Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dogs Paired With Providers at Hospitals Help Ease Staff and Patient Stress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
DENVER — Outside HCA HealthONE Rose medical center, the snow is flying. Inside, on the third floor, there’s a flurry of activity within the labor and delivery unit.
“There’s a lot of action up here. It can be very stressful at times,” said Kristina Fraser, an OB-GYN in blue scrubs.
Nurses wheel a very pregnant mom past.
“We’re going to bring a baby into this world safely,” Fraser said, “and off we go.”
She said she feels ready in part due to a calming moment she had just a few minutes earlier with some canine colleagues.
A pair of dogs, tails wagging, had come by a nearby nursing station, causing about a dozen medical professionals to melt into a collective puddle of affection. A yellow Lab named Peppi showered Fraser in nuzzles and kisses. “I don’t know if a human baby smells as good as that puppy breath!” Fraser had said as her colleagues laughed.
The dogs aren’t visitors. They work here, too, specifically for the benefit of the staff. “I feel like that dog just walks on and everybody takes a big deep breath and gets down on the ground and has a few moments of just decompressing,” Fraser said. “It’s great. It’s amazing.”
Hospital staffers who work with the dogs say there is virtually no bite risk with the carefully trained Labradors, the preferred breed for this work.
The dogs are kept away from allergic patients and washed regularly to prevent germs from spreading, and people must wash their hands before and after petting them.
Doctors and nurses are facing a growing mental health crisis driven by their experiences at work. They and other health care colleagues face high rates of depression, anxiety, stress, suicidal ideation, and burnout. Nearly half of health workers reported often feeling burned out in 2022, an increase from 2018, according to the Centers for Disease Control and Prevention. And the percentage of health care workers who reported harassment at work more than doubled over that four-year period. Advocates for the presence of dogs in hospitals see the animals as one thing that can help.
That includes Peppi’s handler, Susan Ryan, an emergency medicine physician at Rose.
Ryan said years working as an emergency room doctor left her with symptoms of PTSD. “I just was messed up and I knew it,” said Ryan, who isolated more at home and didn’t want to engage with friends. “I shoved it all in. I think we all do.”
She said doctors and other providers can be good at hiding their struggles, because they have to compartmentalize. “How else can I go from a patient who had a cardiac arrest, deal with the family members telling them that, and go to a room where another person is mad that they’ve had to wait 45 minutes for their ear pain? And I have to flip that switch.”
To cope with her symptoms of post-traumatic stress disorder, Ryan started doing therapy with horses. But she couldn’t have a horse in her backyard, so she got a Labrador.
Ryan received training from a national service dog group called Canine Companions, becoming the first doctor trained by the group to have a facility dog in an emergency room. Canine Companions has graduated more than 8,000 service dogs.
The Rose medical center gave Ryan approval to bring a dog to work during her ER shifts. Ryan’s colleagues said they are delighted that a dog is part of their work life.
“When I have a bad day at work and I come to Rose and Peppi is here, my day’s going to be made better,” EMT Jasmine Richardson said. “And if I have a patient who’s having a tough day, Peppi just knows how to light up the room.”
Nursing supervisor Eric Vaillancourt agreed, calling Peppi “joyful.”
Ryan had another dog, Wynn, working with her during the height of the pandemic. She said she thinks Wynn made a huge difference. “It saved people,” she said. “We had new nurses that had never seen death before, and now they’re seeing a covid death. And we were worried sick we were dying.”
She said her hospital system has lost a couple of physicians to suicide in the past two years, which HCA confirmed to KFF Health News and NPR. Ryan hopes the canine connection can help with trauma. “Anything that brings you back to the present time helps ground you again. A dog can be that calming influence,” she said. “You can get down on the ground, pet them, and you just get calm.”
Ryan said research has shown the advantages. For example, one review of dozens of original studies on human-animal interactions found benefits for a variety of conditions including behavioral and mood issues and physical symptoms of stress.
Rose’s president and CEO, Casey Guber, became such a believer in the canine connection he got his own trained dog to bring to the hospital, a black Lab-retriever mix named Ralphie.
She wears a badge: Chief Dog Officer.
Guber said she’s a big morale booster. “Phenomenal,” he said. “It is not uncommon to see a surgeon coming down to our administration office and rolling on the ground with Ralphie, or one of our nurses taking Ralphie out for a walk in the park.”
This article is from a partnership that includes CPR News, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Why You Can’t Just “Get Over” Trauma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time does not, in fact, heal all wounds. Sometimes they even compound themselves over time. Dr. Tracey Marks explains the damage that trauma does—the physiological presentation of “the axe forgets but the tree remembers”—and how to heal from that actual damage.
The science of healing
Trauma affects the mind and body (largely because the brain is, of course, both—and affects pretty much everything else), which can ripple out into all areas of life.
On the physical level, brain areas affected by trauma include:
- Amygdalae: becomes hyperactive, keeping a person in a heightened state of vigilance.
- Hippocampi: can shrink, causing fragmented or missing memories.
- Prefrontal cortex: reduces in activity, impairing decision-making and emotional regulation.
Trauma also activates the body’s fight or flight response, releasing stress hormones like cortisol and adrenaline. These are great things to have a pinch, but having them elevated all the time is equivalent to only ever driving your car at top speed—the only question becomes whether you’ll crash and burn before you break down.
However, there is hope! Neuroplasticity (the brain’s ability to rewire itself) can make trauma recovery possible through various interventions.
Evidence-based therapies for trauma include:
- Eye Movement Desensitization and Reprocessing (EMDR): this can help reprocess traumatic memories and reduce emotional intensity.
- Trauma-focused Cognitive Behavioral Therapy (CBT): this can help change unhelpful thought patterns and includes exposure therapy.
- Somatic therapies: these focus on the body and nervous system to release stored tension.
In this latter category, embodiment is key to trauma recovery—this may sound “wishy-washy”, but the evidence shows that reconnecting with the body does help manage emotional stress responses. Mind-body practices like mindfulness, yoga, and breathwork help cultivate embodiment and reduce trauma-related stress.
In short: you can’t just “get over” it, but with the right support and interventions, it’s possible to rewire the brain and body toward resilience and healing.
For more on all of this from Dr. Marks, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- PTSD, But, Well…. Complex.
- Undoing The Damage Of Life’s Hard Knocks
- A Surprisingly Powerful Tool: Eye Movement Desensitization & Reprocessing
Take care!
Share This Post
-
Rebounding Into The Best Of Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Trampoline” is a brand-name that’s been popularized as a generic name, and “rebounding”, the name used in this video, is the same thing as “trampolining”. With that in mind, let us bounce swiftly onwards:
Surprising benefits
It’s easy to think “isn’t that cheating?” to the point that such “cheating” could be useless, since surely the device is doing most of the work?
The thing is, while indeed it’s doing a lot of the work for you, your muscles are still doing a lot—mostly stabilization work, which is of course a critical thing for our muscles to be able to do. While it’s rare that we need to do a somersault in everyday life, it’s common that we have to keep ourselves from falling over, after all.
It also represents a kind of gentle resistance exercise, and as such, improves bone density—something first discovered during NASA research for astronauts. Other related benefits pertain to the body’s ability to deal with acceleration and deceleration; it also benefits the lymphatic system, which unlike the blood’s circulatory system, has no pump of its own. Rebounding does also benefit the cardiovascular system, though, as now the heart gets confused (in the healthy way, a little like it gets confused with high-intensity interval training).
Those are the main evidence-based benefits; anecdotally (but credibly, since these things can be said of most exercise) it’s also claimed that it benefits posture, improves sleep and mood, promotes weight loss and better digestion, reduces bloating, improves skin (the latter being due to improved circulation), and alleviates arthritis (most moderate exercise improves immune response, and thus reduces chronic inflammation, so again, this is reasonable, even if anecdotal).
For more details on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Exercise Less, Move More
- How To Do HIIT (Without Wrecking Your Body)
- Resistance Is Useful! (Especially As We Get Older)
- HIIT, But Make It HIRT
- The Lymphatic System Against Cancer & More
Take care!
Share This Post
Related Posts
-
I’ve recovered from a cold but I still have a hoarse voice. What should I do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold, flu, COVID and RSV have been circulating across Australia this winter. Many of us have caught and recovered from one of these common upper respiratory tract infections.
But for some people their impact is ongoing. Even if your throat isn’t sore anymore, your voice may still be hoarse or croaky.
So what happens to the voice when we get a virus? And what happens after?
Here’s what you should know if your voice is still hoarse for days – or even weeks – after your other symptoms have resolved.
Why does my voice get croaky during a cold?
A healthy voice is normally clear and strong. It’s powered by the lungs, which push air past the vocal cords to make them vibrate. These vibrations are amplified in the throat and mouth, creating the voice we hear.
The vocal cords are two elastic muscles situated in your throat, around the level of your laryngeal prominence, or Adam’s apple. (Although everyone has one, it tends to be more pronounced in males.) The vocal cords are small and delicate – around the size of your fingernail. Any small change in their structure will affect how the voice sounds.
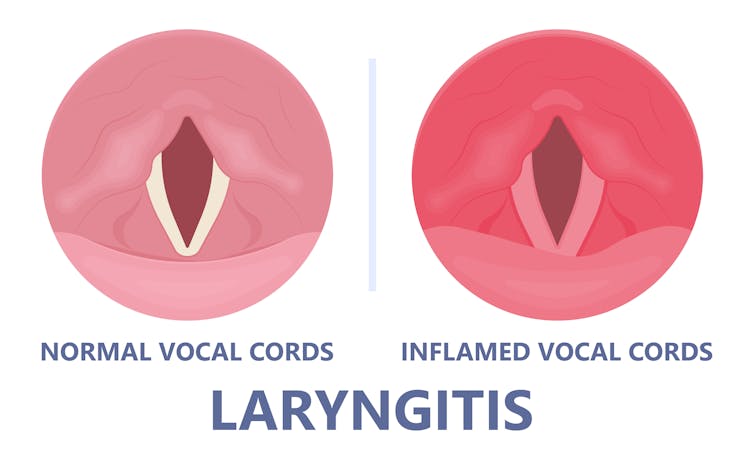
When the vocal cords become inflamed – known as laryngitis – your voice will sound different. Laryngitis is a common part of upper respiratory tract infections, but can also be caused through misuse.
Viruses such as the common cold can inflame the vocal cords. Pepermpron/Shutterstock Catching a virus triggers the body’s defence mechanisms. White blood cells are recruited to kill the virus and heal the tissues in the vocal cords. They become inflamed, but also stiffer. It’s harder for them to vibrate, so the voice comes out hoarse and croaky.
In some instances, you may find it hard to speak in a loud voice or have a reduced pitch range, meaning you can’t go as high or loud as normal. You may even “lose” your voice altogether.
Coughing can also make things worse. It is the body’s way of trying to clear the airways of irritation, including your own mucus dripping onto your throat (post-nasal drip). But coughing slams the vocal cords together with force.
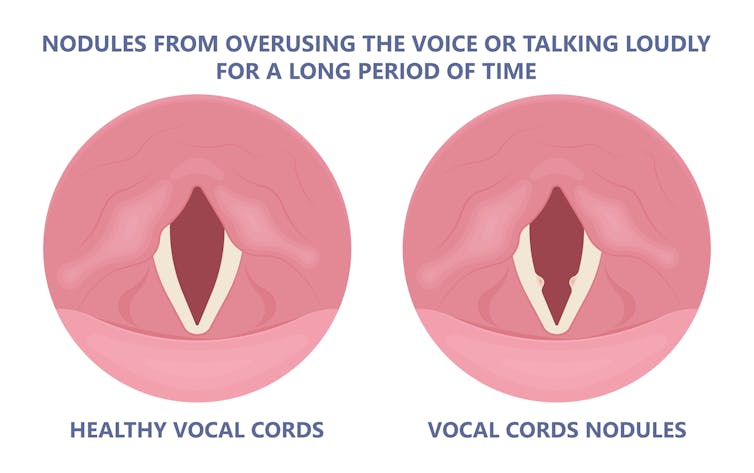
Chronic coughing can lead to persistent inflammation and even thicken the vocal cords. This thickening is the body trying to protect itself, similar to developing a callus when a pair of new shoes rubs.
Thickening on your vocal cords can lead to physical changes in the vocal cords – such as developing a growth or “nodule” – and further deterioration of your voice quality.
Coughing and exertion can cause inflamed vocal cords to thicken and develop nodules. Pepermpron/Shutterstock How can you care for your voice during infection?
People who use their voices a lot professionally – such as teachers, call centre workers and singers – are often desperate to resume their vocal activities. They are more at risk of forcing their voice before it’s ready.
The good news is most viral infections resolve themselves. Your voice is usually restored within five to ten days of recovering from a cold.
Occasionally, your pharmacist or doctor may prescribe cough suppressants to limit additional damage to the vocal cords (among other reasons) or mucolytics, which break down mucus. But the most effective treatments for viral upper respiratory tract infections are hydration and rest.
Drink plenty of water, avoid alcohol and exposure to cigarette smoke. Inhaling steam by making yourself a cup of hot water will also help clear blocked noses and hydrate your vocal cords.
Rest your voice by talking as little as possible. If you do need to talk, don’t whisper – this strains the muscles.
Instead, consider using “confidential voice”. This is a soft voice – not a whisper – that gently vibrates your vocal cords but puts less strain on your voice than normal speech. Think of the voice you use when communicating with someone close by.
During the first five to ten days of your infection, it is important not to push through. Exerting the voice by talking a lot or loudly will only exacerbate the situation. Once you’ve recovered from your cold, you can speak as you would normally.
What should you do if your voice is still hoarse after recovery?
If your voice hasn’t returned to normal after two to three weeks, you should seek medical attention from your doctor, who may refer you to an ear nose and throat specialist.
If you’ve developed a nodule, the specialist would likely refer you to a speech pathologist who will show you how to take care of your voice. Many nodules can be treated with voice therapy and don’t require surgery.
You may have also developed a habit of straining your vocal cords, if you forced yourself to speak or sing while they were inflamed. This can be a reason why some people continue to have a hoarse voice even when they’ve recovered from the cold.
In those cases, a speech pathologist may play a valuable role. They may teach you to exercises that make voicing more efficient. For example, lip trills (blowing raspberries) are a fun and easy way you can learn to relax the voice. This can help break the habit of straining your voice you may have developed during infection.
Yeptain Leung, Postdoctoral Research and Lecturer of Speech Pathology, School of Health Sciences, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Revealed: The Soviet Secret Recipe For Success That The CIA Admits Put The US To Shame
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s edition of 10almonds brings you a blast from the past with a modern twist: an ancient Russian peasant food that became a Soviet staple, and today, is almost unknown in the West.
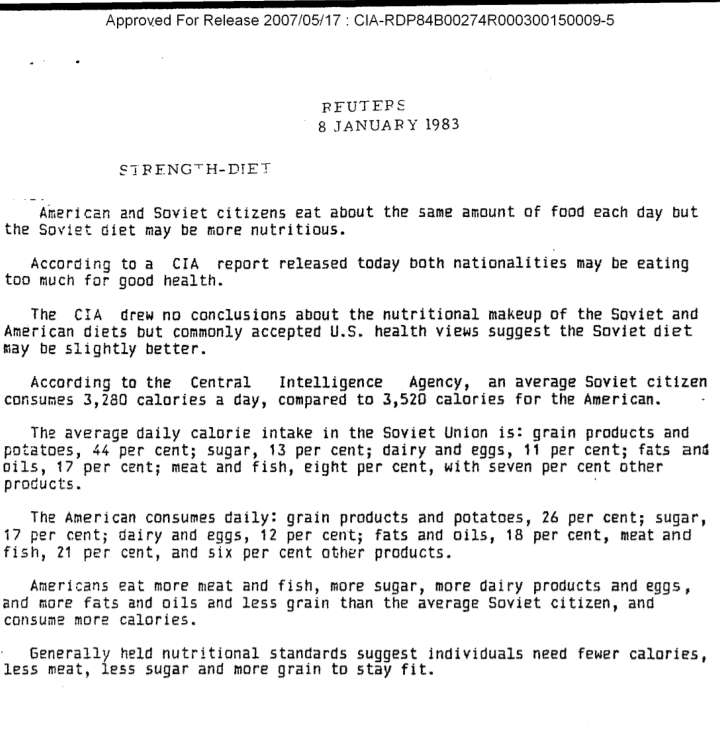
Before we get to that, let’s take a sneaky look at this declassified CIA memorandum from near the end of the Cold War:
(Click here to see a bigger version)
The take-away here is:
- Americans were eating 2–3 times more meat than Soviets
- Soviets were eating nearly double the amount of grain products and potatoes
…and both of these statistics meant that nutritionally speaking, the Soviets were doing better.
Americans also consumed more sugar and fats, which again, wasn’t the best dietary option.
But was the American diet tastier? Depends on whom you ask.
Which brings us to a literal recipe we’re going to be sharing with you today:
It’s not well-known in the West, but in Russia, it’s a famous national comfort food, a bastion of health and nutrition, and it rose to popularity because it was not only cheap and nutritious, but also, you could eat it for days without getting sick of it. And it could be easily frozen for reheating later without losing any of its appeal—it’d still be just as good.
In Russia there are sayings about it:
Щи да каша — пища наша (Shchi da kasha — pishcha nasha)
“Shchi and buckwheat are what we eat”
Top tip: buckwheat makes an excellent (and naturally sweet) alternative to porridge oats if prepared the same way!
Где щи, там и нас ищи (Gdye shchi, tam i nas ishchi)
“Where there’s shchi, us you’ll see”
Голь голью, а луковка во щах есть (Gol’ gol’yu, a lukovka vo shchakh yest’)
“I’m stark naked, but there’s shchi with onions”
There’s a very strong sentiment in Russia that really, all you need is shchi (shchi, shchi… shchi is all you need )
But what, you may ask, is shchi?
Our culinary cultural ambassador Nastja is here to offer her tried-and-tested recipe for…
…Russian cabbage soup (yes, really—bear with us now, and you can thank us later)
There are a lot of recipes for shchi (see for yourself what the Russian version of Lifehacker recommends), and we’ll be offering our favorite…
Nastja’s Nutritious and Delicious Homemade Shchi
Hi, Nastja here! I’m going to share with you my shchi recipe that is:
- Cheap
- So tasty
- Super nutritious*
- Vegan
- Gluten Free
You will also need:
- A cabbage (I use sweetheart, but any white cabbage will do)
- 1 cup (250g) red lentils (other kinds of lentils will work too)
- ½ lb or so (250–300g) tomatoes (I use baby plum tomatoes, but any kind will do)
- ½ lb or so (250–300g) mushrooms (the edible kind)
- An onion (I use a brown onion; any kind will do)
- Salt, pepper, rosemary, thyme, parsley, cumin
- Marmite or similar yeast extract (do you hate it? Me too. Trust me, it’ll be fine, you’ll love it. Omit if you’re a coward.)
- A little oil for sautéing (I use sunflower, but canola is fine, as is soy oil. Do not use olive oil or coconut oil, because the taste is too strong and the flashpoint too low)
First, what the French call mise-en-place, the prep work:
- Chop the cabbage into small strips, ⅛–¼ inch x 1 inch is a good guideline, but you can’t really go wrong unless you go to extremes
- Chop the tomatoes. If you’re using baby plum tomatoes (or cherry tomatoes), cut them in half. If using larger tomatoes, cut them into eighths (halve them, halve the halves, then halve the quarters)
- Chop the mushrooms. If using button mushrooms, half them. If using larger mushrooms, quarter them.
- Chop the onion finely.
- Gather the following kitchenware: A big pan (stock pot or similar), a sauté pan (a big wok or frying pan will do), a small frying pan (here a wok will not do), and a saucepan (a rice cook will also do)
Now, for actual cooking:
- Cook the red lentils until soft (I use a rice cooker, but a saucepan is fine) and set aside
- Sauté the cabbage, put it in the big pot (not yet on the heat!)
- Fry the mushrooms, put them in the big pot (still not yet on the heat!)
When you’ve done this a few times and/or if you’re feeling confident, you can do the above simultaneously to save time
- Blend the lentils into the water you cooked them in, and then add to the big pot.
- Turn the heat on low, and if necessary, add more water to make it into a rich soup
- Add the seasonings to taste, except the parsley. Go easy on the cumin, be generous with the rosemary and thyme, let your heart guide you with the salt and pepper.
- When it comes to the yeast extract: add about one teaspoon and stir it into the pot. Even if you don’t like Marmite, it barely changes the flavour (makes it slightly richer) and adds a healthy dose of vitamin B12.
We did not forget the tomatoes and the onion:
- Caramelize the onion (keep an eye on the big pot) and set it aside
- Fry the tomatoes and add them to the big pot
Last but definitely not least:
- Serve!
- The caramelized onion is a garnish, so put a little on top of each bowl of shchi
- The parsley is also a garnish, just add a little
Any shchi you don’t eat today will keep in the fridge for several days, or in the freezer for much longer.
*That nutritious goodness I talked about? Check it out:
- Lentils are high in protein and iron
- Cabbage is high in vitamin C and calcium
- Mushrooms are high in magnesium
- Tomatoes are good against inflammation
- Black pepper has a host of health benefits
- Yeast extract contains vitamin B12
Let us know how it went! We love to receive emails from our subscribers!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Breathing Cure – by Patrick McKeown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed this author’s “The Oxygen Advantage”, which as you might guess from the title, was also about breathing. So, what’s different here?
While The Oxygen Advantage was mostly about improving good health with optimized breathing, and with an emphasis on sports too, The Breathing Cure is more about the two-way relationship between ill health and disordered breathing (and how to fix it).
Many kinds of illnesses can affect our breathing, and our breathing can affect many types of illness; McKeown covers a lot of these, including the obvious things like respiratory diseases (including COVID and Long COVID, as well as non-infectious respiratory conditions like asthma), but also things like diabetes and heart disease, as well as peri-disease things like chronic pain, and demi-disease things like periods and menopause.
In each case (and more), he examines what things make matters better or worse, and how to improve them.
While the style itself is just as pop-science as The Oxygen Advantage, this time it relies less on anecdote (though there are plenty of anecdotes too), and leans more heavily on a generous chapter-by-chapter scientific bibliography, with plenty of citations to back up claims.
Bottom line: if you’d like to breathe better, this book can help in very many ways.
Click here to check out The Breathing Cure, and breathe easy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: