Dealing With Back Acne
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Lately I’ve increasingly been getting zits on my back, I don’t think my shower habits have changed at all, is this just an age thing or is there something I can do about it?❞
Well, we cannot diagnose from afar, so definitely consider seeing a dermatologist if it persists and/or it’s more than a small nuisance to you, but…
Yes and no, with regard to age.
Rather, it’s not really about age, but (in most cases, anyway) hormonal fluctuations. That’s why teenagers often get it; it’s also why acne breakouts can occur during pregnancy, and it can happen again in perimenopause, menopause, or in the postmenopause climb-down, due to imbalanced hormones during the change, and while it’s less likely for men undergoing the andropause (the noticeable drop of testosterone levels after a certain age), it can absolutely occur if taking certain androgenic supplements, including simply taking testosterone (or conversely, if taking something to dial down antagonistic hormones). It can also happen if you’re taking something that throws out your free testosterone to DHT ratio.
As for what to do in this case? The usual process is: just wait it out. At some point your hormones will become stable again (nature loves equilibrium, and the body is mostly a self-righting system if given what it needs to do that), and your skin will return to normal. To be clear: the acne occurs because of the change, not necessarily the end place. So whatever hormone levels you have, be they medicated or otherwise, you just need to keep them stable now (assuming the levels are fine; if not, get them fine, and then keep them stable—speak to an endocrinologist for that) in order to come out the other side acne-free.
However, that’s “the usual process”, and obviously we cannot guarantee it’s not something else. It can also be caused by stress:
The Impact of Pyschological Stress on Acne ← teehee, a typo made it into the publication title
…in which case, of course, simply manage your stress (we know, often easier said than done, but the point is, that’s the remedy in this case).
See also: How To Reduce Chronic Stress
Diet is not the cause (or cure), but enjoying an anti-inflammatory diet will be beneficial, and consuming inflammatory things, exacerbatory:
Effects of Diet on Acne and Its Response to Treatment
Hygiene is also rarely to blame, but it can make a difference, so: do wash gently, wear clean clothes, and wash your bedsheets more often than you think necessary. And about that showering:
Body Scrubs: Benefits, Risks, and Guidance
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat To Beat Hyperthyroidism!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Would love to see more on eating vegan. I am allergic to soy in any form which seems to be in everything❞
There is a lot of it about, isn’t there? Happily, these days, a lot of meat and dairy alternatives are also made from other sources, for example pea protein is getting used a lot more nowadays in meat substitutes, and there are many kinds of alternatives to dairy (e.g. nut milks, oat milk, hemp milk, and—which is a branding nightmare but very healthy—pea milk).
You might like these previous main features of ours:
- Do We Need Animal Products To Be Healthy?
- The Whys and Hows of Cutting Down Meat Consumption
- Plant-Based Milks—What’s Best?
Also, if doing a whole foods plant-based diet, lentils (especially brown lentils) can be used as a great substitute for minced beef/lamb in recipes that call for such.
Boil the lentils (a liter of water to a cup of lentils is great; use a rice cooker if you have one!) along with the seasonings you will use (herbs appropriate to your dish, and then: black pepper is always good; you shouldn’t need to add salt; a teaspoon of low-sodium yeast extract is great though, or to really get the best nutritional benefits, nooch).
When it is done, you shouldn’t have excess water now, so just use as is, or if you want a slightly fatty kick, fry briefly in a little extra virgin olive oil, before using it however you were planning to use it.
Enjoy!
❝What foods should I eat for hyperthyroidism? My doctor tells me what foods to avoid, but not what to eat❞
Great question! We’ll have to do a main feature on hyperthyroidism one of these days, as so far we’ve only done features on hypothyroidism:
As for hyperthyroidism…
Depending on your medications, your doctor might recommend a low iodine diet. If so, then you might want to check out:
American Thyroid Association | Low Iodine Diet Plan
…for recommendations.
But in a way, that’s still a manner of “what to avoid” (iodine) and then the foods to eat to avoid that.
You may be wondering: is there any food that actively helps against hyperthyroidism, as opposed to merely does not cause problems?
And the answer is: yes!
Cruciferous vegetables (e.g. cabbage, sprouts, broccoli, cauliflower, etc) contain goitrin, which in immoderate quantities can cause problems for people with hypothyroidism because it can reduce thyroid hormone synthesis. If you have hyperthyroidism, however, this can work in your favor.
Read more: The role of micronutrients in thyroid dysfunction
The above paper focuses on children, but it was the paper we found that explains it most clearly while showing good science. However, the same holds true for adults:
Notwithstanding that the title comes from the angle of examining hypothyroidism, the mechanism of action makes clear its beneficence in the case of hyperthyroidism.
Selenium is also a great nutrient in the case of autoimmune hyperthyroidism, because it is needed to metabolize thyroid hormone (if you don’t metabolize it, it’ll just build up):
Selenium and Thyroid Disease: From Pathophysiology to Treatment
The absolute top best dietary source of selenium is Brazil nuts, to the point that people without hyperthyroidism have to take care to not eat more than a few per day (because too much selenium could then cause problems):
NIH | Selenium Fact Sheet for Health Professionals
(this contains information on the recommended amount, the upper limit amount, how much is in Brazil nuts and other foods, and what happens if you get too much or too little)
Note: after Brazil nuts (which are about 5 times more rich in selenium than the next highest source), the other “good” sources of selenium—mostly various kinds of fish—are also “good” source of iodine, so you might want to skip those.
Want more ideas?
You might like this from LivHealth:
Hyperthyroidism Diet: 9 Foods To Ease Symptoms
Enjoy!
Share This Post
-
No, sugar doesn’t make your kids hyperactive
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a Saturday afternoon at a kids’ birthday party. Hordes of children are swarming between the spread of birthday treats and party games. Half-eaten cupcakes, biscuits and lollies litter the floor, and the kids seem to have gained superhuman speed and bounce-off-the-wall energy. But is sugar to blame?
The belief that eating sugary foods and drinks leads to hyperactivity has steadfastly persisted for decades. And parents have curtailed their children’s intake accordingly.
Balanced nutrition is critical during childhood. As a neuroscientist who has studied the negative effects of high sugar “junk food” diets on brain function, I can confidently say excessive sugar consumption does not have benefits to the young mind. In fact, neuroimaging studies show the brains of children who eat more processed snack foods are smaller in volume, particularly in the frontal cortices, than those of children who eat a more healthful diet.
But today’s scientific evidence does not support the claim sugar makes kids hyperactive.
Sharomka/Shutterstock The hyperactivity myth
Sugar is a rapid source of fuel for the body. The myth of sugar-induced hyperactivity can be traced to a handful of studies conducted in the 1970s and early 1980s. These were focused on the Feingold Diet as a treatment for what we now call Attention Deficit Hyperactivity Disorder (ADHD), a neurodivergent profile where problems with inattention and/or hyperactivity and impulsivity can negatively affect school, work or relationships.
Devised by American paediatric allergist Benjamin Feingold, the diet is extremely restrictive. Artificial colours, sweeteners (including sugar) and flavourings, salicylates including aspirin, and three preservatives (butylated hydroxyanisole, butylated hydroxytoluene, and tert-Butrylhdryquinone) are eliminated.
Salicylates occur naturally in many healthy foods, including apples, berries, tomatoes, broccoli, cucumbers, capsicums, nuts, seeds, spices and some grains. So, as well as eliminating processed foods containing artificial colours, flavours, preservatives and sweeteners, the Feingold diet eliminates many nutritious foods helpful for healthy development.
However, Feingold believed avoiding these ingredients improved focus and behaviour. He conducted some small studies, which he claimed showed a large proportion of hyperactive children responded favourably to his diet.
Even it doesn’t make kids hyperactive, they shouldn’t have too much sugar. DenisMArt/Shutterstock Flawed by design
The methods used in the studies were flawed, particularly with respect to adequate control groups (who did not restrict foods) and failed to establish a causal link between sugar consumption and hyperactive behaviour.
Subsequent studies suggested less than 2% responded to restrictions rather than Feingold’s claimed 75%. But the idea still took hold in the public consciousness and was perpetuated by anecdotal experiences.
Fast forward to the present day. The scientific landscape looks vastly different. Rigorous research conducted by experts has consistently failed to find a connection between sugar and hyperactivity. Numerous placebo-controlled studies have demonstrated sugar does not significantly impact children’s behaviour or attention span.
One landmark meta-analysis study, published almost 20 years ago, compared the effects of sugar versus a placebo on children’s behaviour across multiple studies. The results were clear: in the vast majority of studies, sugar consumption did not lead to increased hyperactivity or disruptive behaviour.
Subsequent research has reinforced these findings, providing further evidence sugar does not cause hyperactivity in children, even in those diagnosed with ADHD.
While Feingold’s original claims were overstated, a small proportion of children do experience allergies to artificial food flavourings and dyes.
Pre-school aged children may be more sensitive to food additives than older children. This is potentially due to their smaller body size, or their still-developing brain and body.
Hooked on dopamine?
Although the link between sugar and hyperactivity is murky at best, there is a proven link between the neurotransmitter dopamine and increased activity.
The brain releases dopamine when a reward is encountered – such as an unexpected sweet treat. A surge of dopamine also invigorates movement – we see this increased activity after taking psychostimulant drugs like amphetamine. The excited behaviour of children towards sugary foods may be attributed to a burst of dopamine released in expectation of a reward, although the level of dopamine release is much less than that of a psychostimulant drug.
Dopamine function is also critically linked to ADHD, which is thought to be due to diminished dopamine receptor function in the brain. Some ADHD treatments such as methylphenidate (labelled Ritalin or Concerta) and lisdexamfetamine (sold as Vyvanse) are also psychostimulants. But in the ADHD brain the increased dopamine from these drugs recalibrates brain function to aid focus and behavioural control.
Maybe it’s less of a sugar rush and more of a dopamine rush? Anastasiya Tsiasemnikava/Shutterstock Why does the myth persist?
The complex interplay between diet, behaviour and societal beliefs endures. Expecting sugar to change your child’s behaviour can influence how you interpret what you see. In a study where parents were told their child had either received a sugary drink, or a placebo drink (with a non-sugar sweetener), those parents who expected their child to be hyperactive after having sugar perceived this effect, even when they’d only had the sugar-free placebo.
The allure of a simple explanation – blaming sugar for hyperactivity – can also be appealing in a world filled with many choices and conflicting voices.
Healthy foods, healthy brains
Sugar itself may not make your child hyperactive, but it can affect your child’s mental and physical health. Rather than demonising sugar, we should encourage moderation and balanced nutrition, teaching children healthy eating habits and fostering a positive relationship with food.
In both children and adults, the World Health Organization (WHO) recommends limiting free sugar consumption to less than 10% of energy intake, and a reduction to 5% for further health benefits. Free sugars include sugars added to foods during manufacturing, and naturally present sugars in honey, syrups, fruit juices and fruit juice concentrates.
Treating sugary foods as rewards can result in them becoming highly valued by children. Non-sugar rewards also have this effect, so it’s a good idea to use stickers, toys or a fun activity as incentives for positive behaviour instead.
While sugar may provide a temporary energy boost, it does not turn children into hyperactive whirlwinds.
Amy Reichelt, Senior Lecturer (Adjunct), Nutritional neuroscientist, University of Adelaide
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Sweet Spot for Brain Health – by Dr. Sui Wong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we often mention that “what’s good for the heart is good for the brain”, but at least in part, it’s because (as this book makes very clear), “what’s good for the blood is good for the brain”. After all, our brain uses about 25% of our energy, and that energy is delivered there by the blood. And if it doesn’t get enough nutrients, oxygen, etc, and detritus isn’t taken away, then problems happen.
Dr. Wong discusses Alzheimer’s as heavily driven by metabolic problems such as diabetes and even pre-diabetes, and sets out to put in our hands the guidebook to not only not doing that, but also, actually making sure our brain gets proper nourishment without delivering that as intermittent sugar spikes because we opted for a something with very fast-acting carbs to perk us up energetically.
More than most books on the topic, she talks a lot about the neurobiology of glucose metabolism, so that’s something that really sets this book apart from many of its genre.
The style is narrative, explaining the body’s processes in a clear fashion, without skimping on science. There are definitely words that your average layperson might not know, but they’re explained as we go, and there are frequent recaps of what we learned previously, making for ultimately easy reading.
After all the information is given, there’s also a guided “12-week challenge” with a theme-of-the-week for each week, to integrate a new lifestyle adjustment each week in a progressive fashion so that without needing to drastically change many things at once, we get where we need to be in terms of healthy habits.
Bottom line: if you’d like to do right by your brain and while you’re at it say goodbye to blood sugar highs and lows, then this book is an excellent guide for that.
Click here to check out Sweet Spot For Brain Health, and enjoy a consistently-energized brain!
Share This Post
Related Posts
-
Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chiropractors have been banned again from manipulating babies’ spines. Here’s what the evidence actually says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chiropractors in Australia will not be able to perform spinal manipulation on children under the age of two once more, following health concerns from doctors and politicians.
But what is the spinal treatment at the centre of the controversy? Does it work? Is there evidence of harm?
We’re a team of researchers who specialise in evidence-based musculoskeletal health. I (Matt) am a registered chiropractor, Joshua is a registered physiotherapist and Giovanni trained as a physiotherapist.
Here’s what the evidence says.
Dmitry Naumov/Shutterstock Remind me, how did this all come about?
A Melbourne-based chiropractor posted a video on social media in 2018 using a spring-loaded device (known as the Activator) to manipulate the spine of a two-week-old baby suspended upside down by the ankles.
The video sparked widespread concerns among the public, medical associations and politicians. It prompted a ban on the procedure in young children. The Victorian health minister commissioned Safer Care Victoria to conduct an independent review of spinal manipulation techniques on children.
Recently, the Chiropractic Board of Australia reinstated chiropractors’ authorisation to perform spinal manipulation on babies under two years old. But this week, it backflipped, following heavy criticism from medical associations and politicians.
What is spinal manipulation?
Spinal manipulation is a treatment used by chiropractors and other health professionals such as doctors, osteopaths and physiotherapists.
It is an umbrella term that includes popular “back cracking” techniques.
It also includes more gentle forms of treatment, such as massage or joint mobilisations. These involve applying pressure to joints without generating a “cracking” sound.
Does spinal manipulation in babies work?
Several international guidelines for health-care professionals recommend spinal manipulation to treat adults with conditions such as back pain and headache as there is an abundance of evidence on the topic. For example, spinal manipulation for back pain is supported by data from nearly 10,000 adults.
For children, it’s a different story. Safer Care Victoria’s 2019 review of spinal manipulation found very few studies testing whether this treatment was safe and effective in children.
Studies were generally small and were of poor quality. Some of those small, poor-quality studies, suggest spinal manipulation provides a very small benefit for back pain, colic and potentially bedwetting – some common reasons for parents to take their child to see a chiropractor. But overall, the review found the overall body of evidence was very poor.
Spinal manipulation doesn’t seem to help young children with an ear infection. MIA Studio/Shutterstock However, for most other children’s conditions chiropractors treat – such as headache, asthma, otitis media (a type of ear infection), cerebral palsy, hyperactivity and torticollis (“twisted neck”) – there did not appear to be a benefit.
The number of studies investigating the effectiveness of spinal manipulation on babies under two years of age was even smaller.
There was one high-quality study and two small, poor quality studies. These did not show an appreciable benefit of spinal manipulation on colic, otitis media with effusion (known as glue ear) or twisted neck in babies.
Is spinal manipulation on babies safe?
In terms of safety, most studies in the review found serious complications were extremely rare. The review noted one baby or child dying (a report from Germany in 2001 after spinal manipulation by a physiotherapist). The most common complications were mild in nature such as increased crying and soreness.
However, because studies were very small, they cannot tell us anything about the safety of spinal manipulation in a reliable way. Studies that are designed to properly investigate if a treatment is safe typically include thousands of patients. And these studies have not yet been done.
Why do people see chiropractors?
Safer Care Victoria also conducted surveys with more than 20,000 people living in Australia who had taken their children under 12 years old to a chiropractor in the past ten years.
Nearly three-quarters said that was for treatment of a child aged two years or younger.
Nearly all people surveyed reported a positive experience when they took their child to a chiropractor and reported that their child’s condition improved with chiropractic care. Only a small number of people (0.3%) reported a negative experience, and this was mostly related to cost of treatment, lack of improvement in their child’s condition, excessive use of x-rays, and perceived pressure to avoid medications.
Many of the respondents had also consulted their GP or maternity/child health nurse.
What now for spinal manipulation in children?
At the request of state and federal ministers, the Chiropractic Board of Australia confirmed that spinal manipulation on babies under two years old will continue to be banned until it discusses the issue further with health ministers.
Many chiropractors believe this is unfair, especially considering the strong consumer support for chiropractic care outlined in the Safer Care Victoria report, and the rarity of serious reported harms in children.
Others believe that in the absence of evidence of benefit and uncertainty around whether spinal manipulation is safe in children and babies, the precautionary principle should apply and children and babies should not receive spinal manipulation.
Ultimately, high quality research is urgently needed to better understand whether spinal manipulation is beneficial for the range of conditions chiropractors provide it for, and whether the benefit outweighs the extremely small chance of a serious complication.
This will help parents make an informed choice about health care for their child.
Matt Fernandez, Senior lecturer and researcher in chiropractic, CQUniversity Australia; Giovanni E. Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney, and Joshua Zadro, NHMRC Emerging Leader Research Fellow, Sydney Musculoskeletal Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
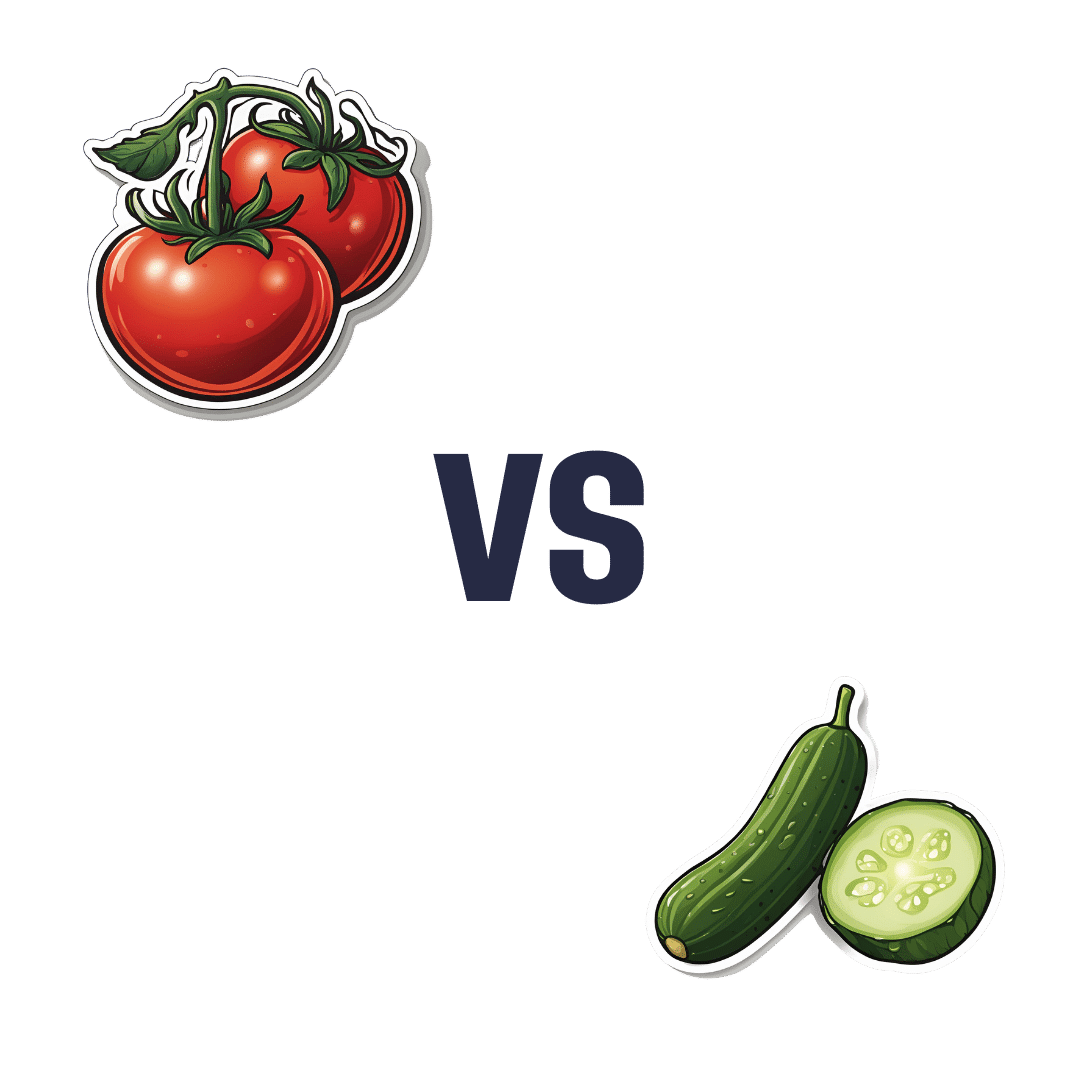
Tomato vs Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tomato to cucumber, we picked the tomato.
Why?
Both are certainly great, but there are some nutritional factors between them:
In terms of macros, everything is approximately equal except that tomato has more than 2x the fiber, so that’s a win for tomato.
When it comes to vitamins, tomatoes have more of vitamins A, B1, B3, B6, B9, C, E, and choline, while cucumber has more of vitamins B2, B5, and K. In short, an 8:3 victory for tomatoes.
In the category of minerals, tomatoes have more copper, potassium, and manganese, while cucumber has more calcium, iron, magnesium, selenium, and zinc. So, a win for cucumber this time.
Both have useful phytochemical properties, too; tomatoes are rich in lycopene which has many benefits, and cucumbers have powerful anti-inflammatory powers whose mechanism of action is not yet fully understood—see the links below for more details!
All in all, enjoy either or both (they make a great salad chopped roughly together with some olives, a little garlic, and a drizzle of olive oil and balsamic vinegar with a twist or three of black pepper), but if you have to pick just one (what a cruel world), we say the tomato has the most benefits, on balance.
Want to learn more?
You might like to read:
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: