Can I take antihistamines everyday? More than the recommended dose? What if I’m pregnant? Here’s what the research says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Allergies happen when your immune system overreacts to a normally harmless substance like dust or pollen. Hay fever, hives and anaphylaxis are all types of allergic reactions.
Many of those affected reach quickly for antihistamines to treat mild to moderate allergies (though adrenaline, not antihistamines, should always be used to treat anaphylaxis).
If you’re using oral antihistamines very often, you might have wondered if it’s OK to keep relying on antihistamines to control symptoms of allergies. The good news is there’s no research evidence to suggest regular, long-term use of modern antihistamines is a problem.
But while they’re good at targeting the early symptoms of a mild to moderate allergic reaction (sneezing, for example), oral antihistamines aren’t as effective as steroid nose sprays for managing hay fever. This is because nasal steroid sprays target the underlying inflammation of hay fever, not just the symptoms.
Here are the top six antihistamines myths – busted.

Myth 1. Oral antihistamines are the best way to control hay fever symptoms
Wrong. In fact, the recommended first line medical treatment for most patients with moderate to severe hay fever is intranasal steroids. This might include steroid nose sprays (ask your doctor or pharmacist if you’d like to know more).
Studies have shown intranasal steroids relieve hay fever symptoms better than antihistamine tablets or syrups.
To be effective, nasal steroids need to be used regularly, and importantly, with the correct technique.
In Australia, you can buy intranasal steroids without a doctor’s script at your pharmacy. They work well to relieve a blocked nose and itchy, watery eyes, as well as improve chronic nasal blockage (however, antihistamine tablets or syrups do not improve chronic nasal blockage).
Some newer nose sprays contain both steroids and antihistamines. These can provide more rapid and comprehensive relief from hay fever symptoms than just oral antihistamines or intranasal steroids alone. But patients need to keep using them regularly for between two and four weeks to yield the maximum effect.
For people with seasonal allergic rhinitis (hayfever), it may be best to start using intranasal steroids a few weeks before the pollen season in your regions hits. Taking an antihistamine tablet as well can help.
Antihistamine eye drops work better than oral antihistamines to relieve acutely itchy eyes (allergic conjunctivitis).
Myth 2. My body will ‘get used to’ antihistamines
Some believe this myth so strongly they may switch antihistamines. But there’s no scientific reason to swap antihistamines if the one you’re using is working for you. Studies show antihistamines continue to work even after six months of sustained use.
Myth 3. Long-term antihistamine use is dangerous
There are two main types of antihistamines – first-generation and second-generation.
First-generation antihistamines, such as chlorphenamine or promethazine, are short-acting. Side effects include drowsiness, dry mouth and blurred vision. You shouldn’t drive or operate machinery if you are taking them, or mix them with alcohol or other medications.
Most doctors no longer recommend first-generation antihistamines. The risks outweigh the benefits.
The newer second-generation antihistamines, such as cetirizine, fexofenadine, or loratadine, have been extensively studied in clinical trials. They are generally non-sedating and have very few side effects. Interactions with other medications appear to be uncommon and they don’t interact badly with alcohol. They are longer acting, so can be taken once a day.
Although rare, some side effects (such as photosensitivity or stomach upset) can happen. At higher doses, cetirizine can make some people feel drowsy. However, research conducted over a period of six months showed taking second-generation antihistamines is safe and effective. Talk to your doctor or pharmacist if you’re concerned.

Myth 4. Antihistamines aren’t safe for children or pregnant people
As long as it’s the second-generation antihistamine, it’s fine. You can buy child versions of second-generation antihistamines as syrups for kids under 12.
Though still used, some studies have shown certain first-generation antihistamines can impair childrens’ ability to learn and retain information.
Studies on second-generation antihistamines for children have found them to be safer and better than the first-generation drugs. They may even improve academic performance (perhaps by allowing kids who would otherwise be distracted by their allergy symptoms to focus). There’s no good evidence they stop working in children, even after long-term use.
For all these reasons, doctors say it’s better for children to use second-generation than first-generation antihistimines.
What about using antihistimines while you’re pregnant? One meta analysis of combined study data including over 200,000 women found no increase in fetal abnormalities.
Many doctors recommend the second-generation antihistamines loratadine or cetirizine for pregnant people. They have not been associated with any adverse pregnancy outcomes. Both can be used during breastfeeding, too.
Myth 5. It is unsafe to use higher than the recommended dose of antihistamines
Higher than standard doses of antihistamines can be safely used over extended periods of time for adults, if required.
But speak to your doctor first. These higher doses are generally recommended for a skin condition called chronic urticaria (a kind of chronic hives).
Myth 6. You can use antihistamines instead of adrenaline for anaphylaxis
No. Adrenaline (delivered via an epipen, for example) is always the first choice. Antihistamines don’t work fast enough, nor address all the problems caused by anaphylaxis.
Antihistamines may be used later on to calm any hives and itching, once the very serious and acute phase of anaphylaxis has been resolved.
In general, oral antihistamines are not the best treatment to control hay fever – you’re better off with steroid nose sprays. That said, second-generation oral antihistamines can be used to treat mild to moderate allergy symptoms safely on a regular basis over the long term.
Janet Davies, Respiratory Allergy Stream Co-chair, National Allergy Centre of Excellence; Professor and Head, Allergy Research Group, Queensland University of Technology; Connie Katelaris, Professor of Immunology and Allergy, Western Sydney University, and Joy Lee, Respiratory Allergy Stream member, National Allergy Centre of Excellence; Associate Professor, School of Public Health and Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
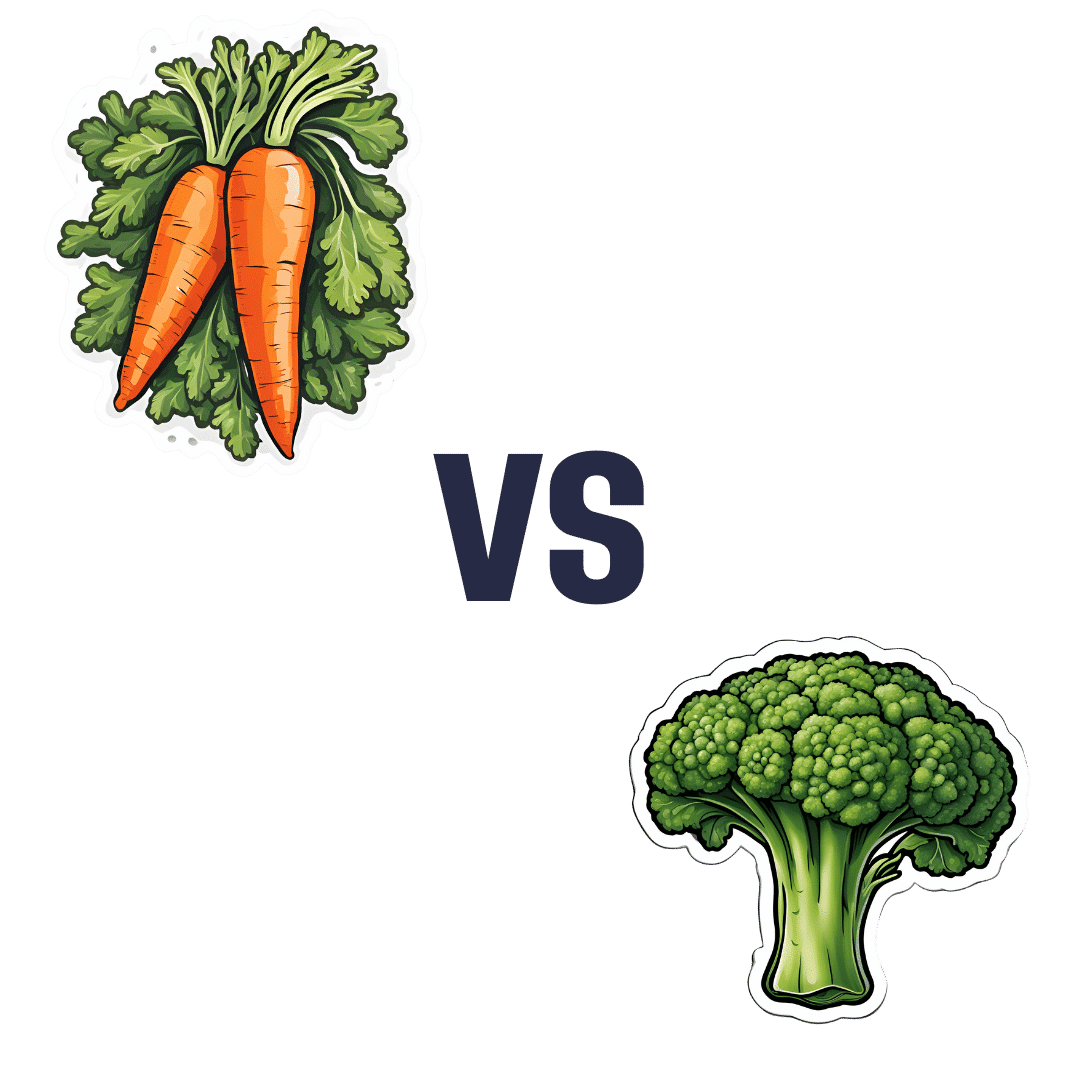
Carrots vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to broccoli, we picked the broccoli.
Why?
These are both excellent candidates that should be in everyone’s diet, but there’s a clear winner:
In terms of macros, carrots have 50% more carbs for the same fiber (giving carrots the relatively higher glycemic index, though really, nobody is getting metabolic disease from eating carrots, which are a low-GI food already), while broccoli has more protein. By the numbers, it’s a nominal win for broccoli here, but really, both are great.
In the category of vitamins, carrots have more of vitamins A and B3, while broccoli has more of vitamins B1, B2, B5, B6, B7, B9, C, E, K, and choline. An easy win for broccoli. We’d like to emphasize, though, that this doesn’t mean carrots don’t have lots of vitamins—they do—it’s just that broccoli has even more!
When it comes to minerals, carrots are genuinely great, and/but not higher in any minerals than broccoli, while broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, selenium, and zinc. So again, a clear win for broccoli, despite carrots’ fortitude.
All in all, an overwhelming win for broccoli, though once again, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Share This Post
-
The Anti-Stress Herb That Also Fights Cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What does Rhodiola rosea actually do, anyway?
Rhodiola rosea (henceforth, “rhodiola”) is a flowering herb whose roots have adaptogenic properties.
In the cold, mountainous regions of Europe and Asia where it grows, it has been used in herbal medicine for centuries to alleviate anxiety, fatigue, and depression.
What does the science say?
Well, let’s just say the science is more advanced than the traditional use:
❝In addition to its multiplex stress-protective activity, Rhodiola rosea extracts have recently demonstrated its anti-aging, anti-inflammation, immunostimulating, DNA repair and anti-cancer effects in different model systems❞
Nor is how it works a mystery, as the same paper explains:
❝Molecular mechanisms of Rhodiola rosea extracts’s action have been studied mainly along with one of its bioactive compounds, salidroside. Both Rhodiola rosea extracts and salidroside have contrasting molecular mechanisms on cancer and normal physiological functions.
For cancer, Rhodiola rosea extracts and salidroside inhibit the mTOR pathway and reduce angiogenesis through down-regulation of the expression of HIF-1α/HIF-2α.
For normal physiological functions, Rhodiola rosea extracts and salidroside activate the mTOR pathway, stimulate paracrine function and promote neovascularization by inhibiting PHD3 and stabilizing HIF-1α proteins in skeletal muscles❞
~ Ibid.
And, as for the question of “do the supplements work?”,
❝In contrast to many natural compounds, salidroside is water-soluble and highly bioavailable via oral administration❞
~ Ibid.
And as to how good it is:
❝Rhodiola rosea extracts and salidroside can impose cellular and systemic benefits similar to the effect of positive lifestyle interventions to normal physiological functions and for anti-cancer❞
~ Ibid.
Source: Rhodiola rosea: anti-stress, anti-aging, and immunostimulating properties for cancer chemoprevention
But that’s not all…
We can’t claim this as a research review if we only cite one paper (even if that paper has 144 citations of its own), and besides, it didn’t cover all the benefits yet!
Let’s first look at the science for the “traditional use” trio of benefits:
When you read those, what are your first thoughts?
Please don’t just take our word for things! Reading even just the abstracts (summaries) at the top of papers is a very good habit to get into, if you don’t have time (or easy access) to read the full text.
Reading the abstracts is also a very good way to know whether to take the time to read the whole paper, or whether it’s better to skip onto a different one.
- Perhaps you noticed that the paper we cited for anxiety was quite a small study.
- The fact is, while we found mountains of evidence for rhodiola’s anxiolytic (antianxiety) effects, they were all small and/or animal studies. So we picked a human study and went with it as illustrative.
- Perhaps you noticed that the paper we cited for fatigue pertained mostly to stress-related fatigue.
- This, we think, is a feature not a bug. After all, most of us experience fatigue because of the general everything of life, not because we just ran a literal marathon.
- Perhaps you noticed that the paper we cited for depression said it didn’t work as well as sertraline (a very common pharmaceutical SSRI antidepressant).
- But, it worked almost as well and it had far fewer adverse effects reported. Bear in mind, the side effects of antidepressants are the reason many people avoid them, or desist in taking them. So rhodiola working almost as well as sertraline for far fewer adverse effects, is quite a big deal!
Bonus features
Rhodiola also putatively offers protection against Alzheimer’s disease, Parkinson’s disease, and cerebrovascular disease in general:
Rosenroot (Rhodiola): Potential Applications in Aging-related Diseases
It may also be useful in the management of diabetes (types 1 and 2), but studies so far have only been animal studies, and/or in vitro studies. Here are two examples:
- Antihyperglycemic action of rhodiola-aqeous extract in type 1 diabetic rats
- Evaluation of Rhodiola crenulata and Rhodiola rosea for management of type 2 diabetes and hypertension
How much to take?
Dosages have varied a lot in studies. However, 120mg/day seems to cover most bases. It also depends on which of rhodiola’s 140 active compounds a particular benefit depends on, though salidroside and rosavin are the top performers.
Where to get it?
As ever, we don’t sell it (or anything else) but here’s an example product on Amazon.
Enjoy!
Share This Post
- Perhaps you noticed that the paper we cited for anxiety was quite a small study.
-
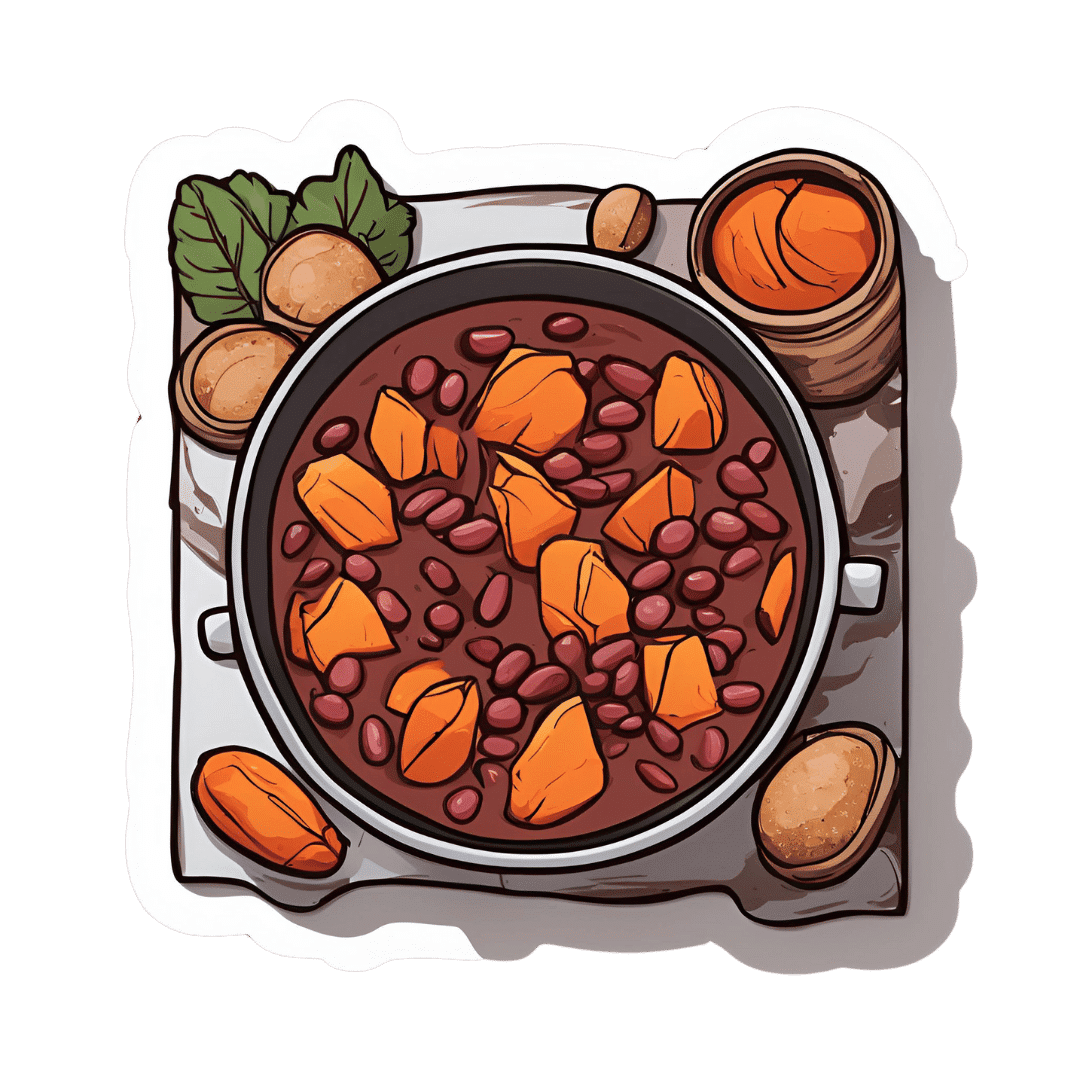
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Share This Post
Related Posts
-
Seasonal Affective Disorder (Beyond Sunlight!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us in the Northern Hemisphere, the time of increasing darkness is upon us again. Depending on our latitude, the sun barely rises before it skitters off again. And depending on other factors of our geography, we might not get much sun during that time (writer’s example: the ancient bog from which I write has been surrounded by fog for two weeks now).
So, what to do about it?
Firstly, we can make the most of whatever sun we do get (especially in the morning, if possible), and we can of course make some use of artificial sunlight. To save doubling up, we’ll link to what we previously wrote about optimizing both of those things:
‘Tis To Season To Be SAD-Savvy
More ways to get serotonin
Sunlight, of course, triggers our bodies to make serotonin, and hence we often make less of it during winter. But, there are other ways to get serotonin too, and one of the best ways is spending time in nature. Yes, even if the weather is gloomy, provided there are still visible green things and you are seeing them, it will promote serotonin production.
Of course, it may not be the season for picnics, but a morning walk through a local park or other green space is ideal.
On which note, gardening remains a good activity. Not a lot of people do so much gardening after a certain point in the year, but in one way, it’s more important than ever to get some soil under your fingernails:
There are bacteria in soil (specifically: Mycobacterium vaccae) that work similarly to antidepressants.
When something is described as having an effect similar to antidepressants, it’s usually hyperbole. In this case, it’s medicine, and literally works directly on the serotonergic system (as do many, but not all, antidepressants).
See also: Antidepressants: Personalization Is Key!
While many antidepressants are selective serotonin uptake inhibitors (i.e., they slow the rate at which your brain loses serotonin), Mycobacterium vaccae increases the rate at which you produce serotonin. So, you feel happier, more relaxed, while also feeling more energized.
^this one’s a mouse study, but we’re including it because it covers exactly how it works in the brain, which is something that the ethics board wouldn’t let them do on humans, due to the need for slicing the brains up for examination.
As to how to benefit: touching soil will get you “infected” by the bacteria, yes, even if you wash your hands later. Growing food in the soil and eating the good (including if you wash and cook it) is even better.
Boost the other “happiness chemicals”
Serotonin is just one “happiness hormone”, other feel-good neurotransmitters that are just as important include dopamine and oxytocin.
Dopamine is most associated with being the “reward chemical”, so it pays to do things that you find rewarding. If you’re stuck for ideas, engaging in small acts of kindness is a sure-fire way to get dopamine flowing and lift your own mood as well as theirs.
See also: 10 Ways To Naturally Boost Dopamine
Oxytocin, meanwhile is the “cuddle chemical”, and can be triggered even if you have nobody to cuddle*. If you do, by the way, make it at least 20–30 seconds, as that’s generally how long it takes to get oxytocin flowing.
*Vividly imagining it has much the same effect, since the brain can’t tell the difference. Alternatively, looking at pictures/videos (your choice) of small cute animals tends to work for most people also.
For more on these things, check out: Neurotransmitter Cheatsheet
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creamy Zucchini, Edamame, & Asparagus Linguine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein, fiber, and polyphenols are the dish of the day here:
You will need
- 1½ cups milk (your choice what kind; we recommend soy for its neutral taste, though hazelnut’s nutty flavor would also work in this recipe)
- 6 oz wholegrain linguine (or your pasta of choice)
- 2 zucchini, thinly sliced
- 5 oz edamame beans (frozen is fine)
- 5 oz asparagus tips, cut into 2″ lengths
- ½ bulb garlic, crushed
- 1 tbsp chia seeds
- 1 small handful arugula
- 1 small handful parsley, chopped
- A few mint leaves, chopped
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan or similar, over a low to medium heat. Add the zucchini and cook for 5 minutes until they start to soften.
2) Add the garlic and continue cooking for 1 minute, stirring gently.
3) Add the milk, bring to the boil, and add the past, chia seeds (the resistant starch from the pasta will help thicken the sauce, as will the chia seeds), and MSG or salt.
4) Reduce the heat, cover, and simmer for 8 minutes.
5) Add the edamame beans and asparagus, and cook for a further 2 minutes, or until the pasta is cooked but still firm to the bite. The sauce should be quite thick now.
6) Stir in the remaining ingredients and serve, adding a garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Make Social Media Work For Your Mental Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Social Media, But Healthy
Social media has a bad reputation, and rightly so. It’s calculated to trick you into doomscrolling and rage-posting, and it encourages you to compare your everyday life to other people’s carefully-curated highlight reels.
Rebalancing Dopamine (Without “Dopamine Fasting”)
But it doesn’t have to be so.
Find your community
One of the biggest strengths social media has going for it is that it can, if used well, be a powerful tool for community. As for why that’s important from a health perspective, see:
How To Beat Loneliness & Isolation
Loneliness & isolation do, of course, kill people. By:
- Accidents, e.g. household fall but nobody notices for a week
- Depression and resultant decline (and perhaps even active suicidality)
- Cognitive decline from a lack of social contact
Read more:
- The Mental Health First-Aid That You’ll Hopefully Never Need
- How To Stay Alive (When You Really Don’t Want To)
- The Five Key Traits Of Healthy Aging
So, what’s “community” to you, and to what extent can you find it online? Examples might include:
- A church, or other religious community, if we be religious
- The LGBT+ community, or even just a part of it, if that fits for us
- Any mutual-support oriented, we-have-this-shared-experience community, could be anything from AA to the VA.
Find your people, and surround yourself with them. There are more than 8,000,000,000 people on this planet, you will not find all the most compatible ones with you on your street.
Grow & nurture your community
Chances are, you have a lot to contribute. Your life experiences are valuable.
Being of service to other people is strongly associated “flourishing”, per the science.
Indeed, one of the questions on the subjective wellness scale test is to ask how much one agrees with the statement “I actively contribute to the happiness and wellbeing of others”.
See: Are You Flourishing? (There’s a Scale)
So, help people, share your insights, create whatever is relevant to your community and fits your skills (it could be anything from art to tutorials to call-to-action posts or whatever works for you and your community)
As a bonus: when people notice you are there for them, they’ll probably be there for you, too. Not always, sadly, but there is undeniable strength in numbers.
Remember it’s not the boss of you
Whatever social media platform(s) you use, the companies in question will want you to use it in the way that is most profitable for them.
Usually that means creating a lot of shallow content, clicking on as many things as possible, and never logging off.
Good ways to guard against that include:
- Use the social media from a computer rather than a handheld device
- Disable “infinite scroll” in the settings, if possible
- Set a timer and stick to it
- Try to keep your interactions to only those that are relevant and kind (for the good of your own health, let alone anyone else’s)
On that latter note…
Before posting, ask “what am I trying to achieve here?” and ensure your action is aligned with your actual desires, and not just reactivity. See also:
A Bone To Pick… Up And Then Put Back Where We Found It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: