Caramelized Caraway Cabbage
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cabbage is an underrated vegetable for its many nutrients and its culinary potential—here’s a great way to make it a delectable starter or respectable side.
You will need
- 1 medium white cabbage, sliced into 1″ thick slabs
- 1 tbsp extra-virgin olive oil
- 1 tbsp caraway seeds
- 1 tsp black pepper
- ½ tsp turmeric
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the non-cabbage ingredients in a small bowl, whisking to mix thoroughly—with a tiny whisk if you have one, but a fork will work if necessary.
3) Arrange the cabbage slices on a lined baking tray and brush the seasoning-and-oil mixture over both sides of each slice.
4) Roast for 20–25 minutes until the cabbage is tender and beginning to caramelize.
5) Serve warm.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Curcumin (Turmeric) is worth its weight in gold
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kiwi vs Lemon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to lemon, we picked the kiwi.
Why?
A fairly straightforward one today!
In terms of macros, kiwi has more protein, carbs, and fiber, the ratio of the latter two also giving it the lower glycemic index. An easy win for kiwi here.
In the category of vitamins, kiwi has more of vitamins A, B2, B3, B9, C, E, K, and choline, while lemon has more of vitamins B1 and B6. Yes, that’s right, lemon didn’t even win on the vitamin C that it’s famous for. In any case, a clear 8:2 win for kiwi.
Looking at minerals, kiwi has more calcium, copper, magnesium, manganese, phosphorus, potassium, and zinc, while lemon has more iron and selenium. So, looking at this 7:2 win for kiwi, you might want to reconsider that “glass of lemon water to replenish minerals” trend!
None of this is to knock lemons, by the way; lemons are still a very respectable fruit, nutritionally. Probably very few people are out there eating lemons the way one might eat kiwi…
(writer’s note: I say “very few”, as once upon a time when my son was small, I remember coming into the kitchen to find he had helped himself to lemon wedges and was just eating them, so it can happen. But I also one time when he was just as small, found him drinking hot sauce directly from the bottle, so hey, he clearly already enjoyed strong flavors. Lest I seem a very inattentive mother, I’ll say in my defense that our kitchen has no real toddler-height hazards when the oven is cold, and those items were from the bottom of the fridge, so easy to access if I leave the room for a moment to grab something)
…but what we do want to say here is: if you don’t care for lemons so much, you’re not missing out. If the lemon water isn’t calling to you, you can skip it guilt-free.
In any case, do enjoy either or both, but kiwi’s the clear winner here!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list! It has some cool properties, as you’ll see, killing cancer cells while sparing healthy ones.
Take care!
Share This Post
-
The Sprout Book – by Doug Evans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sprouting seeds are more nutritious than most people think, and “seeds” is also a much broader category than people think. Beyond even chia and sunflower and such, this book bids us remember that onions do not just appear on supermarket shelves fully formed (to give just one example of many); most plants come from seeds and of those, most can be usefully sprouted.
The author, most well-known for his tech companies, here is selling us a very low-tech health kick with very little profit to be found except for our health. By sprouting seeds of many kinds at home, we can enjoy powerful superfoods that are not only better than, but also cheaper than, most supplements.
Nor are the benefits of sprouting things marginal; we’re not talking about a 1–10% increase in bioavailable so much as what’s often a 100–1000% increase.
After explaining the science and giving a primer on sprouting things for oneself, there is a wide selection of recipes, but the biggest benefit of the book is in just getting the reader up-and-running with at-home sprouting.
Bottom line: if you like the idea of letting food be your medicine and even like the idea of essentially growing your own food with zero gardening skills, then this is an excellent book for you.
Share This Post
-
We looked at genetic clues to depression in more than 14,000 people. What we found may surprise you
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The core experiences of depression – changes in energy, activity, thinking and mood – have been described for more than 10,000 years. The word “depression” has been used for about 350 years.
Given this long history, it may surprise you that experts don’t agree about what depression is, how to define it or what causes it.
But many experts do agree that depression is not one thing. It’s a large family of illnesses with different causes and mechanisms. This makes choosing the best treatment for each person challenging.
Reactive vs endogenous depression
One strategy is to search for sub-types of depression and see whether they might do better with different kinds of treatments. One example is contrasting “reactive” depression with “endogenous” depression.
Reactive depression (also thought of as social or psychological depression) is presented as being triggered by exposure to stressful life events. These might be being assaulted or losing a loved one – an understandable reaction to an outside trigger.
Endogenous depression (also thought of as biological or genetic depression) is proposed to be caused by something inside, such as genes or brain chemistry.
Many people working clinically in mental health accept this sub-typing. You might have read about this online.
But we think this approach is way too simple.
While stressful life events and genes may, individually, contribute to causing depression, they also interact to increase the risk of someone developing depression. And evidence shows that there is a genetic component to being exposed to stressors. Some genes affect things such as personality. Some affect how we interact with our environments.
What we did and what we found
Our team set out to look at the role of genes and stressors to see if classifying depression as reactive or endogenous was valid.
In the Australian Genetics of Depression Study, people with depression answered surveys about exposure to stressful life events. We analysed DNA from their saliva samples to calculate their genetic risk for mental disorders.
Our question was simple. Does genetic risk for depression, bipolar disorder, schizophrenia, ADHD, anxiety and neuroticism (a personality trait) influence people’s reported exposure to stressful life events?
We looked at the genetic risk of mental illness to see how that was linked to stressful life events, such as childhood abuse and neglect. Kamira/Shutterstock You may be wondering why we bothered calculating the genetic risk for mental disorders in people who already have depression. Every person has genetic variants linked to mental disorders. Some people have more, some less. Even people who already have depression might have a low genetic risk for it. These people may have developed their particular depression from some other constellation of causes.
We looked at the genetic risk of conditions other than depression for a couple of reasons. First, genetic variants linked to depression overlap with those linked to other mental disorders. Second, two people with depression may have completely different genetic variants. So we wanted to cast a wide net to look at a wider spectrum of genetic variants linked to mental disorders.
If reactive and endogenous depression sub-types are valid, we’d expect people with a lower genetic component to their depression (the reactive group) would report more stressful life events. And we’d expect those with a higher genetic component (the endogenous group) would report fewer stressful life events.
But after studying more than 14,000 people with depression we found the opposite.
We found people at higher genetic risk for depression, anxiety, ADHD or schizophrenia say they’ve been exposed to more stressors.
Assault with a weapon, sexual assault, accidents, legal and financial troubles, and childhood abuse and neglect, were all more common in people with a higher genetic risk of depression, anxiety, ADHD or schizophrenia.
These associations were not strongly influenced by people’s age, sex or relationships with family. We didn’t look at other factors that may influence these associations, such as socioeconomic status. We also relied on people’s memory of past events, which may not be accurate.
How do genes play a role?
Genetic risk for mental disorders changes people’s sensitivity to the environment.
Imagine two people, one with a high genetic risk for depression, one with a low risk. They both lose their jobs. The genetically vulnerable person experiences the job loss as a threat to their self-worth and social status. There is a sense of shame and despair. They can’t bring themselves to look for another job for fear of losing it too. For the other, the job loss feels less about them and more about the company. These two people internalise the event differently and remember it differently.
Genetic risk for mental disorders also might make it more likely people find themselves in environments where bad things happen. For example, a higher genetic risk for depression might affect self-worth, making people more likely to get into dysfunctional relationships which then go badly.
If two people lose their jobs, one with a high genetic risk of depression the other at low risk, both will experience and remember the event differently. Inside Creative House/Shutterstock What does our study mean for depression?
First, it confirms genes and environments are not independent. Genes influence the environments we end up in, and what then happens. Genes also influence how we react to those events.
Second, our study doesn’t support a distinction between reactive and endogenous depression. Genes and environments have a complex interplay. Most cases of depression are a mix of genetics, biology and stressors.
Third, people with depression who appear to have a stronger genetic component to their depression report their lives are punctuated by more serious stressors.
So clinically, people with higher genetic vulnerability might benefit from learning specific techniques to manage their stress. This might help some people reduce their chance of developing depression in the first place. It might also help some people with depression reduce their ongoing exposure to stressors.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jacob Crouse, Research Fellow in Youth Mental Health, Brain and Mind Centre, University of Sydney and Ian Hickie, Co-Director, Health and Policy, Brain and Mind Centre, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Chickpeas vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to pinto beans, we picked the pinto beans.
Why?
Both are great! And an argument could be made for either…
In terms of macros, pinto beans have slightly more fiber and slightly more protein, while chickpeas have slightly more carbs, and thus predictably higher net carbs. In the category of those proteins, they both have a comparable spread of amino acods, with pinto beans having very slightly more of each amino acid. All this adds up to a clear, but moderate, win for pinto beans.
When it comes to vitamins, technically chickpeas have more of vitamins A, B3, B5, C, K, and choline, but the margins are so small as to be almost meaningless. Meanwhile, pinto beans have more of vitamins B1, B6, and E, and/but the only one where the margin is enough to really care about is vitamin E (a little over 2x what chickpeas have). So, an argument could be made either way, but we’re going to call this category a tie.
The story with minerals is similar; chickpeas have more copper, iron, manganese, phosphorus, and zinc, all with small margins, while pinto beans have more potassium and selenium, and/but also less sodium. We’d call this either a tie, or a very slight win for chickpeas.
Adding up the sections gives for a very modest win for pinto beans, but as we say, an argument could be made for either.
Certainly, enjoy both!
Want to learn more?
You might like to read:
- Chickpeas vs Black Beans – Which is Healthier?
- Kidney Beans vs Fava Beans – Which is Healthier?
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
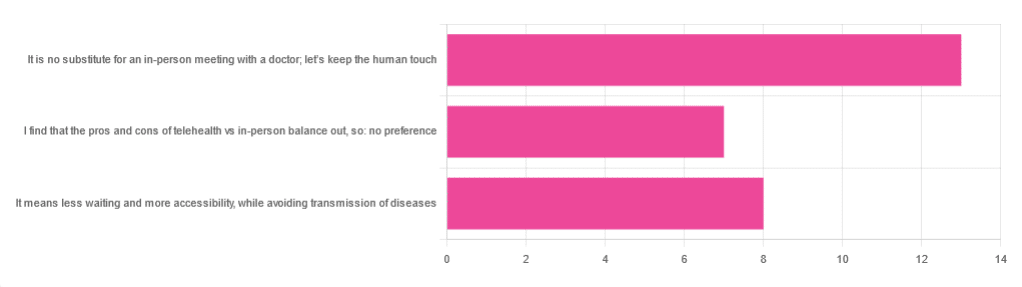
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Origin of Everyday Moods – by Dr. Robert Thayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First of all, what does this title mean by “everyday moods”? By this the author is referring to the kinds of moods we have just as a matter of the general wear-and-tear of everyday life—not the kind that come from major mood disorders and/or serious trauma.
The latter kinds of mood take less explaining, in any case. Dr. Thayer, therefore, spends his time on the less obvious ones—which in turn are the ones that affect most of the most, every day.
Critical to Dr. Thayer’s approach is the mapping of moods by four main quadrants:
- High energy, high tension
- High energy, low tension
- Low energy, high tension
- Low energy, low tension
…though this can be further divided into 25 sectors, if we rate each variable on a scale of 0–4. But for the first treatment, it suffices to look at whether energy and tension are high or low, respectively, and which we’d like to have more or less of.
Then (here be science) how to go about achieving that in the most efficient, evidence-based ways. So, it’s not just a theoretical book; it has great practical value too.
The style of the book is accessible, and walks a fine line between pop-science and hard science, which makes it a great book for laypersons and academics alike.
Bottom line: if you’d like the cheat codes to improve your moods and lessen the impact of bad ones, this is the book for you.
Click here to check out The Origin of Everyday Moods, and manage yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: