The Immunostimulant Superfood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat These Greens!
Chlorella vulgaris, henceforth “chlorella”, is a simple green algae that has a lot of health benefits.
Note: most of the studies here are for Chlorella vulgaris specifically. However, some are for other species of the Chlorella genus, of which Chlorella vulgaris is by far the most common, hence the name (vulgaris = common). The relevant phytochemical properties appear to be the same regardless.
Superfood
While people generally take it as a supplement rather than a food item in any kind of bulk, it is more than 50% protein and contains all 9 essential amino acids.
As you might expect of a green superfood, it’s also full of many antioxidants, most of them carotenoids, and these pack a punch, for example against cancer:
It also has a lot of vitamins and minerals, and even omega-3.
Which latter also means it helps improve lipids and is thus particularly…
Heart healthy
❝Daily consumption of Chlorella supplements provided the potential of health benefits reducing serum lipid risk factors, mainly triglycerides and total cholesterol❞
Its heart-healthy benefits don’t stop at lipids though, and include blood pressure management, as in this study that found…
❝GABA-rich Chlorella significantly decreased high-normal blood pressure and borderline hypertension, and is a beneficial dietary supplement for prevention of the development of hypertension. ❞
About that GABA, if you’re curious about that, check out:
GABA Against Stress, Anxiety, & More
May remove heavy metals
We’re going with “may” for this one as we could only find animal studies so far (probably because most humans don’t have megadoses of heavy metals in them, which makes testing harder).
Here’s an example animal study, though:
Enhanced elimination of tissue methyl mercury in [Chlorella]-fed mice
Immunostimulant
This one’s clearer, for example in this 8-week study (with humans) that found…
❝Serum concentrations of interferon-γ (p<0.05) and interleukin-1β (p<0.001) significantly increased and that of interleukin-12 (p<0.1) tended to increase in the Chlorella group.
The increments of these cytokines after the intervention were significantly bigger in the Chlorella group than those in the placebo group. In addition, NK cell activities (%) were significantly increased in Chlorella group, but not in Placebo group.
The increments of NK cell activities (%) were also significantly bigger in the Chlorella group than the placebo group.
Additionally, changed levels of NK cell activity were positively correlated with those of serum interleukin-1β (r=0.280, p=0.047) and interferon-γ (r=0.271, p<0.005).❞
tl;dr = it boosts numerous different kinds of immune cells
PS, if you click though to the study, you may be momentarily alarmed by the first paragraph of the abstract that says “However, there were no direct evidences for the effect of Chlorella supplementation on immune/inflammation response in healthy humans“
this is from the “Background” section of the abstract, so what they are saying is “before we did this study, nobody had done this yet”.
So, be assured that the results are worthwhile and compelling.
Is it safe?
Based on the studies, it has a good safety profile. However, as it boosts the immune system, you may want to check with your doctor if you have an autoimmune disorder, and/or you are on immunosuppressants.
And in general, of course always check with your doctor/pharmacist if unsure about any potential drug interactions.
Want some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
They Were Injured at the Super Bowl Parade. A Month Later, They Feel Forgotten.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
KFF Health News and KCUR are following the stories of people injured during the Feb. 14 mass shooting at the Kansas City Chiefs Super Bowl celebration. Listen to how one Kansas family is coping with the trauma.
Jason Barton didn’t want to attend the Super Bowl parade this year. He told a co-worker the night before that he worried about a mass shooting. But it was Valentine’s Day, his wife is a Kansas City Chiefs superfan, and he couldn’t afford to take her to games since ticket prices soared after the team won the championship in 2020.
So Barton drove 50 miles from Osawatomie, Kansas, to downtown Kansas City, Missouri, with his wife, Bridget, her 13-year-old daughter, Gabriella, and Gabriella’s school friend. When they finally arrived home that night, they cleaned blood from Gabriella’s sneakers and found a bullet in Bridget’s backpack.
Gabriella’s legs were burned by sparks from a ricocheted bullet, Bridget was trampled while shielding Gabriella in the chaos, and Jason gave chest compressions to a man injured by gunfire. He believes it was Lyndell Mays, one of two men charged with second-degree felony murder.
“There’s never going to be a Valentine’s Day where I look back and I don’t think about it,” Gabriella said, “because that’s a day where we’re supposed to have fun and appreciate the people that we have.”
One month after the parade in which the U.S. public health crisis that is gun violence played out on live television, the Bartons are reeling from their role at its epicenter. They were just feet from 43-year-old Lisa Lopez-Galvan, who was killed. Twenty-four other people were injured. Although the Bartons aren’t included in that official victim number, they were traumatized, physically and emotionally, and pain permeates their lives: Bridget and Jason keep canceling plans to go out, opting instead to stay home together; Gabriella plans to join a boxing club instead of the dance team.
During this first month, Kansas City community leaders have weighed how to care for people caught in the bloody crossfire and how to divide more than $2 million donated to public funds for victims in the initial outpouring of grief.
The questions are far-reaching: How does a city compensate people for medical bills, recovery treatments, counseling, and lost wages? And what about those who have PTSD-like symptoms that could last years? How does a community identify and care for victims often overlooked in the first flush of reporting on a mass shooting: the injured?
The injured list could grow. Prosecutors and Kansas City police are mounting a legal case against four of the shooting suspects, and are encouraging additional victims to come forward.
“Specifically, we’re looking for individuals who suffered wounds from their trying to escape. A stampede occurred while people were trying to flee,” said Jackson County Prosecutor Jean Peters Baker. Anyone who “in the fleeing of this event that maybe fell down, you were trampled, you sprained an ankle, you broke a bone.”
Meanwhile, people who took charge of raising money and providing services to care for the injured are wrestling with who gets the money — and who doesn’t. Due to large donations from celebrities like Taylor Swift and Travis Kelce, some victims or their families will have access to hundreds of thousands of dollars for medical expenses. Other victims may simply have their counseling covered.
The overall economic cost of U.S. firearm injuries is estimated by a recent Harvard Medical School study at $557 billion annually. Most of that — 88% — represented quality-of-life losses among those injured by firearms and their families. The JAMA-published study found that each nonfatal firearm injury leads to roughly $30,000 in direct health care spending per survivor in the first year alone.
In the immediate aftermath of the shootings, as well-intentioned GoFundMe pages popped up to help victims, executives at United Way of Greater Kansas City gathered to devise a collective donation response. They came up with “three concentric circles of victims,” said Jessica Blubaugh, the United Way’s chief philanthropy officer, and launched the #KCStrong campaign.
“There were folks that were obviously directly impacted by gunfire. Then the next circle out is folks that were impacted, not necessarily by gunshots, but by physical impact. So maybe they were trampled and maybe they tore a ligament or something because they were running away,” Blubaugh said. “Then third is folks that were just adjacent and/or bystanders that have a lot of trauma from all of this.”
PTSD, Panic, and the Echo of Gunfire
Bridget Barton returned to Kansas City the day after the shooting to turn in the bullet she found in her backpack and to give a statement at police headquarters. Unbeknownst to her, Mayor Quinton Lucas and the police and fire chiefs had just finished a press conference outside the building. She was mobbed by the media assembled there — interviews that are now a blur.
“I don’t know how you guys do this every day,” she remembered telling a detective once she finally got inside.
The Bartons have been overwhelmed by well wishes from close friends and family as they navigate the trauma, almost to the point of exhaustion. Bridget took to social media to explain she wasn’t ignoring the messages, she’s just responding as she feels able — some days she can hardly look at her phone, she said.
A family friend bought new Barbie blankets for Gabriella and her friend after the ones they brought to the parade were lost or ruined. Bridget tried replacing the blankets herself at her local Walmart, but when she was bumped accidentally, it triggered a panic attack. She abandoned her cart and drove home.
“I’m trying to get my anxiety under control,” Bridget said.
That means therapy. Before the parade, she was already seeing a therapist and planning to begin eye movement desensitization and reprocessing, a form of therapy associated with treating post-traumatic stress disorder. Now the shooting is the first thing she wants to talk about in therapy.
Since Gabriella, an eighth grader, has returned to middle school, she has dealt with the compounding immaturity of adolescence: peers telling her to get over it, pointing finger guns at her, or even saying it should have been her who was shot. But her friends are checking on her and asking how she’s doing. She wishes more people would do the same for her friend, who took off running when the shooting started and avoided injury. Gabriella feels guilty about bringing her to what turned into a horrifying experience.
“We can tell her all day long, ‘It wasn’t your fault. She’s not your responsibility.’ Just like I can tell myself, ‘It wasn’t my fault or my responsibility,’” Bridget said. “But I still bawled on her mom’s shoulder telling her how sorry I was that I grabbed my kid first.”
The two girls have spent a lot of time talking since the shooting, which Gabriella said helps with her own stress. So does spending time with her dog and her lizard, putting on makeup, and listening to music — Tech N9ne’s performance was a highlight of the Super Bowl celebration for her.
In addition to the spark burns on Gabriella’s legs, when she fell to the concrete in the pandemonium she split open a burn wound on her stomach previously caused by a styling iron.
“When I see that, I just picture my mom trying to protect me and seeing everyone run,” Gabriella said of the wound.
It’s hard not to feel forgotten by the public, Bridget said. The shooting, especially its survivors, have largely faded from the headlines aside from court dates. Two additional high-profile shootings have occurred in the area since the parade. Doesn’t the community care, she wonders, that her family is still living with the fallout every day?
“I’m going to put this as plainly as possible. I’m f—ing pissed because my family went through something traumatic,” Bridget vented in a recent social media post. “I don’t really want anything other [than], ‘Your story matters, too, and we want to know how you’re doing.’ Have we gotten that? Abso-f—lutely not.”
‘What Is the Landscape of Need?’
Helped in part by celebrities like Swift and Kelce, donations for the family of Lopez-Galvan, the lone fatality, and other victims poured in immediately after the shootings. Swift and Kelce donated $100,000 each. With the help of an initial $200,000 donation from the Kansas City Chiefs, the United Way’s #KCStrong campaign took off, reaching $1 million in the first two weeks and sitting at $1.2 million now.
Six verified GoFundMe funds were established. One solely for the Lopez-Galvan family has collected over $406,000. Smaller ones were started by a local college student and Swift fans. Churches have also stepped up, and one local coalition had raised $183,000, money set aside for Lopez-Galvan’s funeral, counseling services for five victims, and other medical bills from Children’s Mercy Kansas City hospital, said Ray Jarrett, executive director of Unite KC.
Money for Victims Rolls In
Donations poured in for those injured at the Super Bowl Parade in Kansas City after the Feb. 14 shootings. The largest, starting with a $200,000 donation from the Kansas City Chiefs, is at the United Way of Greater Kansas City. Six GoFundMe sites also popped up, due in part to $100,000 donations each from Taylor Swift and Travis Kelce. Here’s a look at the totals as of March 12.United Way#KCStrong: $1.2 million.Six Verified GoFundMe AccountsLisa Lopez-Galvan GoFundMe (Taylor Swift donated): $406,142Reyes Family GoFundMe (Travis Kelce donated): $207,035Samuel Arellano GoFundMe: $11,896Emily Tavis GoFundMe: $9,518Cristian Martinez’s GoFundMe for United Way: $2,967Swifties’ GoFundMe for Children’s Mercy hospital: $1,060ChurchesResurrection (Methodist) “Victims of Violence Fund”: $53,358‘The Church Loves Kansas City’: $183,000
Meanwhile, those leading the efforts found models in other cities. The United Way’s Blubaugh called counterparts who’d responded to their own mass shootings in Orlando, Florida; Buffalo, New York; and Newtown, Connecticut.
“The unfortunate reality is we have a cadre of communities across the country who have already faced tragedies like this,” Blubaugh said. “So there is an unfortunate protocol that is, sort of, already in place.”
#KCStrong monies could start being paid out by the end of March, Blubaugh said. Hundreds of people called the nonprofit’s 211 line, and the United Way is consulting with hospitals and law enforcement to verify victims and then offer services they may need, she said.
The range of needs is staggering — several people are still recovering at home, some are seeking counseling, and many weren’t even counted in the beginning. For instance, a plainclothes police officer was injured in the melee but is doing fine now, said Police Chief Stacey Graves.
Determining who is eligible for assistance was one of the first conversations United Way officials had when creating the fund. They prioritized three areas of focus: first were the wounded victims and their families, second was collaborating with organizations already helping victims in violence intervention and prevention and mental health services, and third were the first responders.
Specifically, the funds will be steered to cover medical bills, or lost wages for those who haven’t been able to work since the shootings, Blubaugh said. The goal is to work quickly to help people, she said, but also to spend the money in a judicious, strategic way.
“We don’t have a clear sightline of the entire landscape that we’re dealing with,” Blubaugh said. “Not only of how much money do we have to work with, but also, what is the landscape of need? And we need both of those things to be able to make those decisions.”
Firsthand Experience of Daily Kansas City Violence
Jason used his lone remaining sick day to stay home with Bridget and Gabriella. An overnight automation technician, he is the family’s primary breadwinner.
“I can’t take off work, you know?” he said. “It happened. It sucked. But it’s time to move on.”
“He’s a guy’s guy,” Bridget interjected.
On Jason’s first night back at work, the sudden sound of falling dishes startled Bridget and Gabriella, sending them into each other’s arms crying.
“It’s just those moments of flashbacks that are kicking our butts,” Bridget said.
Tell Us About Your Experience
We are continuing to report on the effects of the parade shooting on the people who were injured and the community as a whole. Do you have an experience you want to tell us about, or a question you think we should look into? Message KCUR’s text line at (816) 601-4777. Your information will not be used in an article without your permission.
In a way, the shooting has brought the family closer. They’ve been through a lot recently. Jason survived a heart attack and cancer last year. Raising a teenager is never easy.
Bridget can appreciate that the bullet lodged in her backpack, narrowly missing her, and that Gabriella’s legs were burned by sparks but she wasn’t shot.
Jason is grateful for another reason: It wasn’t a terrorist attack, as he initially feared. Instead, it fits into the type of gun violence he’d become accustomed to growing up in Kansas City, which recorded its deadliest year last year, although he’d never been this close to it before.
“This crap happens every single day,” he said. “The only difference is we were here for it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Mythbusting Cookware Materials
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
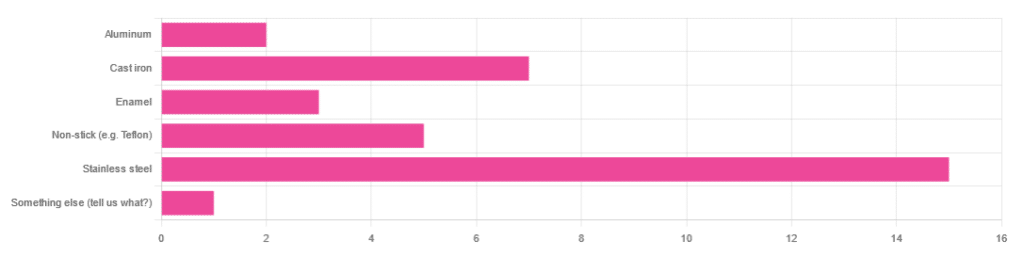
In Wednesday’s newsletter, we asked you what kind of cookware you mostly use, and got the above-depicted, below-described, set of responses:
- About 45% said stainless steel
- About 21% said cast iron
- About 15% said non-stick (e.g. Teflon)
- About 9% said enamel
- About 6% said aluminum
- And 1 person selected “something else”, but then commented to the contrary, writing “I use all of the above”
So, what does the science say about these options?
Stainless steel cookware is safe: True or False?
True! Assuming good quality and normal use, anyway. There really isn’t a lot to say about this, because it’s very unexciting. So long as it is what it is labelled as: there’s nothing coating it, nothing comes out of it unless you go to extremes*, and it’s easy to clean.
*If you cook for long durations at very high temperatures, it can leach nickel and chromium into food. What this means in practical terms: if you are using stainless steel to do deep-frying, then maybe stop that, and also consider going easy on deep-frying in general anyway, because obviously deep-frying is unhealthy for other reasons.
Per normal use, however: pretty much the only way (good quality) stainless steel cookware will harm you is if you touch it while it’s hot, or if it falls off a shelf onto your head.
That said, do watch out for cheap stainless steel cookware that can contain a lot of impurities, including heavy metals. Since you probably don’t have a mass spectrometer and/or chemistry lab at home to check for those impurities, your best guard here is simply to buy from a reputable brand with credible certifications.
Ceramic cookware is safe: True or False?
True… Most of the time! Ceramic pans usually have metal parts and a ceramic cooking surface coated with a very thin layer of silicon. Those metal parts will be as safe as the metals used, so if that’s stainless steel, you’re just as safe as the above. As for the silicon, it is famously inert and body-safe (which is why it’s used in body implants).
However: ceramic cookware that doesn’t have an obvious metal part and is marketed as being pure ceramic, will generally be sealed with some kind of glaze that can leach heavy metals contaminants into the food; here’s an example:
Lead toxicity from glazed ceramic cookware
Copper cookware is safe: True or False?
False! This is one we forgot to mention in the poll, as one doesn’t see a lot of it nowadays. The copper from copper pans can leach into food. Now, of course copper is an important mineral that we must get from our diet, but the amount of copper that that can leach into food from copper pans is far too much, and can induce copper toxicity.
In addition, copper cookware has been found to be, on average, highly contaminated with lead:
Non-stick cookware contaminates the food with microplastics: True or False?
True! If we were to discuss all the common non-stick contaminants here, this email would no longer fit (there’s a size limit before it gets clipped by most email services).
Suffice it to say: the non-stick coating, polytetrafluoroethylene, is itself a PFAS, that is to say, part of the category of chemicals considered environmental pollutants, and associated with a long list of health issues in humans (wherein the level of PFAS in our bloodstream is associated with higher incidence of many illnesses):
You may have noticed, of course, that the “non-stick” coating doesn’t stick very well to the pan, either, and will tend to come off over time, even if used carefully.
Also, any kind of wet cooking (e.g. saucepans, skillets, rice cooker inserts) will leach PFAS into the food. In contrast, a non-stick baking tray lined with baking paper (thus: a barrier between the tray and your food) is really not such an issue.
We wrote about PFAS before, so if you’d like a more readable pop-science article than the scientific paper above, then check out:
PFAS Exposure & Cancer: The Numbers Are High
Aluminum cookware contaminates the food with aluminum: True or False?
True! But not usually in sufficient quantities to induce aluminum toxicity, unless you are aluminum pans Georg who eats half a gram of aluminum per day, who is a statistical outlier and should not be counted.
That’s a silly example, but an actual number; the dose required for aluminum toxicity in blood is 100mg/L, and you have about 5 liters of blood.
Unless you are on kidney dialysis (because 95% of aluminum is excreted by the kidneys, and kidney dialysis solution can itself contain aluminum), you will excrete aluminum a lot faster than you can possibly absorb it from cookware. On the other hand, you can get too much of it from it being a permitted additive in foods and medications, for example if you are taking antacids they often have a lot of aluminum oxide in them—but that is outside the scope of today’s article.
However, aluminum may not be the real problem in aluminum pans:
❝In addition, aluminum (3.2 ± 0.25 to 4.64 ± 0.20 g/kg) and copper cookware (2.90 ± 0.12 g/kg) were highly contaminated with lead.
The time and pH-dependent study revealed that leaching of metals (Al, Pb, Ni, Cr, Cd, Cu, and Fe, etc.) into food was predominantly from anodized and non-anodized aluminum cookware.
More metal leaching was observed from new aluminum cookware compared to old. Acidic food was found to cause more metals to leach during cooking.❞
~ the same paper we cited when talking about copper
Cast iron cookware contaminates the food with iron: True or False?
True, but unlike with the other metals discussed, this is purely a positive, and indeed, it’s even recommended as a good way to fortify one’s diet with iron:
The only notable counterpoint we could find for this is if you have hemochromatosis, a disorder in which the body is too good at absorbing iron and holding onto it.
Thinking of getting some new cookware?
Here are some example products of high-quality safe materials on Amazon, but of course feel free to shop around:
Stainless Steel | Ceramic* | Cast Iron
*it says “non-stick” in the description, but don’t worry, it’s ceramic, not Teflon etc, and is safe
Bonus: rice cooker with stainless steel inner pot
Take care!
Share This Post
-
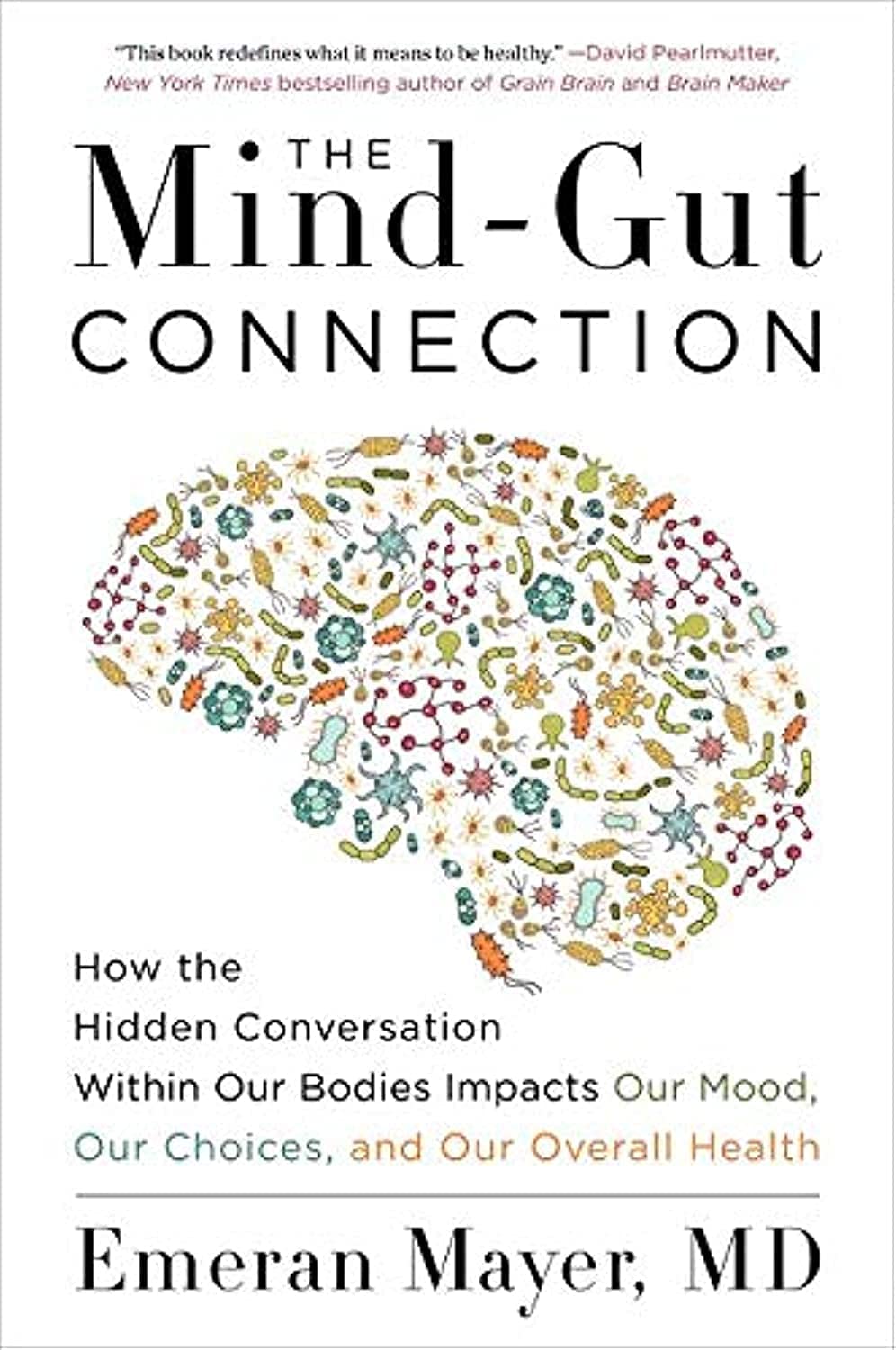
The Mind-Gut Connection – by Dr. Emeran Mayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the mind-gut connection before, so what makes this one stand out?
Firstly, it’s a lot more comprehensive than the usual “please, we’re begging you, eat some fiber”.
And yes, of course that’s part of it. Prebiotics, probiotics, reduce fried and processed foods, reduce sugar/alcohol, reduce meat, and again, eat some greenery.
But where this book really comes into its own is looking more thoroughly at the gut microbiota and their function. Dr. Mayer goes well beyond “there are good and bad bacteria” and looks at the relationship each of them have with the body’s many hormones, and especially neurotransmitters like serotonin and dopamine.
He also looks at the two-way connection between brain and gut. Yes, our gut gives us “gut feelings”, but 10% of communication between the brain and gut is in the other direction; he explores what that means for us, too.
Finally, he does give a lot of practical advice, not just dietary but also behavioral, to make the most of our mind-gut connection and make it work for our health, rather than against it.
Bottom line: this is the best book on the brain-gut connection that this reviewer has read so far, and certainly the most useful if you already know about gut-healthy nutrition, and are looking to take your understanding to the next level.
Click here to check out The Mind-Gut Connection, and start making yours work for your benefit!
Share This Post
Related Posts
-
The Mental Health First-Aid That You’ll Hopefully Never Need
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Take Your Mental Health As Seriously As General Health!
Sometimes, health and productivity means excelling—sometimes, it means avoiding illness and unproductivity. Both are essential, and today we’re going to tackle some ground-up stuff. If you don’t need it right now, great; we suggest to read it for when and if you do. But how likely is it that you will?
- One in four of us are affected by serious mental health issues in any given year.
- One in five of us have suicidal thoughts at some point in our lifetime.
- One in six of us are affected to at least some extent by the most commonly-reported mental health issues, anxiety and depression, in any given week.
…and that’s just what’s reported, of course. These stats are from a UK-based source but can be considered indicative generally. Jokes aside, the UK is not a special case and is not measurably worse for people’s mental health than, say, the US or Canada.
While this is not an inherently cheery topic, we think it’s an important one.
Depression, which we’re going to focus on today, is very very much a killer to both health and productivity, after all.
One of the most commonly-used measures of depression is known by the snappy name of “PHQ9”. It stands for “Patient Health Questionnaire Nine”, and you can take it anonymously online for free (without signing up for anything; it’s right there on the page already):
Take The PHQ9 Test Here! (under 2 minutes, immediate results)
There’s a chance you took that test and your score was, well, depressing. There’s also a chance you’re doing just peachy, or maybe somewhere in between. PHQ9 scores can fluctuate over time (because they focus on the past two weeks, and also rely on self-reports in the moment), so you might want to bookmark it to test again periodically. It can be interesting to track over time.
In the event that you’re struggling (or: in case one day you find yourself struggling, or want to be able to support a loved one who is struggling), some top tips that are useful:
Accept that it’s a medical condition like any other
Which means some important things:
- You/they are not lazy or otherwise being a bad person by being depressed
- You/they will probably get better at some point, especially if help is available
- You/they cannot, however, “just snap out of it”; illness doesn’t work that way
- Medication might help (it also might not)
Do what you can, how you can, when you can
Everyone knows the advice to exercise as a remedy for depression, and indeed, exercise helps many. Unfortunately, it’s not always that easy.
Did you ever see the 80s kids’ movie “The Neverending Story”? There’s a scene in which the young hero Atreyu must traverse the “Swamp of Sadness”, and while he has a magical talisman that protects him, his beloved horse Artax is not so lucky; he slows down, and eventually stops still, sinking slowly into the swamp. Atreyu pulls at him and begs him to keep going, but—despite being many times bigger and stronger than Atreyu, the horse just sinks into the swamp, literally drowning in despair.
See the scene: The Neverending Story movie clip – Artax and the Swamp of Sadness (1984)
Wow, they really don’t make kids’ movies like they used to, do they?
But, depression is very much like that, and advice “exercise to feel less depressed!” falls short of actually being helpful, when one is too depressed to do it.
If you’re in the position of supporting someone who’s depressed, the best tool in your toolbox will be not “here’s why you should do this” (they don’t care; not because they’re an uncaring person by nature, but because they are physiologically impeded from caring about themself at this time), but rather:
“please do this with me”
The reason this has a better chance of working is because the depressed person will in all likelihood be unable to care enough to raise and/or maintain an objection, and while they can’t remember why they should care about themself, they’re more likely to remember that they should care about you, and so will go with your want/need more easily than with their own. It’s not a magic bullet, but it’s worth a shot.
What if I’m the depressed person, though?
Honestly, the same, if there’s someone around you that you do care about; do what you can to look after you, for them, if that means you can find some extra motivation.
But I’m all alone… what now?
Firstly, you don’t have to be alone. There are free services that you can access, for example:
- US: https://nami.org/help
- Canada: https://www.wellnesstogether.ca/en-CA
- UK: https://www.samaritans.org/
…which varyingly offer advice, free phone services, webchats, and the like.
But also, there are ways you can look after yourself a little bit; do the things you’d advise someone else to do, even if you’re sure they won’t work:
- Take a little walk around the block
- Put the lights on when you’re not sleeping
- For that matter, get out of bed when you’re not sleeping. Literally lie on the floor if necessary, but change your location.
- Change your bedding, or at least your clothes
- If changing the bedding is too much, change just the pillowcase
- If changing your clothes is too much, change just one item of clothing
- Drink some water; it won’t magically cure you, but you’ll be in slightly better order
- On the topic of water, splash some on your face, if showering/bathing is too much right now
- Do something creative (that’s not self-harm). You may scoff at the notion of “art therapy” helping, but this is a way to get at least some of the lights on in areas of your brain that are a little dark right now. Worst case scenario is it’ll be a distraction from your problems, so give it a try.
- Find a connection to community—whatever that means to you—even if you don’t feel you can join it right now. Discover that there are people out there who would welcome you if you were able to go join them. Maybe one day you will!
- Hiding from the world? That’s probably not healthy, but while you’re hiding, take the time to read those books (write those books, if you’re so inclined), learn that new language, take up chess, take up baking, whatever. If you can find something that means anything to you, go with that for now, ride that wave. Motivation’s hard to come by during depression and you might let many things slide; you might as well get something out of this period if you can.
If you’re not depressed right now but you know you’re predisposed to such / can slip that way?
Write yourself instructions now. Copy the above list if you like.
Most of all: have a “things to do when I don’t feel like doing anything” list.
If you only take one piece of advice from today’s newsletter, let that one be it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women worry hormonal contraceptives have dangerous side-effects including increased cancer risk. But this perception is often out of proportion with the actual risks.
So, what does the research actually say about cancer risk for contraceptive users?
And is your cancer risk different if, instead of the pill, you use long-acting reversible contraceptives? These include intrauterine devices or IUDs (such as Mirena), implants under the skin (such as Implanon), and injections (such as Depo Provera).
Our new study, conducted by the University of Queensland and QIMR Berghofer Medical Research Institute and published by the Journal of the National Cancer Institute, looked at this question.
We found long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk (which is good news) but not necessarily any safer than the pill.
Peakstock/Shutterstock Some hormonal contraceptives take the form of implants under the skin. WiP-Studio/Shutterstock How does the contraceptive pill affect cancer risk?
The International Agency for Research on Cancer, which compiles evidence on cancer causes, has concluded that oral contraceptives have mixed effects on cancer risk.
Using the oral contraceptive pill:
- slightly increases your risk of breast and cervical cancer in the short term, but
- substantially reduces your risk of cancers of the uterus and ovaries in the longer term.
Our earlier work showed the pill was responsible for preventing far more cancers overall than it contributed to.
In previous research we estimated that in 2010, oral contraceptive pill use prevented over 1,300 cases of endometrial and ovarian cancers in Australian women.
It also prevented almost 500 deaths from these cancers in 2013. This is a reduction of around 25% in the deaths that could have occurred that year if women hadn’t taken the pill.
In contrast, we calculated the pill may have contributed to around 15 deaths from breast cancer in 2013, which is less than 0.5% of all breast cancer deaths in that year.
Previous work showed the pill was responsible for preventing far more cancers overall than it contributed to. Image Point Fr What about long-acting reversible contraceptives and cancer risk?
Long-acting reversible contraceptives – which include intrauterine devices or IUDs, implants under the skin, and injections – release progesterone-like hormones.
These are very effective contraceptives that can last from a few months (injections) up to seven years (intrauterine devices).
Notably, they don’t contain the hormone oestrogen, which may be responsible for some of the side-effects of the pill (including perhaps contributing to a higher risk of breast cancer).
Use of these long-acting contraceptives has doubled over the past decade, while the use of the pill has declined. So it’s important to know whether this change could affect cancer risk for Australian women.
Our new study of more than 1 million Australian women investigated whether long-acting, reversible contraceptives affect risk of invasive cancers. We compared the results to the oral contraceptive pill.
We used de-identified health records for Australian women aged 55 and under in 2002.
Among this group, about 176,000 were diagnosed with cancer between 2004 and 2013 when the oldest women were aged 67. We compared hormonal contraceptive use among these women who got cancer to women without cancer.
We found that long-term users of all types of hormonal contraception had around a 70% lower risk of developing endometrial cancer in the years after use. In other words, the risk of developing endometrial cancer is substantially lower among women who took hormonal contraception compared to those who didn’t.
For ovarian cancer, we saw a 50% reduced risk (compared to those who took no hormonal contraception) for women who were long-term users of the hormone-containing IUD.
The risk reduction was not as marked for the implants or injections, however few long-term users of these products developed these cancers in our study.
As the risk of endometrial and ovarian cancers increases with age, it will be important to look at cancer risk in these women as they get older.
What about breast cancer risk?
Our findings suggest that the risk of breast cancer for current users of long-acting contraceptives is similar to users of the pill.
However, the contraceptive injection was only associated with an increase in breast cancer risk after five years of use and there was no longer a higher risk once women stopped using them.
Our results suggested that the risk of breast cancer also reduces after stopping use of the contraceptive implants.
We will need to follow-up the women for longer to determine whether this is also the case for the IUD.
It is worth emphasising that the breast cancer risk associated with all hormonal contraceptives is very small.
About 30 in every 100,000 women aged 20 to 39 years develop breast cancer each year, and any hormonal contraceptive use would only increase this to around 36 cases per 100,000.
What about other cancers?
Our study did not show any consistent relationships between contraceptive use and other cancers types. However, we only at looked at invasive cancers (meaning those that start at a primary site but have the potential to spread to other parts of the body).
A recent French study found that prolonged use of the contraceptive injection increased the risk of meningioma (a type of benign brain tumour).
However, meningiomas are rare, especially in young women. There are around two cases in every 100,000 in women aged 20–39, so the extra number of cases linked to contraceptive injection use was small.
The French study found the hormonal IUD did not increase meningioma risk (and they did not investigate contraceptive implants).
Benefits and side-effects
There are benefits and side-effects for all medicines, including contraceptives, but it is important to know most very serious side-effects are rare.
A conversation with your doctor about the balance of benefits and side-effects for you is always a good place to start.
Susan Jordan, Professor of Epidemiology, The University of Queensland; Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland, and Penny Webb, Distinguished Scientist, Gynaecological Cancers Group, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Going Gluten-Free Could Be A Bad Idea
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is A Gluten-Free Diet Right For You?
This is Rachel Begun, MS, RD. She’s a nutritionist who, since her own diagnosis with Celiac disease, has shifted her career into a position of educating the public (and correcting misconceptions) about gluten sensitivity, wheat allergy, and Celiac disease. In short, the whole “gluten-free” field.
First, a quick recap
We’ve written on this topic ourselves before; here’s what we had to say:
On “Everyone should go gluten-free”
Some people who have gone gluten-free are very evangelical about the lifestyle change, and will advise everyone that it will make them lose weight, have clearer skin, more energy, and sing well, too. Ok, maybe not the last one, but you get the idea—a dietary change gets seen as a cure-all.
And for some people, it can indeed make a huge difference!
Begun urges us to have a dose of level-headedness in our approach, though.
Specifically, she advises:
- Don’t ignore symptoms, and/but…
- Don’t self-diagnose
- Don’t just quit gluten
One problem with self-diagnosis is that we can easily be wrong:
But why is that a problem? Surely there’s not a health risk in skipping the gluten just to be on the safe side? As it turns out, there actually is:
If we self-diagnose incorrectly, Begun points out, we can miss the actual cause of the symptoms, and by cheerfully proclaiming “I’m allergic to gluten” or such, a case of endometriosis, or Hashimoto’s, or something else entirely, might go undiagnosed and thus untreated.
“Oh, I feel terrible today, there must have been some cross-contamination in my food” when in fact, it’s an undiagnosed lupus flare-up, that kind of thing.
Similarly, just quitting gluten “to be on the safe side” can mask a different problem, if wheat consumption (for example) contributed to, but did not cause, some ailment.
In other words: it could reduce your undesired symptoms, but in so doing, leave a more serious problem unknown.
Instead…
If you suspect you might have a gluten sensitivity, a wheat allergy, or even Celiac disease, get yourself tested, and take professional advice on proceeding from there.
How? Your physician should be able to order the tests for you.
You can also check out resources available here:
Celiac Disease Foundation | How do I get tested?
Or for at-home gluten intolerance tests, here are some options weighed against each other:
MNT | 5 gluten intolerance tests and considerations
Want to learn more?
Begun has a blog:
Rachel Begun | More than just recipes
(it is, in fact, just recipes—but they are very simple ones!)
You also might enjoy this interview, in which she talks about gluten sensitivity, celiac disease, and bio-individuality:
Want to watch it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: