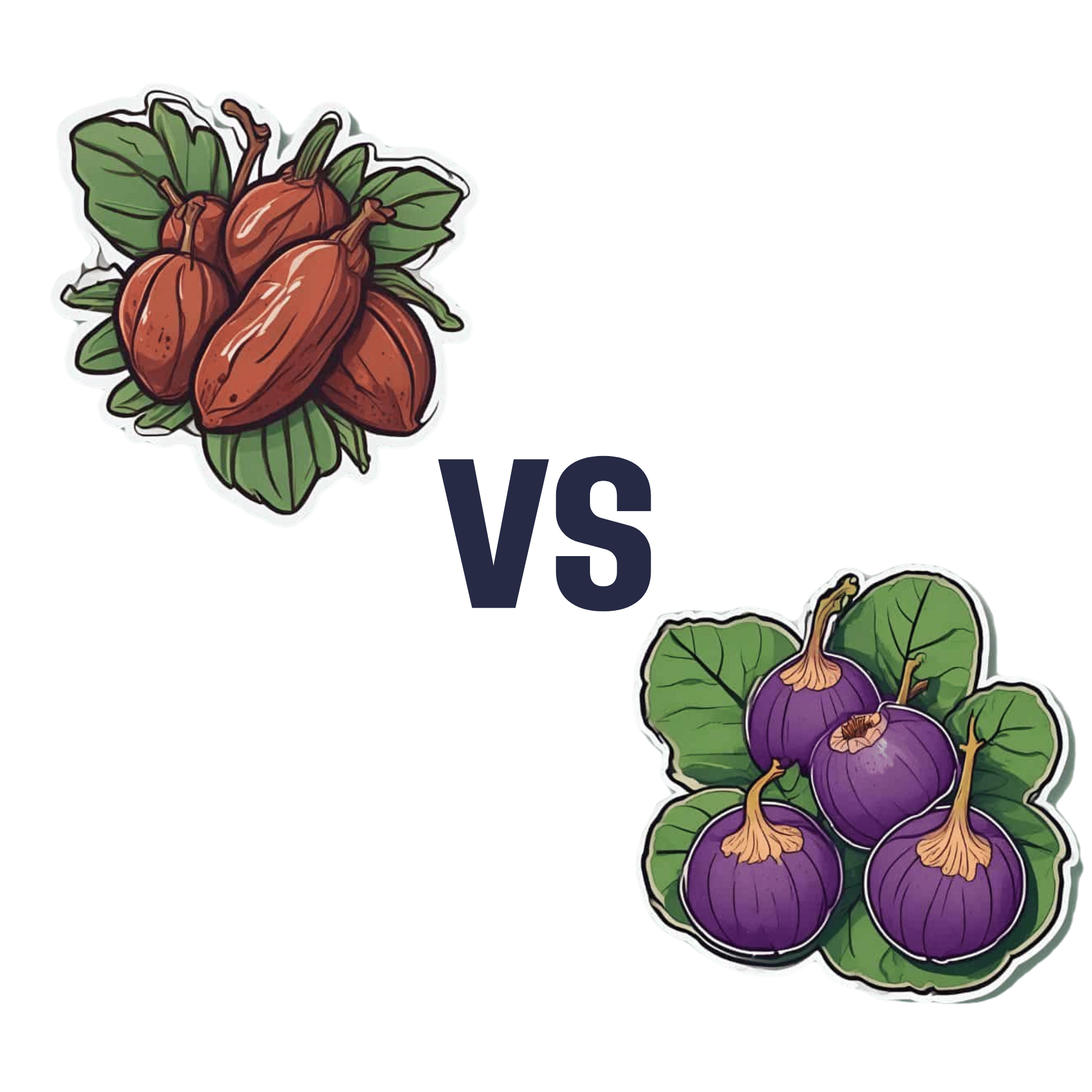
Dates vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to figs, we picked the dates.
Why?
Dates are higher in sugar, but also have a lower glycemic index than figs, which makes the sugar content much healthier. On the flipside, figs do have around 3x more fiber.
So far, so balanced.
When it comes to micronutrients though, dates take the prize much more clearly.
Dates have slightly more of most vitamins, and a lot more of most minerals.
In particular, dates are several times higher in copper, iron, magnesium, manganese, phosphorus, selenium, and zinc.
As for other phytochemical benefits going on:
- both are good against diabetes for reasons beyond the macros
- both have anti-inflammatory properties
- dates have anticancer properties
- dates have kidney-protecting properties
So in this last case, another win for dates.
Both are still great though, so do enjoy both!
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carbonated Water: For Weight Loss, Satiety, Or Just Gas?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are two main mechanisms of action by which sparkling water is considered to help satiety and/or weight loss; they are:
- It “fills us up” such that we feel fuller sooner, and thus eat less, and thus (all other things being equal) perhaps lose weight
- The carbon dioxide is absorbed into the bloodstream, where (as a matter of chemistry) it improves glucose metabolism, thus lowering blood sugars and indirectly leading (potentially) to weight loss, but even if not, lowered blood sugars are good for most people most of the time, right?
However, there are just a few problems:
Full of gas?
Many people self-report enjoying sparkling water as a way to feel fuller while fasting (or even while eating). However, the plural of “anecdote” is not “data”, so, here be data… Ish:
❝In order to determine whether such satiating effects occur through oral carbonic stimulation alone, we conducted modified sham-feeding (SF) tests (carbonated water ingestion (CW), water ingestion (W), carbonated water sham-feeding (CW-SF), and water sham-feeding (W-SF)), employing an equivalent volume and standardized temperature of carbonated and plain water, in a randomized crossover design.
Thirteen young women began fasting at 10 p.m. on the previous night and were loaded with each sample (15ºC, 250 mL) at 9 a.m. on separate days. Electrogastrography (EGG) recordings were obtained from 20 min before to 45 min after the loading to determine the power and frequency of the gastric myoelectrical activity. Appetite was assessed using visual analog scales. After ingestion, significantly increased fullness and decreased hunger ratings were observed in the CW group. After the load, transiently but significantly increased fullness as well as decreased hunger ratings were observed in the CW-SF group. The powers of normogastria (2-4 cpm) and tachygastria (4-9 cpm) showed significant increases in the CW and W groups, but not in the CW-SF and W-SF groups. The peak frequency of normogastria tended to shift toward a higher band in the CW group, whereas it shifted toward a lower band in the CW-SF group, indicating a different EGG rhythm.
Our results suggest that CO2-induced oral stimulation is solely responsible for the feeling of satiety.❞
~ Dr. Maki Suzuki et al.
Now, that’s self-reported, and a sample size of 13, so it’s not the most airtight science ever, but it is at least science. Here’s the paper, by the way:
Oral Carbonation Attenuates Feeling of Hunger and Gastric Myoelectrical Activity in Young Women
Here’s another small study with 8 people, which found that still and sparkling water had the exact same effect:
Effect of carbonated water on gastric emptying and intragastric meal distribution
However, drinking water (still or sparkling) with a meal will not have anywhere near the same effect for satiety as consuming food that has a high water-content.
See also: Some Surprising Truths About Hunger And Satiety ← our main feature in which we examine the science of volumetrics, including a study that shows how water incorporated into a food (but not served with a food) decreases caloric intake.
As an aside, one difference that carbonation can make is to increase ghrelin levels—that’s the hunger hormone (the satiety hormone is leptin, by the way). This one’s a rat study, but it seems reasonable that the same will be true of humans:
…which is worth bearing in mind even if you yourself are not, in fact, a male rat.
The glucose guzzler?
This one has simply been the case of a study being misrepresented, for example here:
Fizzy water might aid weight loss by providing a small boost to glucose uptake and metabolism
The idea is that higher levels of carbon dioxide in the blood mean faster glucose metabolism, which is technically true. Now, often “technically true” is the best kind of true, but not here, because it’s simply not useful.
In short, we produce so much carbon dioxide as part of our normal respiratory processes, that any carbon dioxide we might consume in a carbonated water is barely a blip in the graph.
Oh, and that article we just linked? Even within the article, despite running with that headline, the actual scientists quoted are saying such things as:
❝While there is a hypothetical link between carbonated water and glucose metabolism, this has yet to be tested in well-designed human intervention studies❞
~ Professor Sumantra Ray
Note: the word “hypothetical” means “one level lower than theoretical”. This is very far from being a conclusion.
And the study itself? Wasn’t even about carbonated water, it was about kidney dialysis and how the carbon dioxide content can result in hypoglycemia:
The mechanism of hypoglycemia caused by hemodialysis
…which got referenced in this paper (not a study):
Can carbonated water support weight loss?
…and even that concluded:
❝CO2 in carbonated water may promote weight loss by enhancing glucose uptake and metabolism in red blood cells.
However, the amount is so small that it is difficult to expect weight loss effects solely from the CO2 in carbonated water.
Drinking carbonated water may also affect blood glucose measurements.❞
Note: the word “may”, when used by a scientist and in the absence of any stronger claims, means “we haven’t ruled out the possibility”.
What breaking news that is.
Stop the press! No, really, stop it!
So… What does work?
There are various ways of going about actually hacking hunger (and they stack; i.e. you can use multiple methods and get cumulative results), and we wrote about them here:
Enjoy!
Share This Post
-
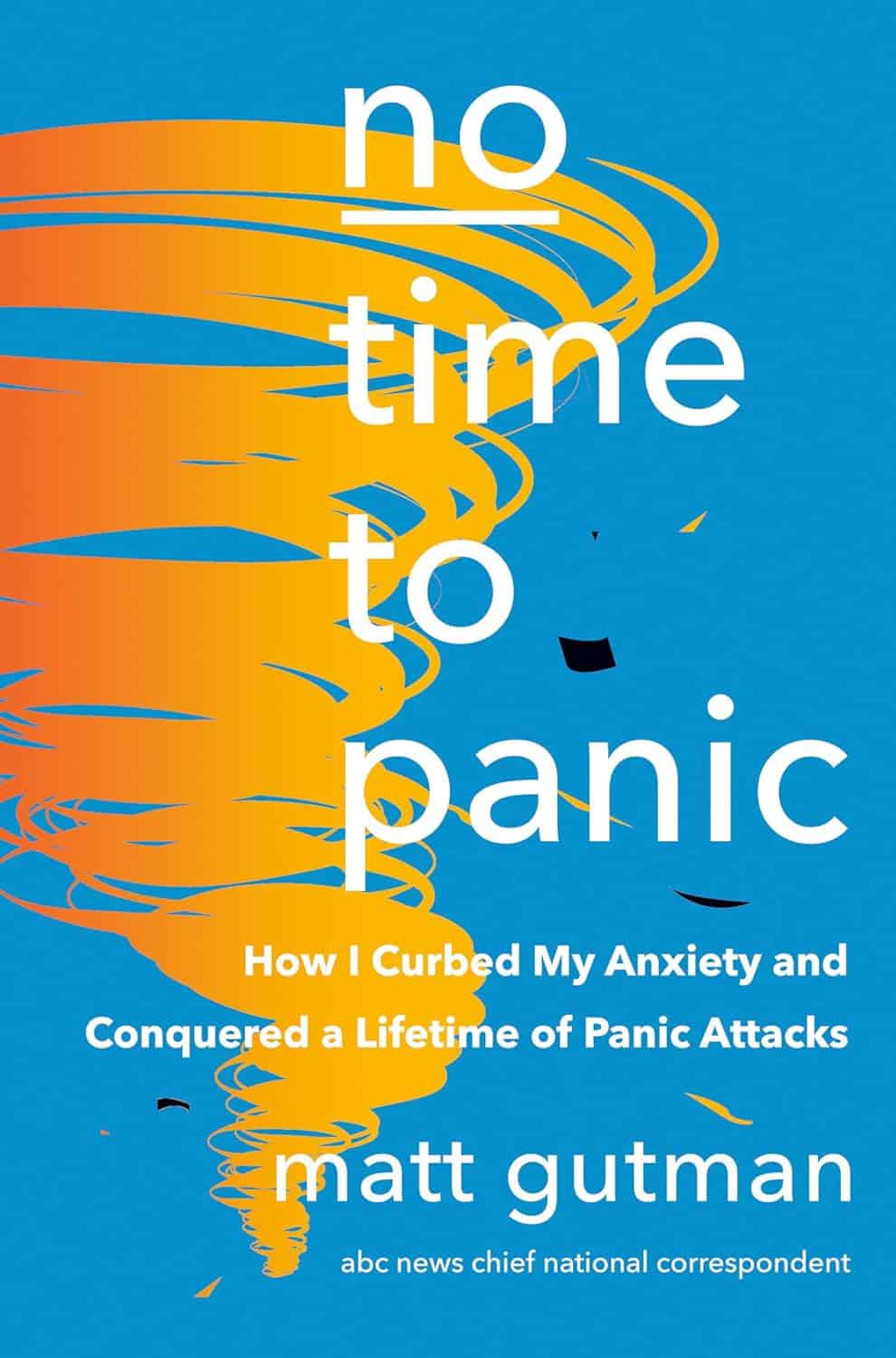
No Time to Panic – by Matt Gutman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Matt Gutman is not a doctor or a psychologist. He’s a journalist, accustomed to asking questions and then asking more probing questions, unrelenting until he gets the answers he’s looking for.
This book is the result of what happened when he needed to overcome his own anxiety and panic attacks, and went on an incisive investigative journey.
The style is as clear and accessible as you’d expect of a journalist, and presents a very human exploration, nonetheless organized in a way that will be useful to the reader.
It’s said that “experience is a great teacher, but she sends hefty bills”. In this case as in many, it’s good to learn from someone else’s experience!
By the end of the book, you’ll have a good grounding in most approaches to dealing with anxiety and panic attacks, and an idea of efficacy/applicability, and what to expect.
Bottom line: without claiming any magic bullet, this book presents six key strategies that Gutman found to work, along with his experiences of what didn’t. Valuable reading if you want to curb your own anxiety, or want to be able to help/support someone else with theirs.
Click here to check out No Time To Panic, and find the peace you deserve!
Share This Post
-
Fasting, eating earlier in the day or eating fewer meals – what works best for weight loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, one in eight people are living with obesity. This is an issue because excess fat increases the risk of type 2 diabetes, heart disease and certain cancers.
Modifying your diet is important for managing obesity and preventing weight gain. This might include reducing your calorie intake, changing your eating patterns and prioritising healthy food.
But is one formula for weight loss more likely to result in success than another? Our new research compared three weight-loss methods, to see if one delivered more weight loss than the others:
- altering calorie distribution – eating more calories earlier rather than later in the day
- eating fewer meals
- intermittent fasting.
We analysed data from 29 clinical trials involving almost 2,500 people.
We found that over 12 weeks or more, the three methods resulted in similar weight loss: 1.4–1.8kg.
So if you do want to lose weight, choose a method that works best for you and your lifestyle.
chalermphon_tiam/Shutterstock Eating earlier in the day
When our metabolism isn’t functioning properly, our body can’t respond to the hormone insulin properly. This can lead to weight gain, fatigue and can increase the risk of a number of chronic diseases such as diabetes.
Eating later in the day – with a heavy dinner and late-night snacking – seems to lead to worse metabolic function. This means the body becomes less efficient at converting food into energy, managing blood sugar and regulating fat storage.
In contrast, consuming calories earlier in the day appears to improve metabolic function.
However, this might not be the case for everyone. Some people naturally have an evening “chronotype”, meaning they wake up and stay up later.
People with this chronotype appear to have less success losing weight, no matter the method. This is due to a combination of factors including genes, an increased likelihood to have a poorer diet overall and higher levels of hunger hormones.
Eating fewer meals
Skipping breakfast is common, but does it hinder weight loss? Or is a larger breakfast and smaller dinner ideal?
While frequent meals may reduce disease risk, recent studies suggest that compared to eating one to two meals a day, eating six times a day might increase weight loss success.
However, this doesn’t reflect the broader research, which tends to show consuming fewer meals can lead to greater weight loss. Our research suggests three meals a day is better than six. The easiest way to do this is by cutting out snacks and keeping breakfast, lunch and dinner.
Most studies compare three versus six meals, with limited evidence on whether two meals is better than three.
However, front-loading your calories (consuming most of your calories between breakfast and lunch) appears to be better for weight loss and may also help reduce hunger across the day. But more studies with a longer duration are needed.
Fasting, or time-restricted eating
Many of us eat over a period of more than 14 hours a day.
Eating late at night can throw off your body’s natural rhythm and alter how your organs function. Over time, this can increase your risk of type 2 diabetes and other chronic diseases, particularly among shift workers.
Time-restricted eating, a form of intermittent fasting, means eating all your calories within a six- to ten-hour window during the day when you’re most active. It’s not about changing what or how much you eat, but when you eat it.
Some people limit their calories to a six hour window, while others opt for ten hours. Shutterstock/NIKS ADS Animal studies suggest time-restricted eating can lead to weight loss and improved metabolism. But the evidence in humans is still limited, especially about the long-term benefits.
It’s also unclear if the benefits of time-restricted eating are due to the timing itself or because people are eating less overall. When we looked at studies where participants ate freely (with no intentional calorie limits) but followed an eight-hour daily eating window, they naturally consumed about 200 fewer calories per day.
What will work for you?
In the past, clinicians have thought about weight loss and avoiding weight gain as a simile equation of calories in and out. But factors such as how we distribute our calories across the day, how often we eat and whether we eat late at night may also impact our metabolism, weight and health.
There are no easy ways to lose weight. So choose a method, or combination of methods, that suits you best. You might consider
- aiming to eat in an eight-hour window
- consuming your calories earlier, by focusing on breakfast and lunch
- opting for three meals a day, instead of six.
The average adult gains 0.4 to 0.7 kg per year. Improving the quality of your diet is important to prevent this weight gain and the strategies above might also help.
Finally, there’s still a lot we don’t know about these eating patterns. Many existing studies are short-term, with small sample sizes and varied methods, making it hard to make direct comparisons.
More research is underway, including well-controlled trials with larger samples, diverse populations and consistent methods. So hopefully future research will help us better understand how altering our eating patterns can result in better health.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University and Loai Albarqouni, Assistant Professor | NHMRC Emerging Leadership Fellow, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Polyphenol Paprika Pepper Penne
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s easier to promptly prepare than it is to pronounce unprepared! Ok, enough alliteration: this dish is as full of flavor as it is full of antioxidants, and it’s great for digestive health and heart health too.
You will need
- 4 large red bell peppers, diced
- 2 red onions, roughly chopped
- 1 bulb garlic, finely chopped
- 2 cups cherry tomatoes, halved
- 10oz wholemeal penne pasta
- 1 tbsp nutritional yeast
- 1 tbsp smoked paprika
- 1 tbsp black pepper
- Extra virgin olive oil for drizzling
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 200℃ / 400℉ / Gas mark 6
2) Put the vegetables in a roasting tin; drizzle with oil, sprinkle with the seasonings (nooch, paprika, black pepper), stir well to mix and distribute the seasonings evenly, and roast for 20–25 minutes, stirring/turning occasionally. When the edges begin to caramelize, turn off the heat, but leave to keep warm.
3) Cook the penne al dente (this should take 7–8 minutes in boiling salted water). Rinse in cold water, then pass a kettle of hot water over them to reheat. This process removed starch and lowered the glycemic index, before reheating the pasta so that it’s hot to serve.
4) Place the roasted vegetables in a food processor and blitz for just a few seconds. You want to produce a very chunky sauce—but not just chunks or just sauce.
5) Combine the sauce and pasta to serve immediately.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Bell Peppers To Pick? A Spectrum Of Specialties ← note how red bell peppers are perfect for this, as their lycopene quadruples in bioavailability when cooked
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- The Many Health Benefits Of Garlic
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vaccines and cancer: The myth that won’t die
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Two recent studies reported rising cancer rates among younger adults in the U.S. and worldwide. This prompted some online anti-vaccine accounts to link the studies’ findings to COVID-19 vaccines.
But, as with other myths, the data tells a very different story.
What you need to know
- Baseless claims that COVID-19 vaccines cause cancer have persisted online for several years and gained traction in late 2023.
- Two recent reports finding rising cancer rates among younger adults are based on pre-pandemic cancer incidence data. Cancer rates in the U.S. have been on the rise since the 1990s.
- There is no evidence of a link between COVID-19 vaccination and increased cancer risk.
False claims about COVID-19 vaccines began circulating months before the vaccines were available. Chief among these claims was misinformed speculation that vaccine mRNA could alter or integrate into vaccine recipients’ DNA.
It does not. But that didn’t prevent some on social media from spinning that claim into a persistent myth alleging that mRNA vaccines can cause or accelerate cancer growth. Anti-vaccine groups even coined the term “turbo cancer” to describe a fake phenomenon of abnormally aggressive cancers allegedly linked to COVID-19 vaccines.
They used the American Cancer Society’s 2024 cancer projection—based on incidence data through 2020—and a study of global cancer trends between 1999 and 2019 to bolster the false claims. This exposed the dishonesty at the heart of the anti-vaccine messaging, as data that predated the pandemic by decades was carelessly linked to COVID-19 vaccines in viral social media posts.
Some on social media cherry-pick data and use unfounded evidence because the claims that COVID-19 vaccines cause cancer are not true. According to the National Cancer Institute and American Cancer Society, there is no evidence of any link between COVID-19 vaccines and an increase in cancer diagnosis, progression, or remission.
Why does the vaccine cancer myth endure?
At the root of false cancer claims about COVID-19 vaccines is a long history of anti-vaccine figures falsely linking vaccines to cancer. Polio and HPV vaccines have both been the target of disproven cancer myths.
Not only do HPV vaccines not cause cancer, they are one of only two vaccines that prevent cancer.
In the case of polio vaccines, some early batches were contaminated with simian virus 40 (SV40), a virus that is known to cause cancer in some mammals but not humans. The contaminated batches were discovered, and no other vaccine has had SV40 contamination in over 60 years.
Follow-up studies found no increase in cancer rates in people who received the SV40-contaminated polio vaccine. Yet, vaccine opponents have for decades claimed that polio vaccines cause cancer.
Recycling of the SV40 myth
The SV40 myth resurfaced in 2023 when vaccine opponents claimed that COVID-19 vaccines contain the virus. In reality, a small, nonfunctional piece of the SV40 virus is used in the production of some COVID-19 vaccines. This DNA fragment, called the promoter, is commonly used in biomedical research and vaccine development and doesn’t remain in the finished product.
Crucially, the SV40 promoter used to produce COVID-19 vaccines doesn’t contain the part of the virus that enters the cell nucleus and is associated with cancer-causing properties in some animals. The promoter also lacks the ability to survive on its own inside the cell or interact with DNA. In other words, it poses no risk to humans.
Over 5.6 billion people worldwide have received COVID-19 vaccines since December 2020. At that scale, even the tiniest increase in cancer rates in vaccinated populations would equal hundreds of thousands of excess cancer diagnoses and deaths. The evidence for alleged vaccine-linked cancer would be observed in real incidence, treatment, and mortality data, not social media anecdotes or unverifiable reports.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: