When Your Brain’s “Get-Up-And-Go” Has Got Up And Gone…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, there are days when the body feels heavy, the brain feels sluggish, and even the smallest tasks feel Herculean.
When these days stack up, this is usually a sign of depression, and needs attention. Unfortunately, when one is in such a state, taking action about it is almost impossible.
Almost, but not quite, as we wrote about previously:
The Mental Health First-Aid You’ll Hopefully Never Need ← this is about as close to true mental health bootstrapping as actually works
Today though, we’re going to assume it’s just an off-day or such. So, what to do about it?
Try turning it off and on again
Sometimes, a reboot is all that’s needed, and if napping is an option, it’s worth considering. However, if you don’t do it right, you can end up groggy and worse off than before, so do check out:
How To Be An Expert Nap-Artist (No More “Sleep Hangovers”!)
If your exhaustion is nevertheless accompanied by stresses that are keeping you from resting, then there’s another “turn it off and on again” process for that:
Fuel in the tank
Our brain is an energy-intensive organ, and cannot run on empty for long. Thus, lacking energy can sometimes simply be a matter of needing to supply some energy. Simple, no? Except, a lot of energy-giving foods can cause a paradoxical slump in energy, so here’s how to avoid that:
Eating For Energy (In Ways That Actually Work)
There are occasions when exhausted, when preparing food seems like too much work. If you’re not in a position to have someone else do it for you, how can you get “most for least” in terms of nutrition for effort?
Many of the above-linked items can help (a bowl of nuts and/or dried fruit is probably not going to break the energy-bank, for instance), but beyond that, there are other considerations too:
How To Eat To Beat Chronic Fatigue (While Chronically Fatigued) ← as the title tells, this is about chronic fatigue, but the advice therein definitely goes for acute fatigue also.
The lights aren’t on
Sometimes it may be that your body is actually fine, but your brain is working in a clunky fashion at best. Assuming there is no more drastic underlying cause for this, a lack of motivation is often as simple as a lack of appropriate dopamine response. When that’s the case…
Lacking Motivation? Science Has The Answer
If, instead, the issue is more serotonin-based than dopamine based, then green places with blue skies are ideal. Depending on geography and season, those things may be in short supply, but the brain is easily tricked with artificial plants and artificial sunlight. Is it as good as a walk in the park on a pleasant summer morning? Probably not, but it’s many times better than nothing, so get those juices flowing:
Neurotransmitter Cheatsheet ← four for the price of one, here!
Schedule time for rest, or your body/brain will schedule it for you
There’s a saying in the field of engineering that “if you don’t schedule time for maintenance, your equipment will schedule it for you”, and the same is true of our body/brain. If you’re struggling to get good quantity, here’s how to at least get good quality:
How To Rest More Efficiently (Yes, Really)
And, importantly,
7 Kinds Of Rest When Sleep Is Not Enough
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Herbs For Evidence-Based Health & Healing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Herbs have been used since prehistoric times to treat injuries and illnesses, but which ones actually work, as opposed to being “old wives’ tales”?
Even today, in pharmacies herbals products may come with a disclaimer “based on traditional use only”, which, in scientific terms, means it likely performs no better than placebo.
This is a “Saturday Life Hacks” edition, not a “Research Review Monday”, so we won’t be doing any deep-dives today, and will instead keep things short and snappy. We’ll also spotlight one main benefit, rather than trying to cover all bases, as we often have room to do on a Monday!
Basil
Helps boost immunity:
Chamomile
Significantly reduces symptoms of osteoarthritis:
(This one challenged your writer’s resolve as it does so many things, it was hard to pick just one. So, she went with one that’s less known that “settling the stomach” and “relieving PMS” and “relaxation” and so forth)
Echinacea
Significantly reduces the risk of catching a cold (but won’t help once you’ve caught it):
Echinacea for preventing and treating the common cold
Elderberry
Significantly hastens recovery from upper respiratory viral infections:
Evening Primrose
Fights neuropathy, along with many other benefits:
An updated review on pharmacological activities and phytochemical constituents of evening primrose
Fennel
Antinflammatory, along with many other benefits:
Ginkgo biloba
Antioxidant effects provide anti-aging benefits:
Advances in the Studies of Ginkgo Biloba Leaves Extract on Aging-Related Diseases
Ginseng
Combats fatigue:
Ginseng as a Treatment for Fatigue: A Systematic Review
Lavender
Enjoyed for its sedative effects, which is really does have:
Evidence for Sedative Effects of the Essential Oil of Lavender after Inhalation
Sage
Helps fight HIV type 1 and Herpes simplex type 2 (and probably other viruses, but that’s what we have the science for right now):
Aqueous extracts from peppermint, sage and lemon balm leaves display potent anti-HIV-1 activity
Valerian
Inconclusive data; “traditional use only” for restful sleep.
Can’t have everything!
Share This Post
-
Better With Age – by Dr. Alan Castel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one isn’t about the biology of aging, so much as (as the subtitle promises) the psychology of it.
Dr. Castel first covers the grounds of what “successful aging” is, and the benefits that can be expected from doing it right. Spoiler, it’s not just “reduced decline”, there are numerous things that actually get better, too.
We also learn how our memory works differently—it can be worse, of course, but it can also be just different, in a way that tends to tie in with vastness of the accumulated knowledge over the years, allowing for easiest access to the things the brain thinks are most important—ranging from expertise in a certain field, to life-experience “wisdom”.
There’s a lot of advice that’s mostly not going to be anything new to regular readers of 10almonds, in terms of staying sharp with an active lifestyle and a well-nourished brain.
The style is very soft pop-science; there are citations dotted throughout, but mostly this is more of a “curl up with a book” book, not a textbook.
In the category of subjective criticism, it can be a little repetitive (but for those who like repetition for ease of learning, you will love this), and his name-dropping habit gets quite eyeroll-worthy quite quickly.
Bottom line: if you’d like to learn about the very many ways in which “over the hill” is simply defeatist pessimism, then this book can help you to ensure you do better.
Click here to check out Better With Age, and get better with age!
Share This Post
-
The Purple Parsnip’s Bioactive Brain Benefits (& more)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Root Might Be A Guardian Angel
Sometimes we go searching for supplements to research; sometimes supplements present themselves for examination! In this case, our attention was grabbed by a headline:
Angelica gigas extract emerges as a potential treatment for vascular disease
Angelica who?
Angelica gigas, also called the purple parsnip (amongst other names), is a flowering plant native to Korea. It has assorted medicinal properties, and in this case, it was its heart-healthy benefits that were making news:
❝Ultimately, this study presents clearly evidence that Angelica gigas extract is a promising natural product-based functional food/herbal medicine candidate for preventing or regulating hyperlipidemic cardiovascular complications❞
But it has a lot more to offer…
The root has various bioactive metabolites, but the compounds that most studies are most interested in are decursin and decursinol, for their neuroprotective and cognitive enhancement effects:
❝[C]rude extracts and isolated components from the root of A. gigas exhibited neuroprotective and cognitive enhancement effects.
Neuronal damage or death is the most important factor for many neurodegenerative diseases.
In addition, recent studies have clearly demonstrated the possible mechanisms behind the neuroprotective action of extracts/compounds from the root of A. gigas.❞
That middle paragraph there? That’s one of the main pathogenic processes of Alzheimer’s, Parkinson’s, Huntington’s, and Multiple Sclerosis.
Angelica gigas attenuates (reduces the force of) that process:
❝The published reports revealed that the extracts and isolated components from the root of A. gigas showed neuroprotective and cognitive enhancement properties through various mechanisms such as anti-apoptosis, antioxidative actions, inhibiting mRNA and protein expressions of inflammatory mediators and regulating a number of signaling pathways.
In conclusion, the A. gigas root can serve as an effective neuroprotective agent by modulating various pathophysiological processes❞
Read more: Neuroprotective and Cognitive Enhancement Potentials of Angelica gigas Nakai Root: A Review
Beyond neuroprotection & cognitive enhancement
…and also beyond its protection against vascular disease, which is what got our attention…
Angelica gigas also has antioxidant properties, anti-cancer properties, and general immune-boosting properties.
We’ve only so much room, so: those links above will take you to example studies for those things, but there are plenty more where they came from, so we’re quite confident in this one.
Of course, what has antioxidant properties is usually anti-inflammatory, anti-cancer, and anti-aging, because these things are reliant on many of the same processes as each other, with a lot of overlap.
Where can we get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Share This Post
Related Posts
-
Probiotics & Gas/Bloating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I read about probiotics and got myself some from amazon but having started them, now I have a lot of gas, is this normal?❞
As Tom Jones would say: it’s not unusual.
However, it’s also not necessary, and it is easy enough to get past!
And probiotics certainly have their place; see: How Much Difference Do Probiotic Supplements Make, Really?
What’s going on with your gas is…
We interrupt this article to bring back attention to our regular legal/medical disclaimer; please do remember that we can only speak in general health terms, cannot diagnose you, nor make any firm assurances about your health, nor prescribe treatment. What we can do is share information that we hope is educational, and if it helps you, so much the better. Always speak to your own doctor if you have concerns about your health.
Now, back to the article,,,
What’s going on with your gas is most probably what happens for a lot of people: you’ve just put a lot of bacteria into your gut, and congratulations, they survived (which is definitely not a given, more on that later, but their survival is what you wanted), and they are now thriving sufficiently that the output of their respiratory processes is tangible to you—in the form of abdominal bloating/gas.
Because your gut is a semi-closed system (literally there’s an opening at both ends, but it’s mostly quite self-contained in terms of its ecosystem, unless you have leaky gut syndrome, which is Very Bad™), this will generally fix itself within a few days at most—perhaps it even has by the time you’re reading this.
How does it fix itself you wonder? Because there’s only enough resources to sustain so many bacteria, what happens when we take a probiotic supplement (or food) is initially an overload of more bacteria than the gut can support (because unless you recently took antibiotics, the gut is pretty much always running at maximum capacity, because the bacteria there have no evolutionary reason to leave room for newcomers; they just multiply as best they can until the resources run out), and then the excess (i.e., those that are in excess of how many your gut can support) will die, and then the numbers will be back to normal.
Note: the numbers will be back to normal. However, that doesn’t mean the probiotics did nothing—what you’ve done is add diversity, and specifically, you’ve made it so that percentage-wise, you now have slightly more “good” bacteria in the balance than you did previously.
So, unless there are factors out of the ordinary: this is all usually self-correcting quite quickly.
Tips to make things go as smoothly as possible
Firstly, pay attention to recommended doses. If you take one, and think “that was delicious; I’ll have six more” then the initial effect will be a lot more than six times stronger, because of the nature of how bacteria multiply (i.e. exponentially) within minutes of reaching your gut.
Again, this will normally self-correct, but there’s no reason to cause yourself discomfort unnecessarily.
Secondly, if you take probiotics and do not get even a little gas or abdominal bloating even just a little bit, even just briefly… Then probably one of two things happened:
- The probiotics were dead on arrival (i.e. the supplement was a dud, or a “live culture” product in fact died before it got to you)
- The probiotics were fine, but your gut wasn’t prepared for them, and they died upon arrival
The latter happens a lot, especially if the current gut health is not good. What your probiotics need to survive (and bear in mind, because of their life cycle, they need this in minutes of arrival, which is their multiply-or-die-out window), is:
- Fiber, especially insoluble fiber
- In a place they can get at it (i.e. it was the most recent thing you ate, and is not several feet further down your intestines)
- Not too crowded with competitors (i.e. you just ate it, not last night)
Thus, it can be best to take probiotics on a mostly-empty stomach after enjoying a fibrous snack.
See also: What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
And for that matter: Stop Sabotaging Your Gut ← this covers some common probiotics mistakes/problems
If you’d rather take them on an entirely empty stomach, look for probiotic supplements that come with their own prebiotic fiber (usually inulin); these are often marketed as “symbiotics”.
We don’t sell them, but here’s an example product on Amazon for your convenience 😎
Another thing to bear in mind is that there is (unless your case is unusual) no reason to take the same kind of probiotic for more than one course (i.e. one container of however many servings it has). This is because one of two things will be the case:
- The probiotic worked, in which case, you now have thriving colonies of the bacterial species that that supplement provided
- The probiotic didn’t work, in which case, why buy that one again?
So, if supplementing with probiotics, it can be good to do so with new brand each time, with a gap in between each for your gut to get used to the new order of things.
Finally, if you’re making any drastic dietary change, likely this will result in similar gut disturbances.
In particular, if you are moving away from foods that feed C. albicans (the bad fungus that puts holes in your gut), then it will object strongly, cause you to crave sugar/flour/alcohol/etc, give you mood swings, and generally remind you that it has its roots firmly embedded in your nervous system. If that happens, don’t listen to it; it’s just its death throes and it’ll quieten down soon.
You can read more about that here:
Making Friends With Your Gut (You Can Thank Us Later)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
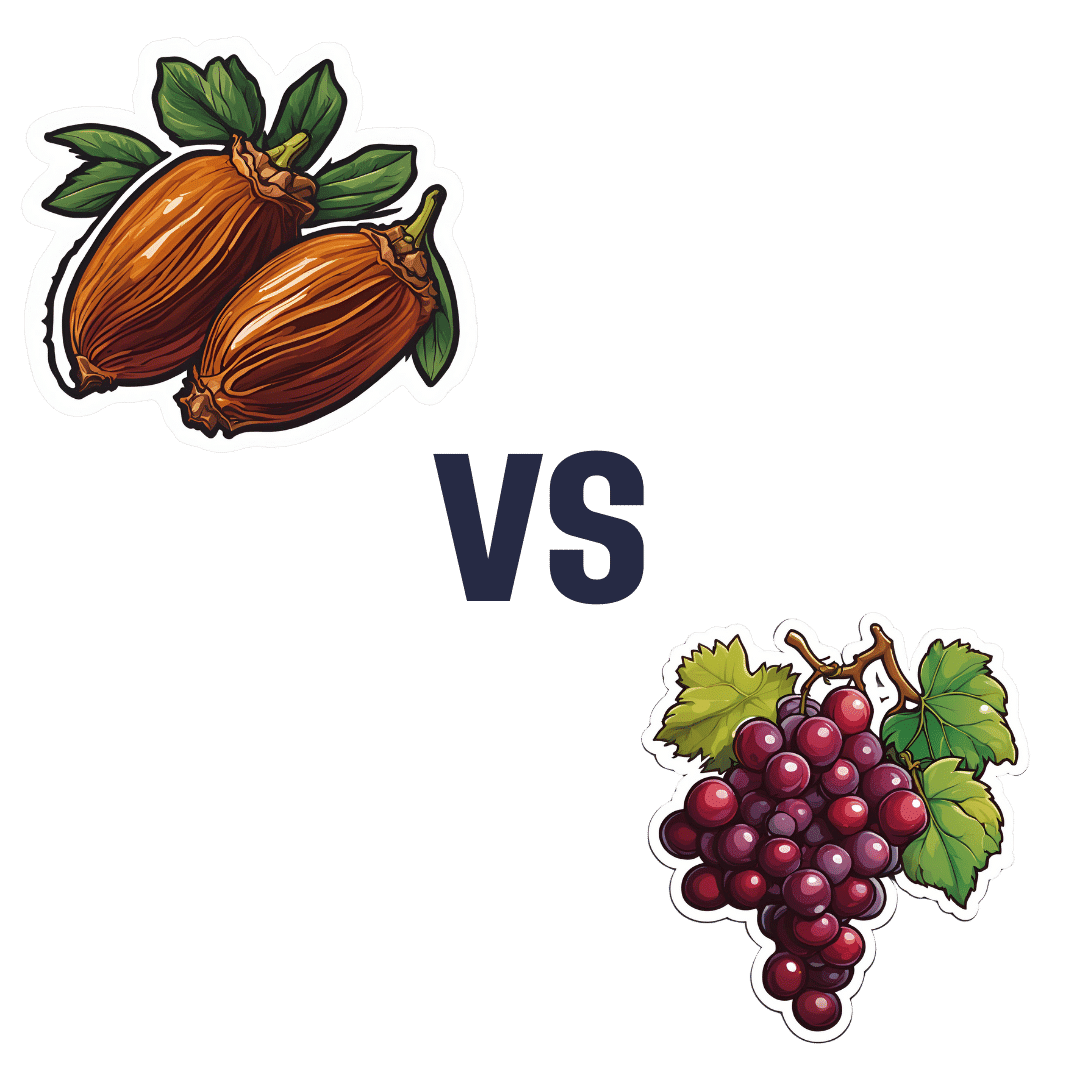
Dates vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to grapes, we picked the dates.
Why?
It’s not close:
In terms of macros, dates have 4x the carbs and/but 8x the fiber, making for the lower glycemic index. Also, for what it’s worth, they have nearly 4x the protein, but probably nobody is eating either of these fruits for the protein. In any case, it’s an easy and clear win for dates in the category of macros.
In the category of vitamins, dates have more of vitamins B2, B3, B5, B6, B9, and choline, while grapes have more of vitamins B1, C, E, and K, making for a 6:4 win for dates.
When it comes to minerals, it’s more one-sided: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. An easy win for dates here.
Of course, enjoy either or both (diversity is good), but if you’re looking for nutrient density, dates are where it’s at.
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cottage cheese is back and all over TikTok. Two dietitians explain why social media’s obsessed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might remember cottage cheese from your childhood. Back then, it was considered “diet food”. You ate it out of the tub, with celery or spread it on crackers for a low-calorie snack. Then cottage cheese went out of fashion.
But cottage cheese is having a resurgence. In recent months, Google searches for “cottage cheese” have risen to the highest levels since 2004.
Social media influencers have been promoting its benefits on TikTok and Instagram with hashtags such as #cottagecheese, #cottagecheeseforlife, and #cottagecheeserecipe. Sales of cottage cheese around the world have skyrocketed.
Let’s see why cottage cheese is having such a moment.
Karolina Kaboompics/Pexels What is cottage cheese?
Cottage cheese is a fresh dairy cheese product with a mild flavour and a slightly tangy taste. It is made by curdling cow’s milk, then draining the whey, leaving behind the curds. These curds are usually small and lumpy, and the texture can vary from creamy to dry, depending on the amount of whey left in the cheese.
The term “cottage cheese” is said to have originated because the cheese was generally made in cottage-type houses from leftover milk, after making butter.
Cottage cheese is cheap, costing about A$12 per kilogram in the supermarket, similar to ricotta cheese.
It’s also surprisingly simple to make at home using freely available recipes. All you need is milk, salt and a splash of vinegar.
We’re using cottage cheese in new ways
It’s difficult to know what started the latest cottage cheese trend. But the creativity of social media means people are sharing alternative ways to use cottage cheese, changing people’s views from it being boring and lacking flavour to it being versatile and healthy.
People are spreading cottage cheese on toast and using it to make dishes such as porridge, dips, salads, bread and flatbreads. They’re using it in cakes and scones, and in desserts such as mousse and ice cream.
Is cottage cheese healthy?
Compared with other cheeses, cottage cheese is low in fat and therefore energy (kilojoules or kJ). This makes it a smart choice for people looking to cut down on their daily energy intake.
For example, 100 grams of cottage cheese contains about 556kJ. The same amount of cheddar contains 1,254kJ and parmesan 1,565kJ.
Many cheeses are rich in protein but they often contain higher amounts of kilojoules due to their fat content. But cottage cheese has substantial amounts of protein with fewer kilojoules.
This makes cottage cheese an ideal option for people aiming to maximise their protein intake without eating large amounts of kilojoules.
Some 100g of cottage cheese provides 17g protein. This is about the same found in three eggs, 60g chicken breast or 320 millilitres (about 300g) full-fat yoghurt.
People are sharing images of their cottage cheese creations on TikTok and Instagram. New Africa/Shutterstock Cottage cheese also contains high levels of vitamin B12 (important for healthy brain function), riboflavin (supports healthy skin and eyes), phosphorus (helps build strong bones and teeth) and folate (essential for cell growth).
However, cottage cheese is lower in calcium compared with other cheeses. It contains just 89 milligrams per 100g. This compares with parmesan (948mg), haloumi (620mg) and ricotta (170mg).
You’ve convinced me. How can I use cottage cheese?
Beyond its excellent nutrition profile, the resurgence of cottage cheese is enabling people to experiment in the kitchen. Its neutral flavour and varied textures – ranging from smooth to chunky – makes it suitable for a range of dishes, from sweet to savoury.
TikTok and Instagram have some great recipes. You could start with an old faithful recipe of celery and cottage cheese, and work your way towards new options such as cottage cheese ice cream.
The healthiest recipes will be those that combine cottage cheese with wholefoods such as fruits, vegetables, nuts and seeds, and lean protein sources.
For instance, you can make a cottage cheese wrap then fill it with vegetables and a lean source of protein (such as chicken or fish).
Other combinations include cottage cheese salad dressings, vegetable dips and egg salads.
Cottage cheese’s rise in popularity is well deserved. Including more cottage cheese in your diet is a smart choice for getting a high dose of protein without adding processed ingredients or too much energy. Embrace the trend and get creative in the kitchen.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: