Children with traumatic experiences have a higher risk of obesity – but this can be turned around
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Children with traumatic experiences in their early lives have a higher risk of obesity. But as our new research shows, this risk can be reduced through positive experiences.
Childhood traumatic experiences are alarmingly common. Our analysis of data from nearly 5,000 children in the Growing Up in New Zealand study revealed almost nine out of ten (87%) faced at least one significant source of trauma by the time they were eight years old. Multiple adverse experiences were also prevalent, with one in three children (32%) experiencing at least three traumatic events.
Childhood trauma includes a range of experiences such as physical and emotional abuse, peer bullying and exposure to domestic violence. It also includes parental substance abuse, mental illness, incarceration, separation or divorce and ethnic discrimination.
We found children from financially disadvantaged households and Māori and Pasifika had the highest prevalence of nearly all types of adverse experiences, as well as higher overall numbers of adversities.
The consequences of these experiences were far-reaching. Children who experienced at least one adverse event were twice as likely to be obese by age eight. The risk increased with the number of traumatic experiences. Children with four or more adverse experiences were nearly three times more likely to be obese.
Notably, certain traumatic experiences (including physical abuse and parental domestic violence) related more strongly to obesity than others. This highlights the strong connection between early-life adversity and physical health outcomes.

Connecting trauma to obesity
One potential explanation could be that the accumulation of early stress in children’s family, school and social environments is associated with greater psychological distress. This in turn makes children more likely to adopt unhealthy weight-related behaviours.
This includes consuming excessive high-calorie “comfort” foods such as fast food and sugary drinks, inadequate intake of nutritious foods, poor sleep, excessive screen time and physical inactivity. In our research, children who experienced adverse events were more likely to adopt these unhealthy behaviours. These, in turn, were associated with a higher risk of obesity.
Despite these challenges, our research also explored a promising area: the protective and mitigating effects of positive experiences.
We defined positive experiences as:
- parents in a committed relationship
- mothers interacting well with their children
- mothers involved in social groups
- children engaged in enriching experiences and activities such as visiting libraries or museums and participating in sports and community events
- children living in households with routines and rules, including those regulating bedtime, screen time and mealtimes
- children attending effective early childhood education.
The findings were encouraging. Children with more positive experiences were significantly less likely to be obese by age eight.
For example, those with five or six positive experiences were 60% less likely to be overweight or obese compared to children with zero or one positive experience. Even two positive experiences reduced the likelihood by 25%.

How positive experiences counteract trauma
Positive experiences can help mitigate the negative effects of childhood trauma. But a minimum of four positive experiences was required to significantly counteract the impact of adverse events.
While nearly half (48%) of the study participants had at least four positive experiences, a concerning proportion (more than one in ten children) reported zero or only one positive experience.
The implications are clear. Traditional weight-loss programmes focused solely on changing behaviours are not enough to tackle childhood obesity. To create lasting change, we must also address the social environments, life experiences and emotional scars of early trauma shaping children’s lives.
Fostering positive experiences is a vital part of this holistic approach. These experiences not only help protect children from the harmful effects of adversity but also promote their overall physical and mental wellbeing. This isn’t just about preventing obesity – it’s about giving children the foundation to thrive and reach their full potential.
Creating supportive environments for vulnerable children
Policymakers, schools and families all have a role to play. Community-based programmes, such as after-school activities, healthy relationship initiatives and mental health services should be prioritised to support vulnerable families.
Trauma-informed care is crucial, particularly for children from disadvantaged households who face higher levels of adversity and fewer positive experiences. Trauma-informed approaches are especially crucial for addressing the effects of domestic violence and other adverse childhood experiences.
Comprehensive strategies should prioritise both safety and emotional healing by equipping families with tools to create safe, nurturing environments and providing access to mental health services and community support initiatives.
At the family level, parents can establish stable routines, participate in social networks and engage children in enriching activities. Schools and early-childhood education providers also play a key role in fostering supportive environments that help children build resilience and recover from trauma.
Policymakers should invest in resources that promote positive experiences across communities, addressing inequalities that leave some children more vulnerable than others. By creating nurturing environments, we can counterbalance the impacts of trauma and help children lead healthier, more fulfilling lives.
When positive experiences outweigh negative ones, children have a far greater chance of thriving – physically, emotionally and socially.
Ladan Hashemi, Senior Research Fellow in Health Sciences, University of Auckland, Waipapa Taumata Rau
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can Medical Schools Funnel More Doctors Into the Primary Care Pipeline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout her childhood, Julia Lo Cascio dreamed of becoming a pediatrician. So, when applying to medical school, she was thrilled to discover a new, small school founded specifically to train primary care doctors: NYU Grossman Long Island School of Medicine.
Now in her final year at the Mineola, New York, school, Lo Cascio remains committed to primary care pediatrics. But many young doctors choose otherwise as they leave medical school for their residencies. In 2024, 252 of the nation’s 3,139 pediatric residency slots went unfilled and family medicine programs faced 636 vacant residencies out of 5,231 as students chased higher-paying specialties.
Lo Cascio, 24, said her three-year accelerated program nurtured her goal of becoming a pediatrician. Could other medical schools do more to promote primary care? The question could not be more urgent. The Association of American Medical Colleges projects a shortage of 20,200 to 40,400 primary care doctors by 2036. This means many Americans will lose out on the benefits of primary care, which research shows improves health, leading to fewer hospital visits and less chronic illness.
Many medical students start out expressing interest in primary care. Then they end up at schools based in academic medical centers, where students become enthralled by complex cases in hospitals, while witnessing little primary care.
The driving force is often money, said Andrew Bazemore, a physician and a senior vice president at the American Board of Family Medicine. “Subspecialties tend to generate a lot of wealth, not only for the individual specialists, but for the whole system in the hospital,” he said.
A department’s cache of federal and pharmaceutical-company grants often determines its size and prestige, he said. And at least 12 medical schools, including Harvard, Yale, and Johns Hopkins, don’t even have full-fledged family medicine departments. Students at these schools can study internal medicine, but many of those graduates end up choosing subspecialties like gastroenterology or cardiology.
One potential solution: eliminate tuition, in the hope that debt-free students will base their career choice on passion rather than paycheck. In 2024, two elite medical schools — the Albert Einstein College of Medicine and the Johns Hopkins University School of Medicine — announced that charitable donations are enabling them to waive tuition, joining a handful of other tuition-free schools.
But the contrast between the school Lo Cascio attends and the institution that founded it starkly illustrates the limitations of this approach. Neither charges tuition.
In 2024, two-thirds of students graduating from her Long Island school chose residencies in primary care. Lo Cascio said the tuition waiver wasn’t a deciding factor in choosing pediatrics, among the lowest-paid specialties, with an average annual income of $260,000, according to Medscape.
At the sister school, the Manhattan-based NYU Grossman School of Medicine, the majority of its 2024 graduates chose specialties like orthopedics (averaging $558,000 a year) or dermatology ($479,000).
Primary care typically gets little respect. Professors and peers alike admonish students: If you’re so smart, why would you choose primary care? Anand Chukka, 27, said he has heard that refrain regularly throughout his years as a student at Harvard Medical School. Even his parents, both PhD scientists, wondered if he was wasting his education by pursuing primary care.
Seemingly minor issues can influence students’ decisions, Chukka said. He recalls envying the students on hospital rotations who routinely were served lunch, while those in primary care settings had to fetch their own.
Despite such headwinds, Chukka, now in his final year, remains enthusiastic about primary care. He has long wanted to care for poor and other underserved people, and a one-year clerkship at a community practice serving low-income patients reinforced that plan.
When students look to the future, especially if they haven’t had such exposure, primary care can seem grim, burdened with time-consuming administrative tasks, such as seeking prior authorizations from insurers and grappling with electronic medical records.
While specialists may also face bureaucracy, primary care practices have it much worse: They have more patients and less money to hire help amid burgeoning paperwork requirements, said Caroline Richardson, chair of family medicine at Brown University’s Warren Alpert Medical School.
“It’s not the medical schools that are the problem; it’s the job,” Richardson said. “The job is too toxic.”
Kevin Grumbach, a professor of family and community medicine at the University of California-San Francisco, spent decades trying to boost the share of students choosing primary care, only to conclude: “There’s really very little that we can do in medical school to change people’s career trajectories.”
Instead, he said, the U.S. health care system must address the low pay and lack of support.
And yet, some schools find a way to produce significant proportions of primary care doctors — through recruitment and programs that provide positive experiences and mentors.
U.S. News & World Report recently ranked 168 medical schools by the percentage of graduates who were practicing primary care six to eight years after graduation.
The top 10 schools are all osteopathic medical schools, with 41% to 47% of their students still practicing primary care. Unlike allopathic medical schools, which award MD degrees, osteopathic schools, which award DO degrees, have a history of focusing on primary care and are graduating a growing share of the nation’s primary care physicians.
At the bottom of the U.S. News list is Yale, with 10.7% of its graduates finding lasting careers in primary care. Other elite schools have similar rates: Johns Hopkins, 13.1%; Harvard, 13.7%.
In contrast, public universities that have made it a mission to promote primary care have much higher numbers.
The University of Washington — No. 18 in the ranking, with 36.9% of graduates working in primary care — has a decades-old program placing students in remote parts of Washington, Wyoming, Alaska, Montana, and Idaho. UW recruits students from those areas, and many go back to practice there, with more than 20% of graduates settling in rural communities, according to Joshua Jauregui, assistant dean for clinical curriculum.
Likewise, the University of California-Davis (No. 22, with 36.3% of graduates in primary care) increased the percentage of students choosing family medicine from 12% in 2009 to 18% in 2023, even as it ranks high in specialty training. Programs such as an accelerated three-year primary care “pathway,” which enrolls primarily first-generation college students, help sustain interest in non-specialty medical fields.
The effort starts with recruitment, looking beyond test scores to the life experiences that forge the compassionate, humanistic doctors most needed in primary care, said Mark Henderson, associate dean for admissions and outreach. Most of the students have families who struggle to get primary care, he said. “So they care a lot about it, and it’s not just an intellectual, abstract sense.”
Establishing schools dedicated to primary care, like the one on Long Island, is not a solution in the eyes of some advocates, who consider primary care the backbone of medicine and not a separate discipline. Toyese Oyeyemi Jr., executive director of the Social Mission Alliance at the Fitzhugh Mullan Institute of Health Workforce Equity, worries that establishing such schools might let others “off the hook.”
Still, attending a medical school created to produce primary care doctors worked out well for Lo Cascio. Although she underwent the usual specialty rotations, her passion for pediatrics never flagged — owing to her 23 classmates, two mentors, and her first-year clerkship shadowing a community pediatrician. Now, she’s applying for pediatric residencies.
Lo Cascio also has deep personal reasons: Throughout her experience with a congenital heart condition, her pediatrician was a “guiding light.”
“No matter what else has happened in school, in life, in the world, and medically, your pediatrician is the person that you can come back to,” she said. “What a beautiful opportunity it would be to be that for someone else.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
How to Think More Effectively – by Alain de Botton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our brain is our most powerful organ, and our mind is an astonishing thing. So why do we sometimes go off-piste?
The School of Life‘s Alain de Botton lays out for us a framework of cumulative thinking, directions for effort, and unlikely tools for cognitive improvement.
The book especially highlights the importance of such things as…
- making time for cumulative thinking
- not, however, trying to force it
- working with, rather than in spite of, distractions
- noting and making use of our irrationalities
- taking what we think/do both seriously and lightly, at once
- practising constructive self-doubt
The style is as clear and easy as you may have come to expect from Alain de Botton / The School of Life, and yet, its ideas are still likely to challenge every reader in some (good!) way.
Bottom line: if you would like what you think, say, do to be more meaningful, this book will help you to make the most of your abilities!
Click here to check out How To Think More Effectively, and upgrade your thought processes!
Share This Post
-
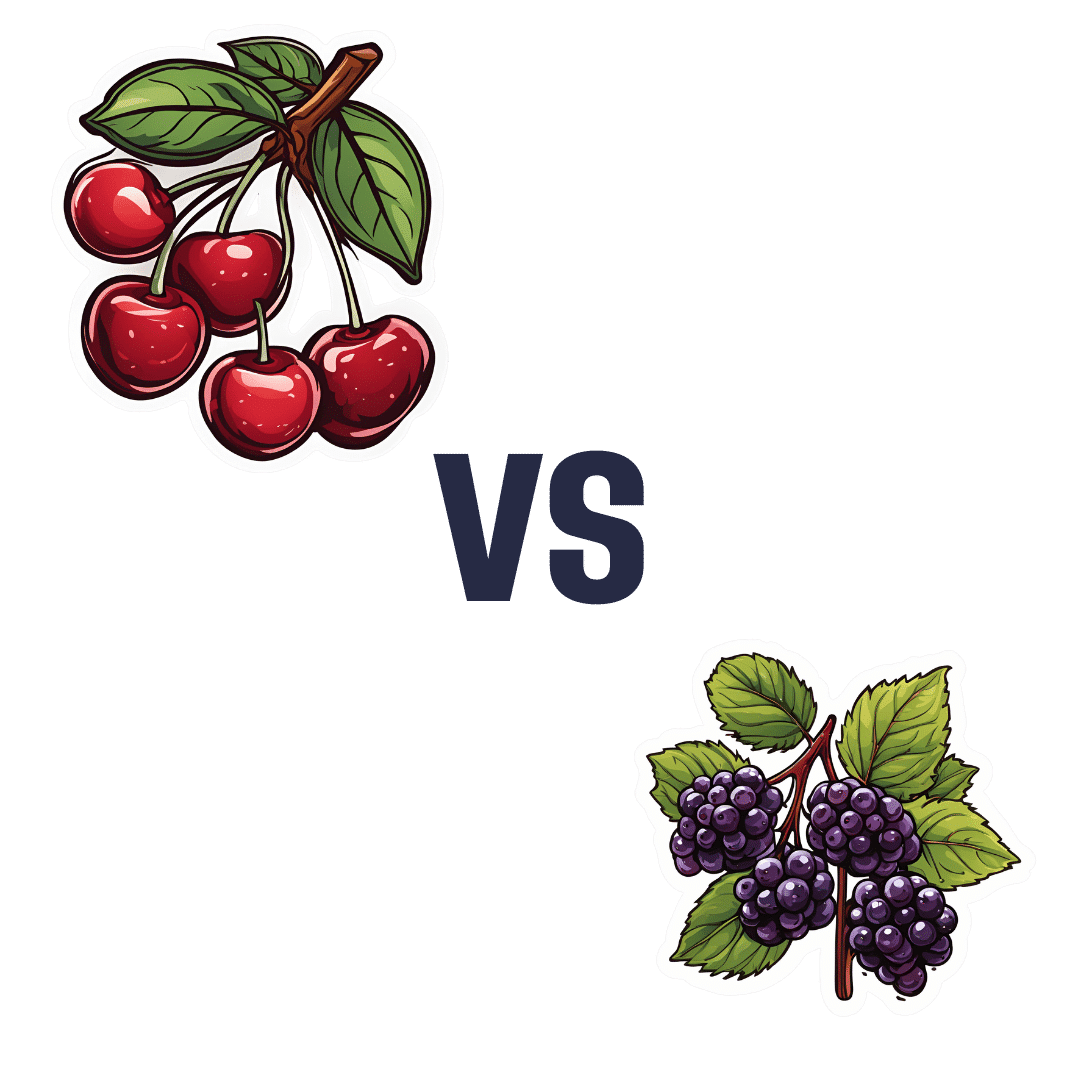
Cherries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to elderberries, we picked the elderberries.
Why?
Both are great! But putting them head-to-head…
In terms of macros, cherries have slightly more protein (but we are talking miniscule numbers here, 0.34mg/100g), while elderberries have moderately more carbs and more than 4x the fiber. This carbs:fiber ratio difference means that elderberries have the lower glycemic index by far, as well as simply more grams/100g fiber, making this an easy win for elderberries.
In the category of vitamins, cherries have more of vitamins A, B9, E, K, and choline, while elderberries have more of vitamins B1, B2, B3, B6, and C. The margins of difference mean that elderberries have the very slightly better overall vitamin coverage, but it’s so slight that we’ll call this a 5:5 tie.
When it comes to minerals, cherries have more copper, magnesium, and manganese, while elderberries have more calcium, iron, phosphorus, potassium, selenium, and zinc. A nice easy win to top it off for elderberries.
On the polyphenols (and other phytochemicals) front, both are great in different ways, nothing that’d we’d consider truly sets one ahead of the other.
All in all, adding up the sections, an overall win for elderberries, but by all means enjoy either or both!
Want to learn more?
You might like to read:
- Cherries’ Very Healthy Wealth Of Benefits!
- Herbs for Evidence-Based Health & Healing ← one of them is elderberry, which hastens recovery from upper respiratory viral infections 😎
Take care!
Share This Post
Related Posts
-
Walnut, Apricot, & Sage Nut Roast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to have at least one good nut roast recipe in your repertoire. It’s something that’s very good for making a good dish out of odds and ends that are in your house, and done well, it’s not only filling and nutritious, but a tasty treat too. Done badly, everyone knows the results can be unfortunate… Making this the perfect way to show off your skills!
You will need
- 1 cup walnuts
- ½ cup almonds
- ¼ cup whole mixed seeds (chia, pumpkin, & poppy are great)
- ¼ cup ground flax (also called flax meal)
- 1 medium onion, finely chopped
- 1 large carrot, grated
- 4 oz dried apricots, chopped
- 3 oz mushrooms, chopped
- 1 oz dried goji berries
- ½ bulb garlic, crushed
- 2 tbsp fresh sage, chopped
- 1 tbsp nutritional yeast
- 2 tsp dried rosemary
- 2 tsp dried thyme
- 2 tsp black pepper, coarse ground
- 1 tsp yeast extract (even if you don’t like it; trust us; it will work) dissolved in ¼ cup hot water
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃, and line a 2 lb loaf tin with baking paper.
2) Heat some oil in a skillet over a moderate heat, and fry the onion for a few minutes until translucent. Add the garlic, carrot, and mushrooms, cooking for another 5 minutes, stirring well. Set aside to cool a little once done.
3) Process the nuts in a food processor, pulsing until they are well-chopped but not so much that they turn into flour.
4) Combine the nuts, vegetables, and all the other ingredients in a big bowl, and mix thoroughly. If it doesn’t have enough structural integrity to be thick and sticky and somewhat standing up by itself if you shape it, add more ground flax. If it is too dry, add a little water but be sparing.
5) Spoon the mixture into the loaf tin, press down well (or else it will break upon removal), cover with foil and bake for 30 minutes. Remove the foil, and bake for a further 15 minutes, until firm and golden. When done, allow it to rest in the tin for a further 15 minutes, before turning it out.
6) Serve, as part of a roast dinner (roast potatoes, vegetables, gravy, etc).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Chia Seeds vs Pumpkin Seeds – Which is Healthier?
- Apricots vs Peaches – Which is Healthier?
- Goji Berries: Which Benefits Do They Really Have?
- Ergothioneine: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Caramelized Caraway Cabbage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cabbage is an underrated vegetable for its many nutrients and its culinary potential—here’s a great way to make it a delectable starter or respectable side.
You will need
- 1 medium white cabbage, sliced into 1″ thick slabs
- 1 tbsp extra-virgin olive oil
- 1 tbsp caraway seeds
- 1 tsp black pepper
- ½ tsp turmeric
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the non-cabbage ingredients in a small bowl, whisking to mix thoroughly—with a tiny whisk if you have one, but a fork will work if necessary.
3) Arrange the cabbage slices on a lined baking tray and brush the seasoning-and-oil mixture over both sides of each slice.
4) Roast for 20–25 minutes until the cabbage is tender and beginning to caramelize.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Curcumin (Turmeric) is worth its weight in gold
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Does One Test Acupuncture Against Placebo Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pinpointing The Usefulness Of Acupuncture
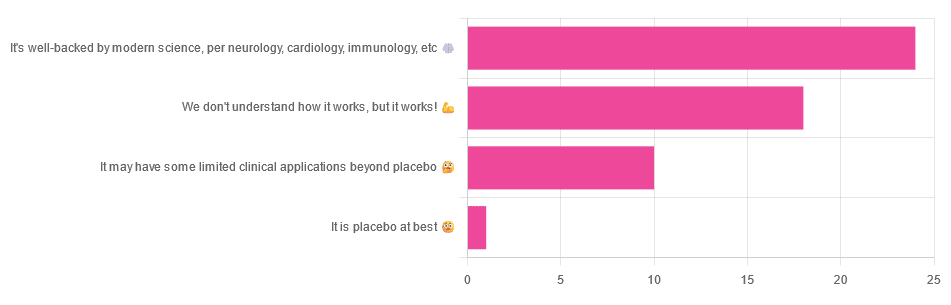
We asked you for your opinions on acupuncture, and got the above-depicted, below-described, set of answers:
- A little under half of all respondents voted for “It’s well-backed by modern science, per neurology, cardiology, immunology, etc”
- Slightly fewer respondents voted for “We don’t understand how it works, but it works!”
- A little under a fifth of respondents voted for “It may have some limited clinical applications beyond placebo”
- One (1) respondent voted for for “It’s placebo at best”
When we did a main feature about homeopathy, a couple of subscribers wrote to say that they were confused as to what homeopathy was, so this time, we’ll start with a quick definition first.
First, what is acupuncture? For the convenience of a quick definition so that we can move on to the science, let’s borrow from Wikipedia:
❝Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine in which thin needles are inserted into the body.
Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.❞
Now, that’s not a promising start, but we will not be deterred! We will instead examine the science itself, rather than relying on tertiary sources like Wikipedia.
It’s worth noting before we move on, however, that there is vigorous debate behind the scenes of that article. The gist of the argument is:
- On one side: “Acupuncture is not pseudoscience/quackery! This has long been disproved and there are peer-reviewed research papers on the subject.”
- On the other: “Yes, but only in disreputable quack journals created specifically for that purpose”
The latter counterclaim is a) potentially a “no true Scotsman” rhetorical ploy b) potentially true regardless
Some counterclaims exhibit specific sinophobia, per “if the source is Chinese, don’t believe it”. That’s not helpful either.
Well, the waters sure are muddy. Where to begin? Let’s start with a relatively easy one:
It may have some clinical applications beyond placebo: True or False?
True! Admittedly, “may” is doing some of the heavy lifting here, but we’ll take what we can get to get us going.
One of the least controversial uses of acupuncture is to alleviate chronic pain. Dr. Vickers et al, in a study published under the auspices of JAMA (a very respectable journal, and based in the US, not China), found:
❝Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.
However, these differences are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to the therapeutic effects of acupuncture❞
Source: Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis
If you’re feeling sharp today, you may be wondering how the differences are described as “significant” and “relatively modest” in the same text. That’s because these words have different meanings in academic literature:
- Significant = p<0.05, where p is the probability of the achieved results occurring randomly
- Modest = the differences between the test group and the control group were small
In other words, “significant modest differences” means “the sample sizes were large, and the test group reliably got slightly better results than placebo”
We don’t understand how it works, but it works: True or False
Broadly False. When it works, we generally have an idea how.
Placebo is, of course, the main explanation. And even in examples such as the above, how is placebo acupuncture given?
By inserting acupuncture needles off-target rather than in accord with established meridians and points (the lines and dots that, per Traditional Chinese Medicine, indicate the flow of qi, our body’s vital energy, and welling-points of such).
So, if a patient feels that needles are being inserted randomly, they may no longer have the same confidence that they aren’t in the control group receiving placebo, which could explain the “modest” difference, without there being anything “to” acupuncture beyond placebo. After all, placebo works less well if you believe you are only receiving placebo!
Indeed, a (Korean, for the record) group of researchers wrote about this—and how this confounding factor cuts both ways:
❝Given the current research evidence that sham acupuncture can exert not only the originally expected non-specific effects but also sham acupuncture-specific effects, it would be misleading to simply regard sham acupuncture as the same as placebo.
Therefore, researchers should be cautious when using the term sham acupuncture in clinical investigations.❞
Source: Sham Acupuncture Is Not Just a Placebo
It’s well-backed by modern science, per neurology, cardiology, immunology, etc: True or False?
False, for the most part.
While yes, the meridians and points of acupuncture charts broadly correspond to nerves and vasculature, there is no evidence that inserting needles into those points does anything for one’s qi, itself a concept that has not made it into Western science—as a unified concept, anyway…
Note that our bodies are indeed full of energy. Electrical energy in our nerves, chemical energy in every living cell, kinetic energy in all our moving parts. Even, to stretch the point a bit, gravitational potential energy based on our mass.
All of these things could broadly be described as qi, if we so wish. Indeed, the ki in the Japanese martial art of aikido is the latter kinds; kinetic energy and gravitational potential energy based on our mass. Same goes, therefore for the ki in kiatsu, a kind of Japanese massage, while the ki in reiki, a Japanese spiritual healing practice, is rather more mystical.
The qi in Chinese qigong is mostly about oxygen, thus indirectly chemical energy, and the electrical energy of the nerves that are receiving oxygenated blood at higher or lower levels.
On the other hand, the efficacy of the use of acupuncture for various kinds of pain is well-enough evidenced. Indeed, even the UK’s famously thrifty NHS (that certainly would not spend money on something it did not find to work) offers it as a complementary therapy for some kinds of pain:
❝Western medical acupuncture (dry needling) is the use of acupuncture following a medical diagnosis. It involves stimulating sensory nerves under the skin and in the muscles.
This results in the body producing natural substances, such as pain-relieving endorphins. It’s likely that these naturally released substances are responsible for the beneficial effects experienced with acupuncture.❞
Source: NHS | Acupuncture
Meanwhile, the NIH’s National Cancer Institute recommends it… But not as a cancer treatment.
Rather, they recommend it as a complementary therapy for pain management, and also against nausea, for which there is also evidence that it can help.
Frustratingly, while they mention that there is lots of evidence for this, they don’t actually link the studies they’re citing, or give enough information to find them. Instead, they say things like “seven randomized clinical trials found that…” and provide links that look reassuring until one finds, upon clicking on them, that it’s just a link to the definition of “randomized clinical trial”:
Source: NIH | Nactional Cancer Institute | Acupuncture (PDQ®)–Patient Version
However, doing our own searches finds many studies (mostly in specialized, potentially biased, journals such as the Journal of Acupuncture and Meridian Studies) finding significant modest outperformance of [what passes for] placebo.
Sometimes, the existence of papers with promising titles, and statements of how acupuncture might work for things other than relief of pain and nausea, hides the fact that the papers themselves do not, in fact, contain any evidence to support the hypothesis. Here’s an example:
❝The underlying mechanisms behind the benefits of acupuncture may be linked with the regulation of the hypothalamic-pituitary-gonadal (adrenal) axis and activation of the Wnt/β-catenin and OPG/RANKL/RANK signaling pathways.
In summary, strong evidence may still come from prospective and well-designed clinical trials to shed light on the potential role of acupuncture in preserving bone loss❞
Source: Acupuncture for Osteoporosis: a Review of Its Clinical and Preclinical Studies
So, here they offered a very sciencey hypothesis, and to support that hypothesis, “strong evidence may still come”.
“We must keep faith” is not usually considered evidence worthy of inclusion in a paper!
PS: the above link is just to the abstract, because the “Full Text” link offered in that abstract leads to a completely unrelated article about HIV/AIDS-related cryptococcosis, in a completely different journal, nothing to do with acupuncture or osteoporosis).
Again, this is not the kind of professionalism we expect from peer-reviewed academic journals.
Bottom line:
Acupuncture reliably performs slightly better than sham acupuncture for the management of pain, and may also help against nausea.
Beyond placebo and the stimulation of endorphin release, there is no consistently reliable evidence that is has any other discernible medical effect by any mechanism known to Western science—though there are plenty of hypotheses.
That said, absence of evidence is not evidence of absence, and the logistical difficulty of testing acupuncture against placebo makes for slow research. Maybe one day we’ll know more.
For now:
- If you find it helps you: great! Enjoy
- If you think it might help you: try it! By a licensed professional with a good reputation, please.
- If you are not inclined to having needles put in you unnecessarily: skip it! Extant science suggests that at worst, you’ll be missing out on slight relief of pain/nausea.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: