Cannabis & Heart Attacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many, cannabis use has taken the place that alcohol used to have when it comes to wanting a “downer”, that is to say, a drug that relaxes us as opposed to stimulating us.
Indeed, it is generally considered safer than alcohol ← however this is not a strong claim, because alcohol is much more dangerous than one would think given its ubiquity and (in many places, at least) social acceptability.
We’ve talked a bit about cannabis use before, in its various forms, for example:
Cannabis Myths vs Reality ← a very good starting point for the curious
And one specifically about the use of THC gummies (THC is the psychoactive compound in cannabis, i.e. it’s the chemical that gets people high, as opposed to CBD, which is not psychoactive) as a sleep aid:
Sweet Dreams Are Made of THC (Or Are They?)
And for those skipping the THC, we’ve also written about CBD use, including:
CBD Oil: What Does The Science Say? and Do CBD Gummies Work?
So, about cannabis and heart attacks
Alcohol is a relaxant, and yet it can contribute to heart disease (amongst many other things, of course):
Can We Drink To Good Health? ← this is mostly about red wine’s putative heart health benefits, how the idea got popularized, and how it doesn’t stand up to scrutiny when actually looking at the evidence.
And cannabis, another relaxant? Not so good either!
New research has shown that cannabis users have a higher risk of heart attacks, even among younger and otherwise healthy individuals. This is based on analyzing data from 4,636,628 relatively healthy adults.
Specifically, the data showed that even young healthy cannabis users get:
- Sixfold increased risk of heart attack
- Fourfold increased risk of ischemic stroke
- Threefold increased risk of cardiovascular death, heart attack, or stroke
We mention the otherwise “relatively healthy” nature of the participants, because it’s important to note that less healthy people (who were perhaps using cannabis to self-medicate for some serious condition) were not included in the dataset, as it’d skew the data unhelpfully and it’d make the risk look a lot higher than the risk levels we mentioned above.
The mechanisms by which cannabis affects heart health are not fully understood, but hypotheses include:
- Disrupting heart rhythm regulation
- Increasing oxygen demand in the heart muscle
- Causing endothelial dysfunction, which affects blood vessel function
Further, heart attack risk peaked one hour after cannabis use, and while this doesn’t prove causality, it certainly doesn’t make cannabis look safe.
You can read the paper in its entirety here:
Want a safer way to relax?
We recommend:
- No-Frills, Evidence-Based Mindfulness
- Meditation Games That You’ll Actually Enjoy
- Which Style Of Yoga Is Best For You?
- 7 Kinds Of Rest When Sleep Is Not Enough
- Better Sex = Longer Life (Here’s How)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could Just Two Hours Sleep Per Day Be Enough?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Polyphasic Sleep… Super-Schedule Or An Idea Best Put To Rest?
What is it?
Let’s start by defining some terms:
- Monophasic sleep—sleeping in one “chunk” per day. For example, a good night’s “normal” sleep.
- Biphasic sleep—sleeping in two “chunks” per day. Typically, a shorter night’s sleep, with a nap usually around the middle of the day / early afternoon.
- Polyphasic sleep—sleeping in two or more “chunks per day”. Some people do this in order to have more hours awake per day, to do things. The idea is that sleeping this way is more efficient, and one can get enough rest in less time. The most popular schedules used are:
- The Überman schedule—six evenly-spaced 20-minute naps, one every four hours, throughout the 24-hour day. The name is a semi-anglicized version of the German word Übermensch, “Superman”.
- The Everyman schedule—a less extreme schedule, that has a three-hours “long sleep” during the night, and three evenly-spaced 20-minute naps during the day, for a total of 4 hours sleep.
There are other schedules, but we’ll focus on the most popular ones here.
Want to learn about the others? Visit: Polyphasic.Net (a website by and for polyphasic sleep enthusiasts)
Some people have pointed to evidence that suggests humans are naturally polyphasic sleepers, and that it is only modern lifestyles that have forced us to be (mostly) monophasic.
There is at least some evidence to suggest that when environmental light/dark conditions are changed (because of extreme seasonal variation at the poles, or, as in this case, because of artificial changes as part of a sleep science experiment), we adjust our sleeping patterns accordingly.
The counterpoint, of course, is that perhaps when at the mercy of long days/nights at the poles, or no air-conditioning to deal with the heat of the day in the tropics, that perhaps we were forced to be polyphasic, and now, with modern technology and greater control, we are free to be monophasic.
Either way, there are plenty of people who take up the practice of polyphasic sleep.
Ok, But… Why?
The main motivation for trying polyphasic sleep is simply to have more hours in the day! It’s exciting, the prospect of having 22 hours per day to be so productive and still have time over for leisure.
A secondary motivation for trying polyphasic sleep is that when the brain is sleep-deprived, it will prioritize REM sleep. Here’s where the Überman schedule becomes perhaps most interesting:
The six evenly-spaced naps of the Überman schedule are each 20 minutes long. This corresponds to the approximate length of a normal REM cycle.
Consequently, when your head hits the pillow, you’ll immediately begin dreaming, and at the end of your dream, the alarm will go off.
Waking up at the end of a dream, when one hasn’t yet entered a non-REM phase of sleep, will make you more likely to remember it. Similarly, going straight into REM sleep will make you more likely to be aware of it, thus, lucid dreaming.
Read: Sleep fragmentation and lucid dreaming (actually a very interesting and informative lucid dreaming study even if you don’t want to take up polyphasic sleep)
Six 20-minute lucid-dreaming sessions per day?! While awake for the other 22 hours?! That’s… 24 hours per day of wakefulness to use as you please! What sorcery is this?
Hence, it has quite an understandable appeal.
Next Question: Does it work?
Can we get by without the other (non-REM) kinds of sleep?
According to Überman cycle enthusiasts: Yes! The body and brain will adapt.
According to sleep scientists: No! The non-REM slow-wave phases of sleep are essential
Read: Adverse impact of polyphasic sleep patterns in humans—Report of the National Sleep Foundation sleep timing and variability consensus panel
(if you want to know just how bad it is… the top-listed “similar article” is entitled “Suicidal Ideation”)
But what about, for example, the Everman schedule? Three hours at night is enough for some non-REM sleep, right?
It is, and so it’s not as quickly deleterious to the health as the Überman schedule. But, unless you are blessed with rare genes that allow you to operate comfortably on 4 hours per day (you’ll know already if that describes you, without having to run any experiment), it’s still bad.
Adults typically need 7–9 hours of sleep per night, and if you don’t get it, you’ll accumulate a sleep debt. And, importantly:
When you accumulate sleep debt, you are borrowing time at a very high rate of interest!
And, at risk of laboring the metaphor, but this is important too:
Not only will you have to pay it back soon (with interest), you will be hounded by the debt collection agents—decreased cognitive ability and decreased physical ability—until you pay up.
In summary:
- Polyphasic sleep is really very tempting
- It will give you more hours per day (for a while)
- It will give the promised lucid dreaming benefits (which is great until you start micronapping between naps, this is effectively a mini psychotic break from reality lasting split seconds each—can be deadly if behind the wheel of a car, for instance!)
- It is unequivocally bad for the health and we do not recommend it
Bottom line:
Some of the claimed benefits are real, but are incredibly short-term, unsustainable, and come at a cost that’s far too high. We get why it’s tempting, but ultimately, it’s self-sabotage.
(Sadly! We really wanted it to work, too…)
Share This Post
-
Health Care AI, Intended To Save Money, Turns Out To Require a Lot of Expensive Humans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Preparing cancer patients for difficult decisions is an oncologist’s job. They don’t always remember to do it, however. At the University of Pennsylvania Health System, doctors are nudged to talk about a patient’s treatment and end-of-life preferences by an artificially intelligent algorithm that predicts the chances of death.
But it’s far from being a set-it-and-forget-it tool. A routine tech checkup revealed the algorithm decayed during the covid-19 pandemic, getting 7 percentage points worse at predicting who would die, according to a 2022 study.
There were likely real-life impacts. Ravi Parikh, an Emory University oncologist who was the study’s lead author, told KFF Health News the tool failed hundreds of times to prompt doctors to initiate that important discussion — possibly heading off unnecessary chemotherapy — with patients who needed it.
He believes several algorithms designed to enhance medical care weakened during the pandemic, not just the one at Penn Medicine. “Many institutions are not routinely monitoring the performance” of their products, Parikh said.
Algorithm glitches are one facet of a dilemma that computer scientists and doctors have long acknowledged but that is starting to puzzle hospital executives and researchers: Artificial intelligence systems require consistent monitoring and staffing to put in place and to keep them working well.
In essence: You need people, and more machines, to make sure the new tools don’t mess up.
“Everybody thinks that AI will help us with our access and capacity and improve care and so on,” said Nigam Shah, chief data scientist at Stanford Health Care. “All of that is nice and good, but if it increases the cost of care by 20%, is that viable?”
Government officials worry hospitals lack the resources to put these technologies through their paces. “I have looked far and wide,” FDA Commissioner Robert Califf said at a recent agency panel on AI. “I do not believe there’s a single health system, in the United States, that’s capable of validating an AI algorithm that’s put into place in a clinical care system.”
AI is already widespread in health care. Algorithms are used to predict patients’ risk of death or deterioration, to suggest diagnoses or triage patients, to record and summarize visits to save doctors work, and to approve insurance claims.
If tech evangelists are right, the technology will become ubiquitous — and profitable. The investment firm Bessemer Venture Partners has identified some 20 health-focused AI startups on track to make $10 million in revenue each in a year. The FDA has approved nearly a thousand artificially intelligent products.
Evaluating whether these products work is challenging. Evaluating whether they continue to work — or have developed the software equivalent of a blown gasket or leaky engine — is even trickier.
Take a recent study at Yale Medicine evaluating six “early warning systems,” which alert clinicians when patients are likely to deteriorate rapidly. A supercomputer ran the data for several days, said Dana Edelson, a doctor at the University of Chicago and co-founder of a company that provided one algorithm for the study. The process was fruitful, showing huge differences in performance among the six products.
It’s not easy for hospitals and providers to select the best algorithms for their needs. The average doctor doesn’t have a supercomputer sitting around, and there is no Consumer Reports for AI.
“We have no standards,” said Jesse Ehrenfeld, immediate past president of the American Medical Association. “There is nothing I can point you to today that is a standard around how you evaluate, monitor, look at the performance of a model of an algorithm, AI-enabled or not, when it’s deployed.”
Perhaps the most common AI product in doctors’ offices is called ambient documentation, a tech-enabled assistant that listens to and summarizes patient visits. Last year, investors at Rock Health tracked $353 million flowing into these documentation companies. But, Ehrenfeld said, “There is no standard right now for comparing the output of these tools.”
And that’s a problem, when even small errors can be devastating. A team at Stanford University tried using large language models — the technology underlying popular AI tools like ChatGPT — to summarize patients’ medical history. They compared the results with what a physician would write.
“Even in the best case, the models had a 35% error rate,” said Stanford’s Shah. In medicine, “when you’re writing a summary and you forget one word, like ‘fever’ — I mean, that’s a problem, right?”
Sometimes the reasons algorithms fail are fairly logical. For example, changes to underlying data can erode their effectiveness, like when hospitals switch lab providers.
Sometimes, however, the pitfalls yawn open for no apparent reason.
Sandy Aronson, a tech executive at Mass General Brigham’s personalized medicine program in Boston, said that when his team tested one application meant to help genetic counselors locate relevant literature about DNA variants, the product suffered “nondeterminism” — that is, when asked the same question multiple times in a short period, it gave different results.
Aronson is excited about the potential for large language models to summarize knowledge for overburdened genetic counselors, but “the technology needs to improve.”
If metrics and standards are sparse and errors can crop up for strange reasons, what are institutions to do? Invest lots of resources. At Stanford, Shah said, it took eight to 10 months and 115 man-hours just to audit two models for fairness and reliability.
Experts interviewed by KFF Health News floated the idea of artificial intelligence monitoring artificial intelligence, with some (human) data whiz monitoring both. All acknowledged that would require organizations to spend even more money — a tough ask given the realities of hospital budgets and the limited supply of AI tech specialists.
“It’s great to have a vision where we’re melting icebergs in order to have a model monitoring their model,” Shah said. “But is that really what I wanted? How many more people are we going to need?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Buckwheat vs Bulgur Wheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing buckwheat to bulgur, we picked the buckwheat.
Why?
First, some things to know up front:
- Bulgur wheat is a kind of cracked wheat product. As such, it contains wheat, and yes, gluten.
- Buckwheat is not a wheat, nor even a grass, but a flowering plant. Buckwheat is as related to wheat as a lionfish is to a lion. It does not contain gluten.
- Buckwheat can be purchased whole or hulled. We went with whole. If you go with hulled, the percentages of vitamins and minerals will be relatively higher, and/but this will be because you lost the fibrous husk, so they’ll be commensurately lower in fiber. If you were to go with hulled, we’d still pick it over bulgur wheat though, just for a different reason (as in that case, the vitamin and mineral contents would be more overwhelmingly in buckwheat’s favor, even though it’d have less fiber).
Ok, now that those things are covered…
Looking at the macronutrients, there’s not a lot between them, except that buckwheat has the much lower glycemic index (this is only the case if you got whole, not hulled—if you got hulled, the glycemic index would be about the same).
In terms of vitamins, buckwheat has more of vitamins B2, B5, B9, E, K, and choline, while bulgur wheat technically has more vitamin A, but the numbers are tiny; a cup of bulgur wheat will give you 0.12% of the RDA. So, an easy win (functionally: 5:0) for buckwheat.
When it comes to minerals, buckwheat has more copper, magnesium, potassium, and selenium, while bulgur wheat has more calcium and manganese. They’re equal on iron and phosphorus, making this a 4:2 win for buckwheat.
Adding up the categories makes this a clear win for buckwheat!
Want to learn more?
You might like to read:
Take care!
Share This Post
Related Posts
-
The Brain Health Book – by Dr. John Randolph
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a clinical neuropsychologist and brain health consultant, brings his professional knowledge and understanding to bear on the questions of what works, what doesn’t, and why?
In practical terms, the focus is mostly on maintaining/improving attention, memory, and executive functions. To that end, he covers what kinds of exercises to do (physical and mental!), and examines what strategies make the most difference—including the usual lifestyle considerations of course, but also more specifically than that, what to prioritize over what when it comes to daily choices.
The style is easy pop-science, with an emphasis on being directly useful to the reader, rather than giving an overabundance of citations for everything as we go along. He does, however, explain the necessary science as we go, making the book educational without being academic.
Bottom line: if you’d like to maintain/improve your brain, this book can certainly help with that, and as a bonus (unless you are already an expert) you’ll learn plenty about the brain as you go.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
In Vermont, Where Almost Everyone Has Insurance, Many Can’t Find or Afford Care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
RICHMOND, Vt. — On a warm autumn morning, Roger Brown walked through a grove of towering trees whose sap fuels his maple syrup business. He was checking for damage after recent flooding. But these days, his workers’ health worries him more than his trees’.
The cost of Slopeside Syrup’s employee health insurance premiums spiked 24% this year. Next year it will rise 14%.
The jumps mean less money to pay workers, and expensive insurance coverage that doesn’t ensure employees can get care, Brown said. “Vermont is seen as the most progressive state, so how is health care here so screwed up?”
Vermont consistently ranks among the healthiest states, and its unemployment and uninsured rates are among the lowest. Yet Vermonters pay the highest prices nationwide for individual health coverage, and state reports show its providers and insurers are in financial trouble. Nine of the state’s 14 hospitals are losing money, and the state’s largest insurer is struggling to remain solvent. Long waits for care have become increasingly common, according to state reports and interviews with residents and industry officials.
Rising health costs are a problem across the country, but Vermont’s situation surprises health experts because virtually all its residents have insurance and the state regulates care and coverage prices.
For more than 15 years, federal and state policymakers have focused on increasing the number of people insured, which they expected would shore up hospital finances and make care more available and affordable.
“Vermont’s struggles are a wake-up call that insurance is only one piece of the puzzle to ensuring access to care,” said Keith Mueller, a rural health expert at the University of Iowa.
Regulators and consultants say the state’s small, aging population of about 650,000 makes spreading insurance risk difficult. That demographic challenge is compounded by geography, as many Vermonters live in rural areas, where it’s difficult to attract more health workers to address shortages.
At least part of the cost spike can be attributed to patients crossing state lines for quicker care in New York and Massachusetts. Those visits can be more expensive for both insurers and patients because of long ambulance rides and charges from out-of-network providers.
Patients who stay, like Lynne Drevik, face long waits. Drevik said her doctor told her in April that she needed knee replacement surgeries — but the earliest appointment would be in January for one knee and the following April for the other.
Drevik, 59, said it hurts to climb the stairs in the 19th-century farmhouse in Montgomery Center she and her husband operate as an inn and a spa. “My life is on hold here, and it’s hard to make any plans,” she said. “It’s terrible.”
Health experts say some of the state’s health system troubles are self-inflicted.
Unlike most states, Vermont regulates hospital and insurance prices through an independent agency, the Green Mountain Care Board. Until recently, the board typically approved whatever price changes companies wanted, said Julie Wasserman, a health consultant in Vermont.
The board allowed one health system — the University of Vermont Health Network — to control about two-thirds of the state’s hospital market and allowed its main facility, the University of Vermont Medical Center in Burlington, to raise its prices until it ranked among the nation’s most expensive, she said, citing data the board presented in September.
Hospital officials contend their prices are no higher than industry averages.
But for 2025, the board required the University of Vermont Medical Center to cut the prices it bills private insurers by 1%.
The nonprofit system says it is navigating its own challenges. Top officials say a severe lack of housing makes it hard to recruit workers, while too few mental health providers, nursing homes, and long-term care services often create delays in discharging patients, adding to costs.
Two-thirds of the system’s patients are covered by Medicare or Medicaid, said CEO Sunny Eappen. Both government programs pay providers lower rates than private insurance, which Eappen said makes it difficult to afford rising prices for drugs, medical devices, and labor.
Officials at the University of Vermont Medical Center point to several ways they are trying to adapt. They cited, for example, $9 million the hospital system has contributed to the construction of two large apartment buildings to house new workers, at a subsidized price for lower-income employees.
The hospital also has worked with community partners to open a mental health urgent care center, providing an alternative to the emergency room.
In the ER, curtains separate areas in the hallway where patients can lie on beds or gurneys for hours waiting for a room. The hospital also uses what was a storage closet as an overflow room to provide care.
“It’s good to get patients into a hallway, as it’s better than a chair,” said Mariah McNamara, an ER doctor and associate chief medical officer with the hospital.
For the about 250 days a year when the hospital is full, doctors face pressure to discharge patients without the ideal home or community care setup, she said. “We have to go in the direction of letting you go home without patient services and giving that a try, because otherwise the hospital is going to be full of people, and that includes people that don’t need to be here,” McNamara said.
Searching for solutions, the Green Mountain Care Board hired a consultant who recommended a number of changes, including converting four rural hospitals into outpatient facilities, in a worst-case scenario, and consolidating specialty services at several others.
The consultant, Bruce Hamory, said in a call with reporters that his report provides a road map for Vermont, where “the health care system is no match for demographic, workforce, and housing challenges.”
But he cautioned that any fix would require sacrifice from everyone, including patients, employers, and health providers. “There is no simple single policy solution,” he said.
One place Hamory recommended converting to an outpatient center only was North Country Hospital in Newport, a village in Vermont’s least populated region, known as the Northeast Kingdom.
The 25-bed hospital has lost money for years, partly because of an electronic health record system that has made it difficult to bill patients. But the hospital also has struggled to attract providers and make enough money to pay them.
Officials said they would fight any plans to close the hospital, which recently dropped several specialty services, including pulmonology, neurology, urology, and orthopedics. It doesn’t have the cash to upgrade patient rooms to include bathroom doors wide enough for wheelchairs.
On a recent morning, CEO Tom Frank walked the halls of his hospital. The facility was quiet, with just 14 admitted patients and only a couple of people in the ER. “This place used to be bustling,” he said of the former pulmonology clinic.
Frank said the hospital breaks even treating Medicare patients, loses money treating Medicaid patients, and makes money from a dwindling number of privately insured patients.
The state’s strict regulations have earned it an antihousing, antibusiness reputation, he said. “The cost of health care is a symptom of a larger problem.”
About 30 miles south of Newport, Andy Kehler often worries about the cost of providing health insurance to the 85 workers at Jasper Hill Farm, the cheesemaking business he co-owns.
“It’s an issue every year for us, and it looks like there is no end in sight,” he said.
Jasper Hill pays half the cost of its workers’ health insurance premiums because that’s all it can afford, Kehler said. Employees pay $1,700 a month for a family, with a $5,000 deductible.
“The coverage we provide is inadequate for what you pay,” he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
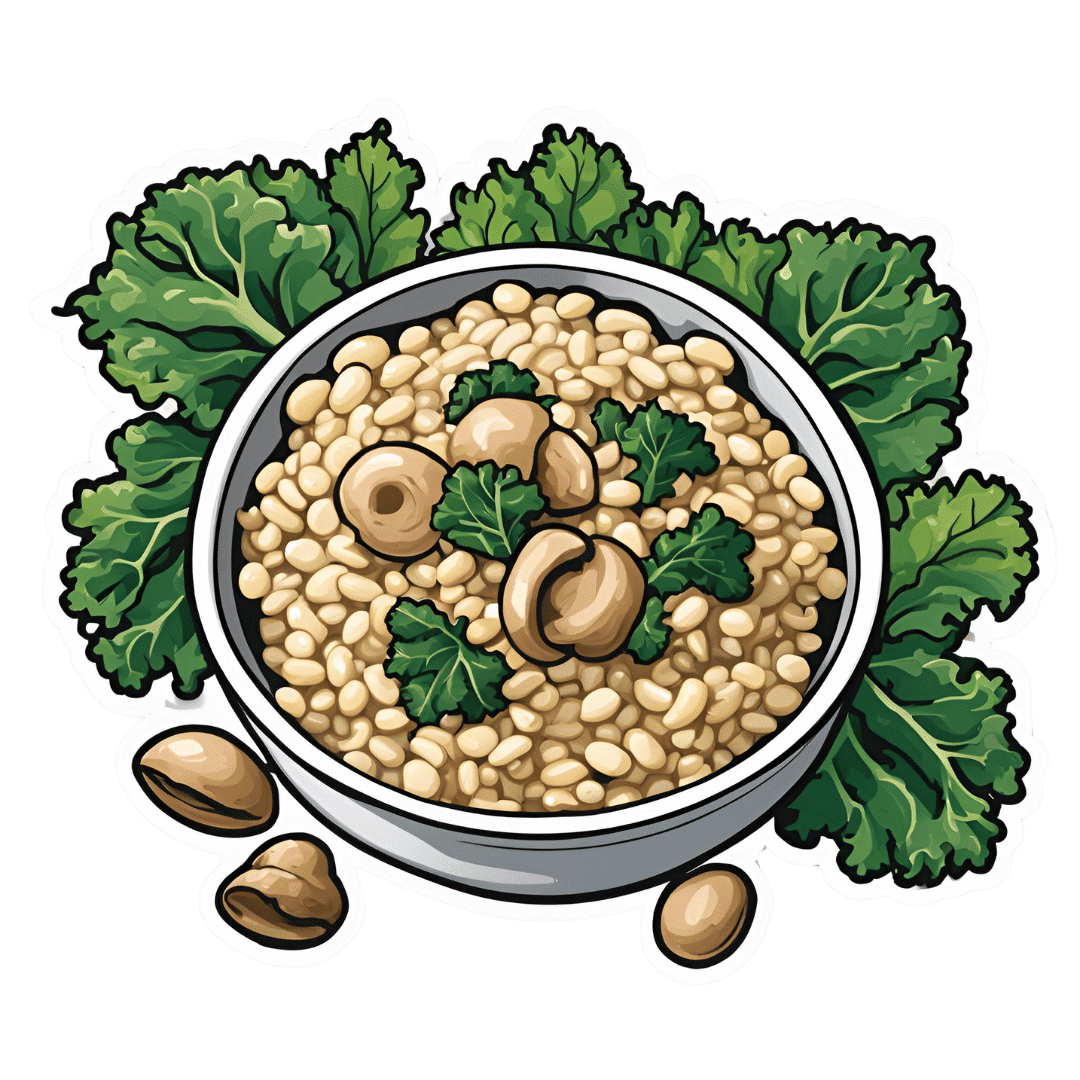
Anti-Aging Risotto With Mushrooms, White Beans, & Kale
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This risotto is made with millet, which as well as being gluten-free, is high in resistant starch that’s great for both our gut and our blood sugars. Add the longevity-inducing ergothioneine in the shiitake and portobello mushrooms, as well as the well-balanced mix of macro- and micronutrients, polyphenols such as lutein (important against neurodegeneration) not to mention more beneficial phytochemicals in the seasonings, and we have a very anti-aging dish!
You will need
- 3 cups low-sodium vegetable stock
- 3 cups chopped fresh kale, stems removed (put the removed stems in the freezer with the vegetable offcuts you keep for making low-sodium vegetable stock)
- 2 cups thinly sliced baby portobello mushrooms
- 1 cup thinly sliced shiitake mushroom caps
- 1 cup millet, as yet uncooked
- 1 can white beans, drained and rinsed (or 1 cup white beans, cooked, drained, and rinsed)
- ½ cup finely chopped red onion
- ½ bulb garlic, finely chopped
- ¼ cup nutritional yeast
- 1 tbsp balsamic vinegar
- 2 tsp ground black pepper
- 1 tsp white miso paste
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a sauté or other pan suitable for both frying and volume-cooking. Fry the onion for about 5 minutes until soft, and then add the garlic, and cook for a further 1 minute, and then turn the heat down low.
2) Add about ¼ cup of the vegetable stock, and stir in the miso paste and MSG/salt.
3) Add the millet, followed by the rest of the vegetable stock. Cover and allow to simmer for 30 minutes, until all the liquid is absorbed and the millet is tender.
4) Meanwhile, heat a little oil to a medium heat in a skillet, and cook the mushrooms (both kinds), until lightly browned and softened, which should only take a few minutes. Add the vinegar and gently toss to coat the mushrooms, before setting side.
5) Remove the millet from the heat when it is done, and gently stir in the mushrooms, nutritional yeast, white beans, and kale. Cover, and let stand for 10 minutes (this will be sufficient to steam the kale in situ).
6) Uncover and fluff the risotto with a fork, sprinkling in the black pepper as you do so.
7) Serve. For a bonus for your tastebuds and blood sugars, drizzle with aged balsamic vinegar.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Magic Of Mushrooms: The “Longevity Vitamin” (That’s Not A Vitamin)
- Brain Food? The Eyes Have It!
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: