 repetitions.
Exercise 2: Rotational Mobility Stretch
Purpose: enhances torso rotation, core strength, and hip mobility.
Equipment: none (or a mat)
Steps:- Lie on your side with knees stacked at 90° and arms extended in front.
- Hold a weight in the top hand.
- Inhale and lift the top arm toward the ceiling, extending the shoulder blade.
- Exhale and twist your torso, allowing the arm to move toward the floor.
- Modify by extending the bottom leg for a deeper twist if needed.
- Perform 6 reps per side, switching legs and repeating on the other side.
Exercise 3: Doorway/Pole Side Stretch
Purpose: targets multiple areas for a deep, satisfying stretch.
Equipment: door frame, pole, or wall.
Steps:- Stand at arm’s length from the wall or frame.
- Cross the outer leg (furthest from the wall) behind the inner leg.
- Place the closest hand on the wall and reach the other arm overhead.
- Grip the wall or frame with the top hand, pressing away with the bottom hand.
- Lean into a banana-shaped curve and rotate your chest upward for a deeper stretch.
- Hold for 20–30 seconds per side and repeat 2–3 times.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Share This Post
-
Tilapia vs Cod – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tilapia to cod, we picked the tilapia.
Why?
Another case of “that which is more expensive is not necessarily the healthier”!
In terms of macros, tilapia has more protein and fats, as well as more omega-3 (and omega-6). On the downside, tilapia does have relatively more saturated fat, but at 0.94g/100g, it’s not exactly butter.
The vitamins category sees that tilapia has more of vitamins B1, B3, B5, B12, D, and K, while cod has more of vitamins B6, B9, and choline. A moderate win for tilapia.
When it comes to minerals, things are most divided; tilapia has more copper, iron, phosphorus, potassium, manganese, and selenium, while cod has more magnesium and zinc. An easy win for tilapia.
One other thing to note is that both of these fish contain mercury these days (and it’s worth noting: cod has nearly 10x more mercury). Mercury is, of course, not exactly a health food.
So, excessive consumption of either is not recommended, but out of the two, tilapia is definitely the one to pick.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Know The Health Differences
Take care!
Share This Post
Related Posts
-
Ageless – by Dr. Andrew Steele
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, yet another book with “The new science of…” in the title; does this one deliver new science?
Actually, yes, this time! The author was originally a physicist before deciding that aging was the number one problem that needed solving, and switched tracks to computational biology, and pioneered a lot of research, some of the fruits of which can be found in this book, in amongst a more general history of the (very young!) field of biogerontology.
Downside: most of this is not very practical for the lay reader; most of it is explanations of how things happen on a cellular and/or genetic level, and how we learned that. A lot also pertains to what we can learn from animals that either age very slowly, or are biologically immortal (in other words, they can still be killed, but they don’t age and won’t die of anything age-related), or are immune to cancer—and how we might borrow those genes for gene therapy.
However, there are also chapters on such things as “running repairs”, “reprogramming aging”, and “how to live long enough to live even longer”.
The style is conversational pop science; in the prose, he simply states things without reference, but at the back, there are 40 pages of bibliography, indexed in the order in which they occurred and prefaced with the statement that he’s referencing in each case. It’s an odd way to do citations, but it works comfortably enough.
Bottom line: if you’d like to understand aging on the cellular level, and how we know what we know and what the likely future possibilities are, then this is a great book; it’s also simply very enjoyable to read, assuming you have an interest in the topic (as this reviewer does).
Click here to check out Ageless, and understand the science of getting older without getting old!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Honey vs Maple Syrup – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honey to maple syrup, we picked the honey.
Why?
It was very close, as both have small advantages:
• Honey has some medicinal properties (and depending on type, may contain an antihistamine)
• Maple syrup is a good source of manganese, as well as low-but-present amounts of other mineralsHowever, you wouldn’t want to eat enough maple syrup to rely on it as a source of those minerals, and honey has the lower GI (average 46 vs 54; for comparison, refined sugar is 65), which works well as a tie-breaker.
(If GI’s very important to you, though, the easy winner here would be agave syrup if we let it compete, with its GI of 15)
Read more:
• Can Honey Relieve Allergies?
• From Apples to Bees, and High-Fructose C’sDon’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
90% Of People Skip This Essential Exercise—Are You One Of Them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Single-leg strengthening is essential for joint health at any age (unless you want to bunny-hop up and down the stairs with both feet at once, for example), yet many people overlook it. This neglect often leads to pain, stiffness, and a higher risk of injury.
Dr. Alyssa Kuhn, arthritis specialist, explains how to do it:
On the rise
In this video, different exercise variations—beginner, intermediate, and advanced—are presented to help you build strength at your own pace:
Beginner: start by using a chair, adding a cushion for support if needed. Sit at the edge and position one foot slightly in front of the other in a staggered stance. Stand up and sit down in a controlled manner, allowing the back leg to bear more weight and work harder than the front leg. Do 8–10 repetitions per side and pay attention to whether one side feels weaker. To build strength, incorporate this movement into daily activities, such as standing up from the couch. Master this variation before progressing, to avoid knee injury.
Intermediate: to make the exercise more challenging, you can either use a lower chair, or extend your front foot further out, shifting more weight to your back leg. Only modify one variable at a time to maintain control. Do 8–10 repetitions per side, ensuring proper form. A common mistake is allowing the back knee to move inward, which can cause knee stress. To prevent this, use a mirror to check your form and keep the knee and ankle aligned during movement.
Advanced: when you’re ready, extend your front leg completely with the heel on the ground and toes up, removing its stability and forcing the back leg to work even harder. Maintain controlled movement while keeping your knee and ankle aligned. Repeat the exercise on both sides, focusing extra effort on the weaker leg to build balanced strength.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: