Chorus or Cacophony? Cicada Song Hits Some Ears Harder Than Others
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Shhhooo. Wee-uuu. Chick, chick, chick. That’s the sound of three different cicada species. For some people, those sounds are the song of the summer. Others wish the insects would turn it down. The cacophony can be especially irritating for people on the autism spectrum who have hearing sensitivity.
Warren Rickly, 14, lives in suburban south St. Louis County, Missouri. Warren, who has autism, was at the bus stop recently waiting for his younger brother when the sound of cicadas became too much to bear.
“He said it sounds like there’s always a train running next to him,” his mother, Jamie Reed, said.
Warren told her the noise hurt.
Starting this spring, trillions of the red-eyed insects crawled their way out of the ground across the Midwest and Southeast. It’s part of a rare simultaneous emergence of two broods — one that appears every 13 years, the other every 17.
The noisy insects can be stressful. People with autism can have a sensitivity to texture, brightness, and sound.
“I think the difference for individuals with autism is the level of intensity or how upsetting some of these sensory differences are,” said Rachel Follmer, a developmental and behavioral pediatrician at Lurie Children’s Hospital in Chicago.
“It can get to the extreme where it can cause physical discomfort,” she said.
When a large group of cicadas starts to sing, the chorus can be as loud as a motorcycle. Researchers at the University of Missouri-St. Louis this year crowdsourced cicada noise levels as high as 86 decibels, about as loud as a food blender.
That can be stressful, not melodic, Follmer said.
To help children cope, she suggests giving them a primer before they encounter a noisy situation. For cicadas, that could mean explaining what they are, that they don’t bite or sting, and that they’ll be here for just a short time.
“When something is uncomfortable, not having power in that situation can be very scary for a lot of individuals, whether you’re on the spectrum or not,” Follmer said.
Jamie Reed’s family has been using this and other strategies to help her son. Warren wears noise-canceling headphones, listens to music, and has been teaching himself about cicadas.
“For him, researching it and looking into it I think grounds him a little bit,” Reed said.
Fatima Husain is a professor and neuroscientist at the University of Illinois Urbana-Champaign and studies how the brain processes sound. She said people with tinnitus may also struggle with cicada song.
Tinnitus, a ringing or other noise in the ears, is a person’s perception of sound without an external source.
“Some people say it sounds like buzzing, like wind blowing through trees, and ironically, quite a few people say it sounds like cicadas,” Husain said.
For most people with tinnitus the cicada’s song is harmless background noise, according to Husain, but for others the ringing can prevent easy conversation or sleep. Those with tinnitus are also more likely to have anxiety or depression. A loud persistent sound, like singing cicadas, can make someone’s tinnitus worse, Husain said.
It’s not always bad, though. The cicada’s song can also be a relief.
For some, tinnitus gets worse in a quiet environment. Husain said she’s seen reports this year of patients saying the cicadas’ song has been like soothing white noise.
“The sound is loud enough that in some ways it’s drowning their internal tinnitus,” Husain said.
As loud as the cicadas can be, they won’t necessarily damage anyone’s hearing, according to the Centers for Disease Control and Prevention. Hearing loss builds up over time from repeated exposure to loud sounds. Cicadas aren’t loud enough for long enough to do lasting damage, Husain said.
Everyday sources of noise come with a higher risk. Husain said constant exposure to loud highways, an airport, industrial sites, or household appliances like blenders and hair dryers can be a concern. And they can take a toll on someone’s emotional well-being.
“If you are being exposed to very loud sounds for a part of your school day or your working day, it may make you more stressed out; it may make you more angry about things,” she said.
Unlike the highway or an airport, cicadas won’t be around long. Most of the current brood will be gone in the next few weeks. Just in time for another noisy summer event: the Fourth of July.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Study Tips for Exam Season?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Any study tips as we approach exam season? A lot of the productivity stuff is based on working life, but I can’t be the only student!
A: We’ve got you covered:
- Be passionate about your subject! We know of no greater study tip than that.
- Find a willing person and lecture them on your subject. When one teaches, two learn!
- Your mileage may vary depending on your subject, but, find a way of studying that’s fun to you!
- If you can get past papers, get as many as you can, and use those as your “last minute” studying in the week before your exam(s). This will prime you for answering exam-style questions (and leverage state-dependent memory). As a bonus, it’ll also help ease any anxiety, because by the time of your exam it’ll be “same old, same old”!
Share This Post
-
Homeopathy: Evidence So Tiny That It’s Not there?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Homeopathy: Evidence So Tiny That It’s Not There?
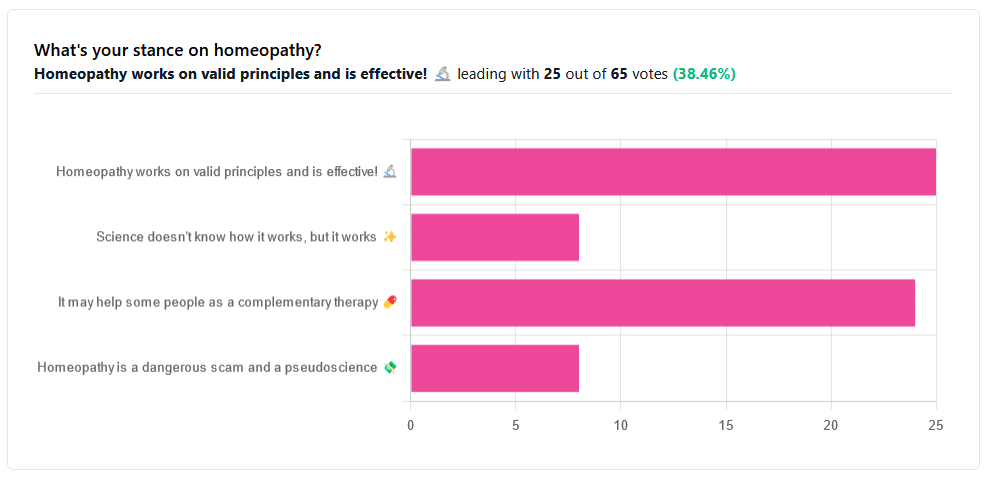
Yesterday, we asked you your opinions on homeopathy. The sample size of responses was a little lower than we usually get, but of those who did reply, there was a clear trend:
- A lot of enthusiasm for “Homeopathy works on valid principles and is effective”
- Near equal support for “It may help some people as a complementary therapy”
- Very few people voted for “Science doesn’t know how it works, but it works”; this is probably because people who considered voting for this, voted for the more flexible “It may help some people as a complementary therapy” instead.
- Very few people considered it a dangerous scam and a pseudoscience.
So, what does the science say?
Well, let us start our investigation by checking out the position of the UK’s National Health Service, an organization with a strong focus on providing the least expensive treatments that are effective.
Since homeopathy is very inexpensive to arrange, they will surely want to put it atop their list of treatments, right?
❝Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can cause the body to heal itself.
There’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.❞
The NHS actually has a lot more to say about that, and you can read their full statement here.
But that’s just one institution. Here’s what Australia’s National Health and Medical Research Council had to say:
❝There was no reliable evidence from research in humans that homeopathy was effective for treating the range of health conditions considered: no good-quality, well-designed studies with enough participants for a meaningful result reported either that homeopathy caused greater health improvements than placebo, or caused health improvements equal to those of another treatment❞
You can read their full statement here.
The American FDA, meanwhile, have a stronger statement:
❝Homeopathic drug products are made from a wide range of substances, including ingredients derived from plants, healthy or diseased animal or human sources, minerals and chemicals, including known poisons. These products have the potential to cause significant and even permanent harm if they are poorly manufactured, since that could lead to contaminated products or products that have potentially toxic ingredients at higher levels than are labeled and/or safe, or if they are marketed as substitute treatments for serious or life-threatening diseases and conditions, or to vulnerable populations.❞
You can read their full statement here.
Homeopathy is a dangerous scam and a pseudoscience: True or False?
False and True, respectively, mostly.
That may be a confusing answer, so let’s elaborate:
- Is it dangerous? Mostly not; it’s mostly just water. However, two possibilities for harm exist:
- Careless preparation could result in a harmful ingredient still being present in the water—and because of the “like cures like” principle, many of the ingredients used in homeopathy are harmful, ranging from heavy metals to plant-based neurotoxins. However, the process of “ultra-dilution” usually removes these so thoroughly that they are absent or otherwise scientifically undetectable.
- Placebo treatment has its place, but could result in “real” treatment going undelivered. This can cause harm if the “real” treatment was critically needed, especially if it was needed on a short timescale.
- Is it a scam? Probably mostly not; to be a scam requires malintent. Most practitioners probably believe in what they are practising.
- Is it a pseudoscience? With the exception that placebo effect has been highly studied and is a very valid complementary therapy… Yes, aside from that it is a pseudoscience. There is no scientific evidence to support homeopathy’s “like cures like” principle, and there is no scientific evidence to support homeopathy’s “water memory” idea. On the contrary, they go against the commonly understood physics of our world.
It may help some people as a complementary therapy: True or False?
True! Not only is placebo effect very well-studied, but best of all, it can still work as a placebo even if you know that you’re taking a placebo… Provided you also believe that!
Science doesn’t know how it works, but it works: True or False?
False, simply. At best, it performs as a placebo.
Placebo is most effective when it’s a remedy against subjective symptoms, like pain.
However, psychosomatic effect (the effect that our brain has on the rest of our body, to which it is very well-connected) can mean that placebo can also help against objective symptoms, like inflammation.
After all, our body, directed primarily by the brain, can “decide” what immunological defenses to deploy or hold back, for example. This is why placebo can help with conditions as diverse as arthritis (an inflammatory condition) or diabetes (an autoimmune condition, and/or a metabolic condition, depending on type).
Here’s how homeopathy measures up, for those conditions:
(the short answer is “no better than placebo”)
Homeopathy works on valid principles and is effective: True or False?
False, except insofar as placebo is a valid principle and can be effective.
The stated principles of homeopathy—”like cures like” and “water memory”—have no scientific basis.
We’d love to show the science for this, but we cannot prove a negative.
However, the ideas were conceived in 1796, and are tantamount to alchemy. A good scientific attitude means being open-minded to new ideas and testing them. In homeopathy’s case, this has been done, extensively, and more than 200 years of testing later, homeopathy has consistently performed equal to placebo.
In summary…
- If you’re enjoying homeopathic treatment and that’s working for you, great, keep at it.
- If you’re open-minded to enjoying a placebo treatment that may benefit you, be careful, but don’t let us stop you.
- If your condition is serious, please do not delay seeking evidence-based medical treatment.
Share This Post
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Share This Post
Related Posts
-
Infrared-Reflecting Patches For Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Hi! I’ve been reading about LifeWave patches, would you recommend them?❞
For reference first, this is talking about these: LifeWave.com
Short answer: no
Longer answer: their main premise seems to be that the patches (subscription prices seem to start from about $100–$300 per month) reflect infrared energy back into your body, making you more energized and healthy.
Fun fact: aluminum foil reflects infrared energy (which we feel as heat), by the way, and that is why space blankets (of the kind used in emergencies and by some athletes) are made shiny like that, often with aluminized mylar.
We cannot comment too closely on the rest of the presented science of their products, as it seems quite unlike anything we’re accustomed to reading, and we were not able to make a lot of sense of it.
They do cite research papers to back their claims, including research conducted by the company’s founder and published via an open journal.
Many others are independent studies conducted by often the same researchers as each other, mostly experts in acupuncture and acupressure.
For the papers we looked at, the sample sizes were very small, but the conclusions were very positive.
They were published in a variety of journals, of which we cannot claim any prior knowledge (i.e:, they were not the peer-reviewed journals from which we cite most of our sources).
Also, none were registered with ClinicalTrials.gov.
To be on the safe side, their disclaimer does advise:
❝LifeWave products are only intended to maintain or encourage a general state of health or healthy activity and are not intended to diagnose, treat, cure, mitigate, or prevent any disease or medical condition of the body❞
They do have a Frequently Asked Questions page, which tells about ancient Egyptian use of colored glass, as well as more modern considerations including joining, ordering, their commissions system, binary commissions and matching bonuses, and “how to rank up in LifeWave” as well as a lot of information about subscribing as a preferred customer or a brand partner, opting in to their multi-level marketing opportunities.
Here’s what “Honest Brand Reviews” had to say:
Honest Brand Reviews | LifeWave Review
Our position:
We cannot honestly claim to understand their science, and thus naturally won’t actively recommend what we can’t speak for.
An expert’s position:
Since we couldn’t understand how this would work, here’s what Dr. Paul Knoepfler has to say about their flagship product, the LifeWave X39 patch:
LifeWave X39 stem cell patch story has holes
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
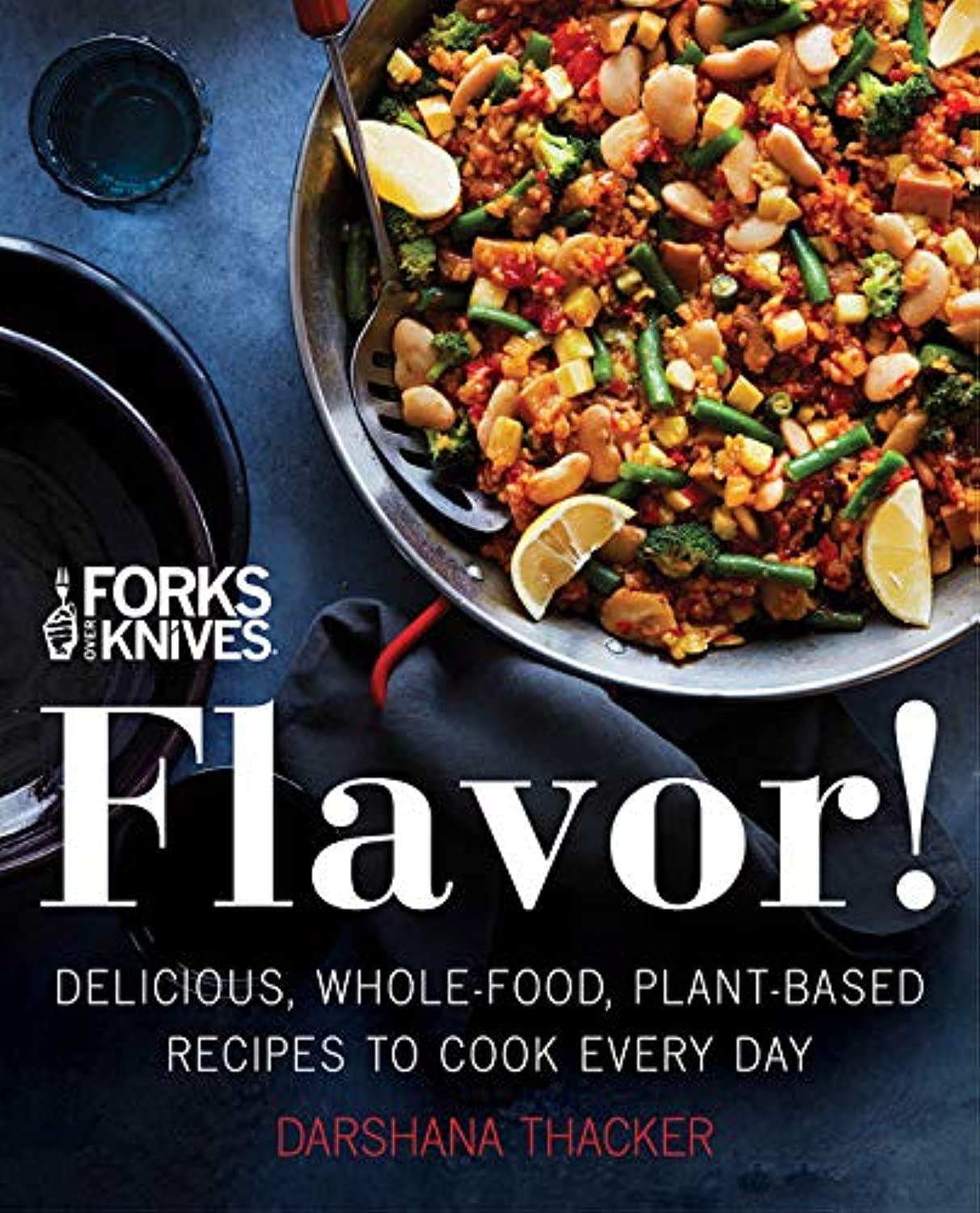
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut-Healthy Labneh Orecchiette
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Labneh (a sort of yogurt-cheese made from strained yogurt) is a great probiotic, and there’s plenty of resistant starch in this dish too, from how we cook, cool, and reheat the pasta. Add to this the lycopene from the tomatoes, the ergothioneine from the mushrooms, and the healthful properties of the garlic, black pepper, and red chili, and we have a very healthy dish!
You will need
- 10 oz labneh (if you can’t buy it locally, you can make your own by straining Greek yogurt through a muslin cloth, suspended over a bowl to catch the water that drips out, overnight—and yes, plant-based is also fine if you are vegan, and the gut benefits are similar because unlike vegan cheese, vegan yogurt is still fermented)
- 6 oz wholegrain orecchiette (or other pasta, but this shape works well for this sauce)
- ¼ bulb garlic, grated
- Juice of ½ lemon
- Large handful chopped parsley
- Large handful chopped dill
- 9 oz cherry tomatoes, halved
- 9 oz mushrooms (your choice what kind), sliced (unless you went for shiitake or similar, which don’t need it due to already being very thin)
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Cook the pasta as you normally would. Drain, and rinse with cold water. Set aside.
2) Combine the labneh with the garlic, black pepper, dill, parsley, and lemon juice, in a large bowl. Set aside.
3) Heat a little olive oil in a skillet; add the chili flakes, followed by the mushrooms. Cook until soft and browned, then add the tomatoes and fry for a further 1 minute—we want the tomatoes to be blistered, but not broken down. Stir in the MSG/salt, and take off the heat.
4) Refresh the pasta by passing a kettle of boiling water through it in a colander, then add the hot pasta to the bowl of labneh sauce, stirring to coat thoroughly.
5) Serve, spooning the mushrooms and tomatoes over the labneh pasta.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: