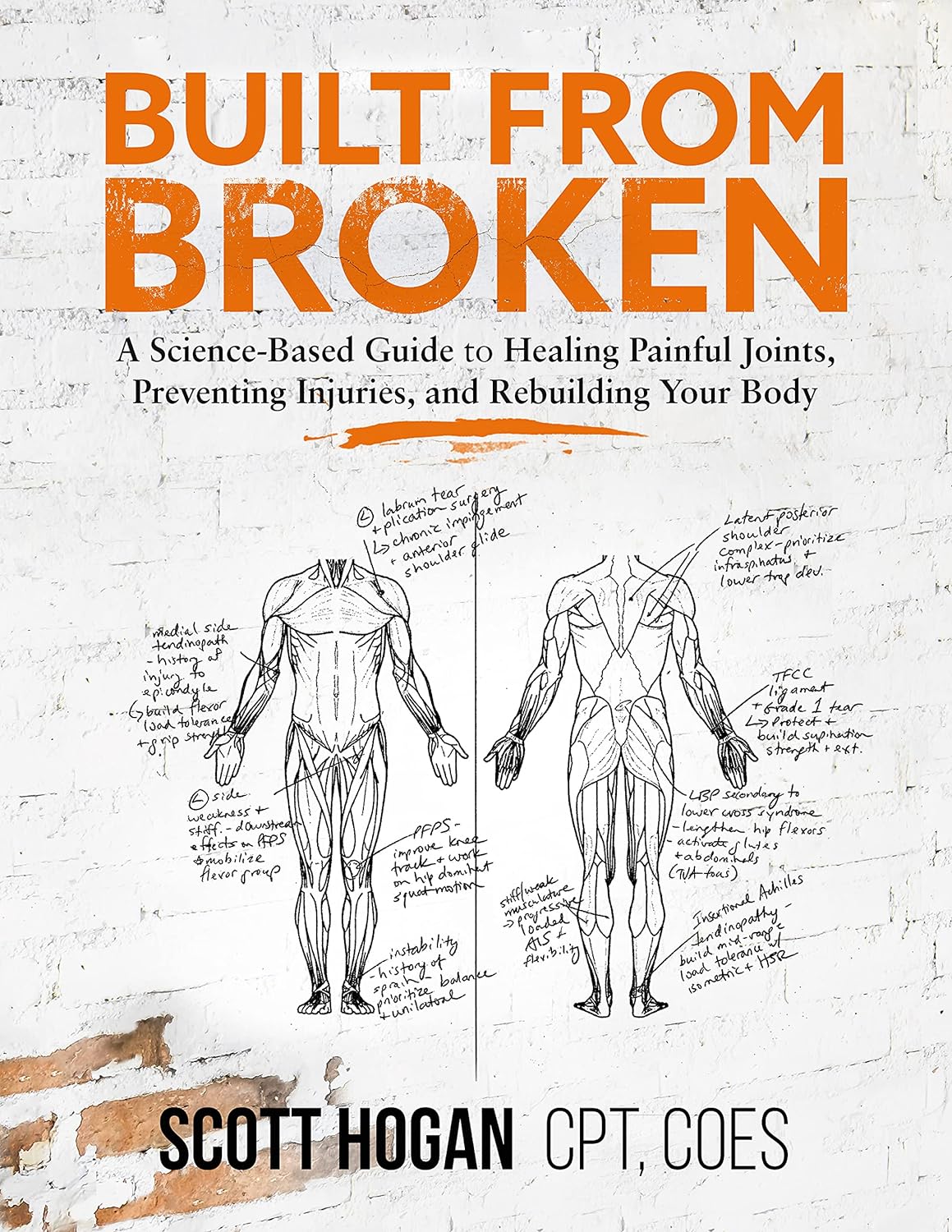
Built from Broken – by Scott Hogan, CPT, COES
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So many exercise programs come with the caveat “consult your doctor before engaging in any new activity”, and the safe-but-simple “do not try to train through an injury”.
Which is all very well and good for someone in fabulous health who sprained an ankle while running and can just wait a bit, but what about those of us carrying…
- long-term injuries
- recurring injuries
- or just plain unfixable physical disabilities?
That’s where physiotherapist Scott Hogan comes in. The subtitle line goes:
❝A Science-Based Guide to Healing Painful Joints, Preventing Injuries, and Rebuilding Your Body❞
…but he does also recognize that there are some things that won’t bounce back.
On the other hand… There are a lot of things that get written off by doctors as “here’s some ibuprofen” that, with consistent mindful training, could actually be fixed.
Hogan delivers again and again in this latter category! You’ll see on Amazon that the book has thousands of 4- and 5-star ratings and many glowing reviews, and it’s for a reason or three:
- The book first lays a foundational knowledge of the most common injuries likely to impede us from training
- It goes on to give step-by-step corrective exercises to guide your body through healing itself. Your body is trying to heal itself anyway; you might as well help it accomplish that!
- It finishes up with a comprehensive (and essential) guide to train for the strength and mobility that will help you avoid future problems.
In short: a potentially life-changing book if you have some (likely back- or joint-related) problem that needs overcoming!
And if you don’t? An excellent pre-emptive guide all the same. This is definitely one of those “an ounce of prevention is better than a pound of cure” things.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sensitive – by Jenn Granneman and Andre Sólo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is written for what is called the “Highly Sensitive Person”, which makes it sound like a very rare snowflake condition, when in fact the diagnostic criteria (discussed early in the book) yield a population bell curve of 30:40:30, whereupon 30% are in the band of “high sensitivity”, 40% “normal sensitivity” and the remainder “low sensitivity”. You may note that “high” and “low” together outnumber “normal”, but statistics is like that.
So, if you’re one of the approximately one in three people who fall into the higher category, and/or you have a loved one who is in that category, then this book looks at the many advantages to a commonly stigmatized and (by cruel irony) criticized personality trait.
Those advantages range from personal life to work and even public life (yes, really), and can be grown, positively highlighted, used, and enjoyed.
In the category of criticism, the book does not usefully cover the benefit of psychological resilience. Resilience does not mean losing sensitivity, just, being able to also dry one’s tears and weather life’s slings and arrows when the world is harsher than one might like. But for the authors, they have stacked all their chips on “we must make the world a better place”. Which is a noble goal, if not always an immediately attainable one.
Bottom line: if you are more sensitive than average and would like to use that to benefit yourself and those around you, then this is the book for you!
Click here to check out Sensitive, and make the most of your strengths!
Share This Post
-
Pistachios vs Almonds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to almonds, we picked the almonds.
Why?
It was very close! And those who’ve been following our “This or That” comparisons might be aware that pistachios and almonds have both been winning their respective comparisons with other nuts so far, so today we put them head-to-head.
In terms of macros, almonds have a little more protein and a little more fiber—as well as slightly more fat, though the fats are healthy. Pistachios, meanwhile, are higher in carbs. A moderate win for almonds on the macro front.
When it comes to vitamins, pistachios have more of vitamins A, B1, and B6, while almonds have more of vitamins B2, B3, and E. We could claim a slight victory for pistachios, based on the larger margins, or else a slight victory for almonds, based on vitamin E being a more common nutritional deficiency than vitamin A, and therefore the more useful vitamin to have more of. We’re going to call this category a tie.
In the category of minerals, almonds lead with more calcium, magnesium, manganese, and zinc, while pistachios boast more copper, potassium, and selenium, though the margins are more modest for pistachios. A moderate win for almonds on minerals, therefore.
Adding up the sections gives a win for almonds, but of course, do enjoy both, because both are excellent in their own right.
Want to learn more?
You might like to read:
- Why You Should Diversify Your Nuts!
- Pistachios vs Walnuts – Which is Healthier?
- Almonds vs Cashews – Which is Healthier?
Take care!
Share This Post
-
Three-Bean Chili & Cashew Cream
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A hearty classic with a twist! Delicious and filling and full of protein, fiber, and powerful phytonutrients (including heavy-hitters ergothioneine and lycopene), this recipe is also quite flexible, so you can always add in extra seasonal vegetables if you like (to get you started: cherry tomatoes in summer and sweet potato in fall are fine options)!
You will need
- 1 cup low-sodium vegetable stock (ideally you made it yourself from vegetable offcuts you kept in the freezer for this purpose, but if not, you should be able to find low-sodium stock cubes)
- 1 can kidney beans, drained and rinsed
- 1 can black beans, drained and rinsed
- 1 can chickpeas, drained and rinsed
- 2 cans chopped tomatoes
- 1 onion, finely chopped
- 1 carrot, diced
- 2 celery sticks, chopped
- 4 oz mushrooms, chopped
- ½ bulb garlic, crushed
- 2 tbsp tomato purée
- 1 red chili pepper, finely chopped (multiply per your heat preferences)
- 1 tbsp ground paprika
- 1 tbsp black pepper, coarse ground
- 2 tsp fresh rosemary (or 1 tbsp dried)
- 2 tsp fresh thyme (or 1 tbsp dried)
- 1 tsp ground cumin
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
For the cashew cream:
- 6 oz cashews, soaked in kettle-hot water for at least 15 minutes
- 1 tbsp nutritional yeast
- 1 tsp lemon juice
To serve:
- Handful of chopped parsley
- Your carbohydrates of choice; we recommend our Tasty Versatile Rice recipe, and/or our Delicious Quinoa Avocado Bread recipe.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some olive oil in a skillet and fry the onion for about 5 minutes, stirring as necessary.
2) Add the garlic and chili and cook for a further 1 minute.
3) Add the celery, carrot, and mushrooms and continue cooking for 1–2 minutes.
4) Add everything else from the main section, taking care to stir well to distribute the seasonings evenly. Reduce the heat and allow to simmer for around 20 minutes, stirring occasionally.
5) While you are waiting, drain the cashews, and add them to a high-speed blender with ½ cup (fresh) cold water, as well as the nutritional yeast and lemon juice. Blend on full power until smooth; this may take about 3 minutes, so we recommend doing it in 30-second bursts to avoid overheating the motor. You’ll also probably need to scrape it down the sides at least once. You can add a little more water if you want the cream to be thinner than it is appearing, but go slowly if you do.
6) Serve with rice, adding a dollop of the cream and garnishing with parsley, with bread on the side if you like.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What’s Your Plant Diversity Score?
- Three Daily Servings of Beans?
- Kidney Beans or Black Beans – Which is Healthier?
- What Matters Most For Your Heart?
- “The Longevity Vitamin” (That’s Not A Vitamin)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
Related Posts
-
Lacking Motivation? Science Has The Answer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Science Of Motivation (And How To Use It To Your Advantage)
When we do something rewarding, our brain gets a little (or big!) spike of dopamine. Dopamine is popularly associated with pleasure—which is fair— but there’s more to it than this.
Dopamine is also responsible for motivation itself, as a prime mover before we do the thing that we find rewarding. If we eat a banana, and enjoy it, perhaps because our body needed the nutrients from it, our brain gets a hit of dopamine.
(and not because bananas contain dopamine; that dopamine is useful for the body, but can’t pass the blood-brain barrier to have an effect on the brain)
So where does the dopamine in our brain come from? That dopamine is made in the brain itself.
Key Important Fact: the brain produces dopamine when it expects an activity to be rewarding.
If you take nothing else away from today’s newsletter, let it be this!
It makes no difference if the activity is then not rewarding. And, it will keep on motivating you to do something it anticipated being rewarding, no matter how many times the activity disappoints, because it’ll remember the very dopamine that it created, as having been the reward.
To put this into an example:
- How often have you spent time aimlessly scrolling social media, flitting between the same three apps, or sifting through TV channels when “there’s nothing good on to watch”?
- And how often did you think afterwards “that was a good and rewarding use of my time; I’m glad I did that”?
In reality, whatever you felt like you were in search of, you were really in search of dopamine. And you didn’t find it, but your brain did make some, just enough to keep you going.
Don’t try to “dopamine detox”, though.
While taking a break from social media / doomscrolling the news / mindless TV-watching can be a great and healthful idea, you can’t actually “detox” from a substance your body makes inside itself.
Which is fortunate, because if you could, you’d die, horribly and miserably.
If you could “detox” completely from dopamine, you’d lose all motivation, and also other things that dopamine is responsible for, including motor control, language faculties, and critical task analysis (i.e. planning).
This doesn’t just mean that you’d not be able to plan a wedding; it also means:
- you wouldn’t be able to plan how to get a drink of water
- you wouldn’t have any motivation to get water even if you were literally dying of thirst
- you wouldn’t have the motor control to be able to physically drink it anyway
Read: Dopamine and Reward: The Anhedonia Hypothesis 30 years on
(this article is deep and covers a lot of ground, but is a fascinating read if you have time)
Note: if you’re wondering why that article mentions schizophrenia so much, it’s because schizophrenia is in large part a disease of having too much dopamine.
Consequently, antipsychotic drugs (and similar) used in the treatment of schizophrenia are generally dopamine antagonists, and scientists have been working on how to treat schizophrenia without also crippling the patient’s ability to function.
Do be clever about how you get your dopamine fix
Since we are hardwired to crave dopamine, and the only way to outright quash that craving is by inducing anhedonic depression, we have to leverage what we can’t change.
The trick is: question how much your motivation aligns with your goals (or doesn’t).
So if you feel like checking Facebook for the eleventieth time today, ask yourself: “am I really looking for new exciting events that surely happened in the past 60 seconds since I last checked, or am I just looking for dopamine?”
You might then realize: “Hmm, I’m actually just looking for dopamine, and I’m not going to find it there”
Then, pick something else to do that will actually be more rewarding. It helps if you make a sort of dopa-menu in advance, of things to pick from. You can keep this as a list on your phone, or printed and pinned up near your computer.
Examples might be: Working on that passion project of yours, or engaging in your preferred hobby. Or spending quality time with a loved one. Or doing housework (surprisingly not something we’re commonly motivated-by-default to do, but actually is rewarding when done). Or exercising (same deal). Or learning that language on Duolingo (all those bells and whistles the app has are very much intentional dopamine-triggers to make it addictive, but it’s not a terrible outcome to be addicted to learning!).
Basically… Let your brain’s tendency to get led astray work in your favor, by putting things in front of it that will lead you in good directions.
Things for your health and/or education are almost always great things to allow yourself the “ooh, shiny” reaction and pick them up, try something new, etc.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Make Your Negativity Work For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s The Right Balance?
We’ve written before about positivity the pitfalls and perils of toxic positivity:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
…as well as the benefits that can be found from selectively opting out of complaining:
A Bone To Pick… Up And Then Put Back Where We Found It
So… What place, if any, does negativity usefully have in our lives?
Carrot and Stick
We tend to think of “carrot and stick” motivation being extrinsic, i.e. there is some authority figure offering is reward and/or punishment, in response to our reactions.
In those cases when it really is extrinsic, the “stick” can still work for most people, by the way! At least in the short term.
Because in the long term, people are more likely to rebel against a “stick” that they consider unjust, and/or enter a state of learned helplessness, per “I’ll never be good enough to satisfy this person” and give up trying to please them.
But what about when you have your own carrot and stick? What about when it comes to, for example, your own management of your own healthy practices?
Here it becomes a little different—and more effective. We’ll get to that, but first, bear with us for a touch more about extrinsic motivation, because here be science:
We will generally be swayed more easily by negative feelings than positive ones.
For example, a study was conducted as part of a blood donation drive, and:
- Group A was told that their donation could save a life
- Group B was told that their donation could prevent a death
The negative wording given to group B boosted donations severalfold:
Read the paper: Life or Death Decisions: Framing the Call for Help
We have, by the way, noticed a similar trend—when it comes to subject lines in our newsletters. We continually change things up to see if trends change (and also to avoid becoming boring), but as a rule, the response we get from subscribers is typically greater when a subject line is phrased negatively, e.g. “how to avoid this bad thing” rather than “how to have this good thing”.
How we can all apply this as individuals?
When we want to make a health change (or keep up a healthy practice we already have)…
- it’s good to note the benefits of that change/practice!
- it’s even better to note the negative consequences of not doing it
For example, if you want to overcome an addiction, you will do better for your self-reminders to be about the bad consequences of using, more than the good consequences of abstinence.
See also: How To Reduce Or Quit Alcohol
This goes even just for things like diet and exercise! Things like diet and exercise can seem much more low-stakes than substance abuse, but at the end of the day, they can add healthy years onto our lives, or take them off.
Because of this, it’s good to take time to remember, when you don’t feel like exercising or do feel like ordering that triple cheeseburger with fries, the bad outcomes that you are planning to avoid with good diet and exercise.
Imagine yourself going in for that quadruple bypass surgery, asking yourself whether the unhealthy lifestyle was worth it. Double down on the emotions; imagine your loved ones grieving your premature death.
Oof, that was hard-hitting
It was, but it’s effective—if you choose to do it. We’re not the boss of you! Either way, we’ll continue to send the same good health advice and tips and research and whatnot every day, with the same (usually!) cheery tone.
One last thing…
While it’s good to note the negative, in order to avoid the things that lead to it, it’s not so good to dwell on the negative.
So if you get caught in negative thought spirals or the like, it’s still good to get yourself out of those.
If you need a little help with that sometimes, check out these:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spoon-Fed – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Spector looks at widespread beliefs about food, and where those often scientifically disproven beliefs come from. Hint, there’s usually some manner of “follow the money”.
From calorie-counting to cholesterol content, from fish to bottled water, to why of all the people who self-report having an allergy, only around half turn out to actually have one when tested, Dr. Spector sets the record straight.
The style is as very down-to-earth and not at all self-aggrandizing; the author acknowledges his own mistakes and limitations along the way. In terms of pushing any particular agenda, his only agenda is clear: inform the public about bad science, so that we demand better science going forwards. Along the way, he gives us lots of information that can inform our personal health choices based on better science than indiscriminate headlines wildly (and sometimes intentionally) misinterpreting results.
Read this book, and you may find yourself clicking through to read the studies for yourself, next time you see a bold headline.
Bottom line: this book looks at a lot of what’s wrong with what a lot of people believe about healthy eating. Regular 10almonds readers might not find a lot that’s new here, but it could be a great gift for a would-be health-conscious friend or relative
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: