Blood-Sugar Balancing Beetroot Cutlets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These beetroot cutlets are meaty and proteinous and fibrous and even have a healthy collection of fats, making these much better for your heart and blood than an animal-based equivalent.
You will need
- 1 can kidney beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- ½ cup chopped roasted or steamed beetroot, blotted dry
- ½ cup chopped walnuts (if allergic, substitute with ¼ cup pumpkin seeds)
- ½ cup cooked (ideally: mixed) grains of your choice (if you need gluten-free, there are plenty of gluten-free grains and pseudocereals)
- ¼ cup finely chopped onion
- ¼ bulb garlic, minced or crushed
- 2 tbsp nutritional yeast
- 2 tbsp ground flaxseeds
- 2 tbsp ground chia seeds
- 2 tsp tomato purée
- 1 tsp black pepper
- ½ tsp white miso paste
- ½ tsp smoked paprika
- ½ tsp cayenne pepper
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Combine the beetroot, beans, walnuts, grains, and onion in a food processor, and process until a coarse even mixture.
2) Add the remaining ingredients and process to mix thoroughly.
3) Transfer the mixture to a clean work surface and divide into six balls. If the structural integrity is not good (i.e. too soft), add a little more of any or all of these ingredients: chopped walnuts, ground flax, ground chia, nutritional yeast.
4) Press the balls firmly into cutlets, and refrigerate for at least 1 hour, but longer is even better if you have the time. Alternatively, if you’d like to freeze them for later use, then this is the point at which to do that.
5) Preheat the oven to 375℉ / 190℃.
6) Roast the cutlets on a baking tray lined with baking paper, for about 30 minutes, turning over carefully with a spatula halfway through. They should be firm when done; if they’re not, give them a little longer.
7) Serve hot, for example on a bed of greens and with a drizzle of aged balsamic vinegar.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Beetroot’s Many Benefits
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Omega-3 Fatty Acids Really Do For Us
- Three Daily Servings of Beans?
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
At first, suncreams helped you ‘tan with ease’
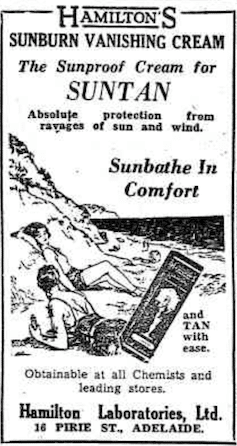
This early sunscreen claimed you could ‘tan with ease’.
Trove/NLASunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
This 1967 Coppertone advertisement urged you to ‘tan, not burn’.
SenseiAlan/Flickr, CC BY-SASunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
-
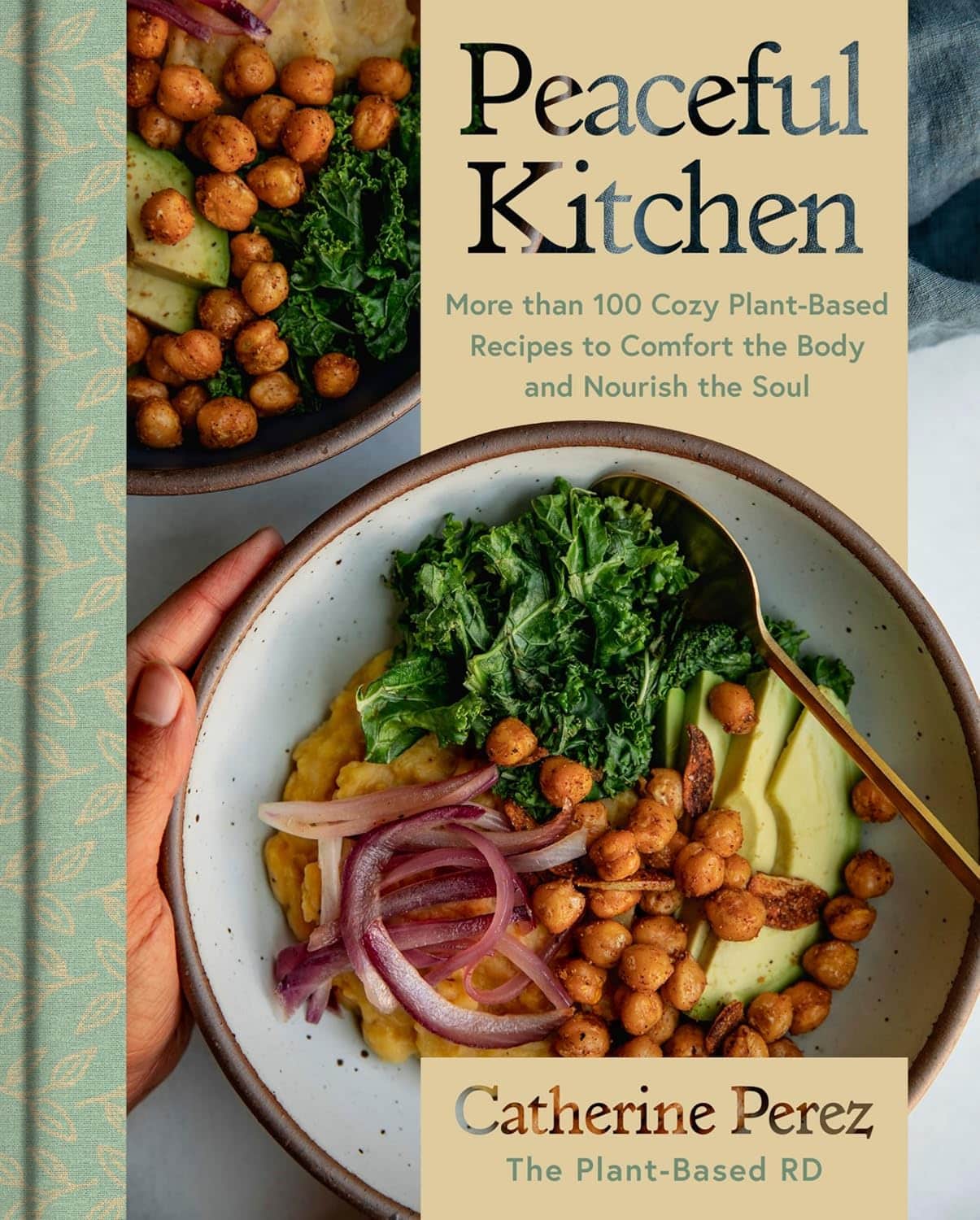
Peaceful Kitchen – by Catherine Perez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a keen cook and Registered Dietician with a Master’s in same, covers the basics of the science of nutrition as relevant to her recipes, but first and foremost this is not a science textbook—it’s a cookbook, and its pages contain more love for the art than citations for the (perfectly respectable) science.
Mexican and Dominican cuisine are the main influences in this book, but there are dishes from around the world too.
The recipes themselves are… Comparable in difficulty to the things we often feature in our recipes section here at 10almonds. They’re probably not winning any restaurants Michelin stars, but they’re not exactly student survival recipes either. They’re made from mostly non-obscure whole foods, nutritionally-dense ingredients at that, with minimal processed foods involved.
That said, she does take a “add, don’t subtract” approach to nutrition, i.e. focussing more on adding in diversity of plants than on “don’t eat this; don’t eat that” mandates.
If there’s any criticism to be levelled at the book, it’s that in most cases we’d multiply the spices severalfold, but that’s not a big problem as readers can always judge that individually; she’s given the basic information of which spices in which proportions, which is the key knowledge.
Bottom line: if you’re looking to expand your plant-based cooking repertoire, this one is a fine choice.
Click here to check out Peaceful Kitchen, and try some new things!
Share This Post
-
Kiwi vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to passion fruit, we picked the passion fruit.
Why?
This fruit is so passionate about delivery nutrient-dense goodness, that at time of writing, nothing has beaten it yet!
In terms of macros, passion fruit has a little more protein, as well as 50% more carbs, and/but more than 3x the fiber. That last stat is particularly impressive, and also results in passion fruit having a much lower glycemic index, too. In short, a clear win for passion fruit in the macros category.
In the category of vitamins, kiwi has more of vitamins B9, C, E, and K, while passion fruit has more of vitamins A, B2, B3, and B6, making for a tie this time.
As for minerals, kiwi has more calcium, copper, manganese, and zinc, while passion fruit has more iron, magnesium, phosphorus, potassium, and selenium, resulting in a modest, marginal win for passion fruit in this category.
Adding up the categories gives a convincing win for passion fruit, but by all means enjoy either or both; diversity is good! And kiwi has its merits too (for example, it’s particularly high in vitamin K, appropriately enough).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
Related Posts
-
Pumpkin Protein Crackers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ten of these (give or take what size you make them) will give you the 20g protein that most people’s body’s can use at a time. Five of these plus some of one of the dips we list at the bottom will also do it:
You will need
- 1 cup chickpea flour (also called gram flour or garbanzo bean flour)
- 2 tbsp pumpkin seeds
- 1 tbsp chia seeds
- 1 tsp baking powder
- ¼ tsp MSG or ½ tsp low-sodium salt
- 2 tbsp extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Combine the dry ingredients in a mixing bowl, and mix thoroughly.
3) Add the oil, and mix thoroughly.
4) Add water, 1 tbsp at a time, mixing thoroughly until the mixture comes together and you have a dough ball. You’ll probably need 3–4 tbsp in total, but do add them one at a time.
5) Roll out the dough as thinly and evenly as you can between two sheets of baking paper. Remove the top layer of the paper, and slice the dough into squares or triangles. You could use a cookie-cutter to make other shapes if you like, but then you’ll need to repeat the rolling to use up the offcuts. So we recommend squares or triangles at least for your first go.
6) Bake them in the oven for 12–15 minutes or until golden and crispy. Enjoy immediately or keep in an airtight container.
Enjoy!
Want to learn more?
For those interested in some things to go with what we have going on today:
- Muhammara ← this is a very nutritionally-dense dip (not to mention tasty; seriously, check out these flavors)
- Hero Homemade Hummus ← a classic
- Plant-Based Healthy Cream Cheese ← also a very respectable option
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
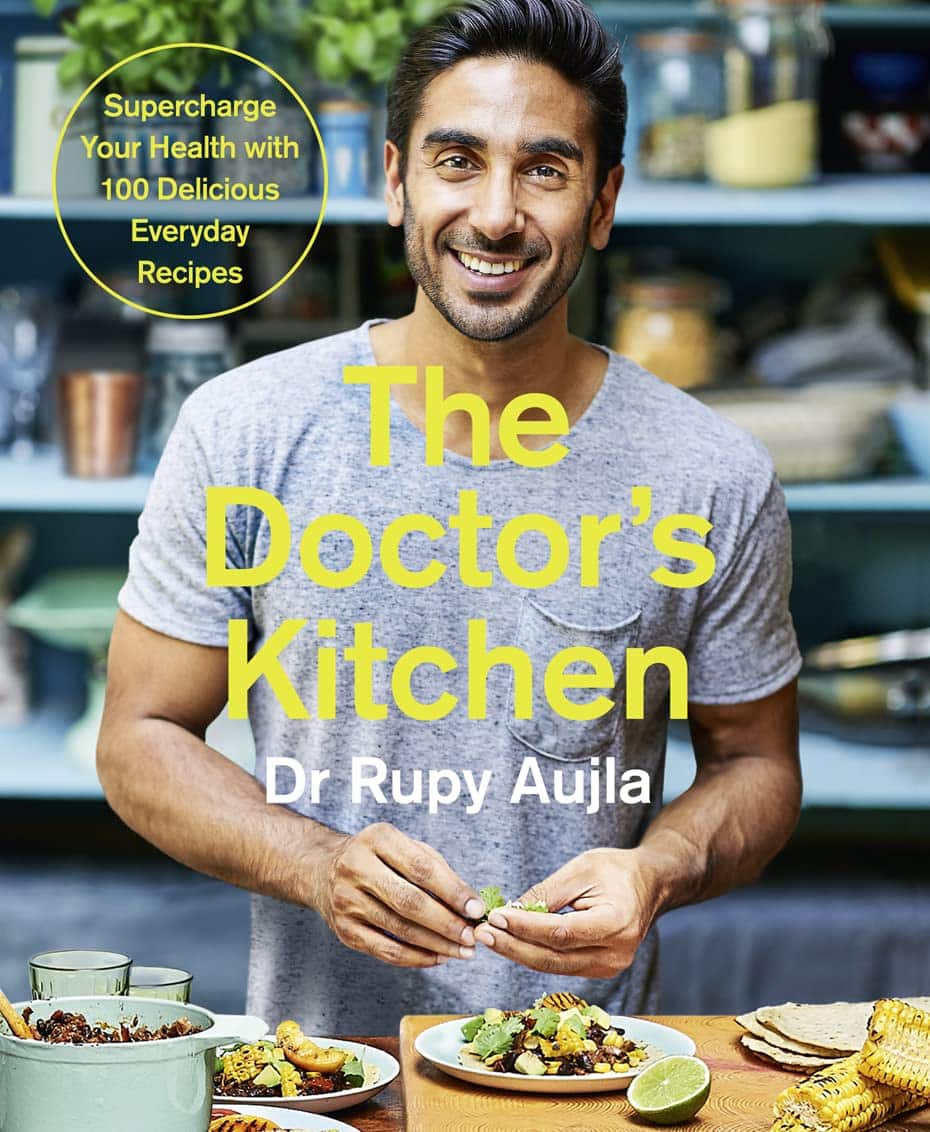
The Doctor’s Kitchen – by Dr. Rupy Aujla
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured Dr. Aujla before as an expert-of-the-week, and now it’s time to review a book by him. What’s his deal, and what should you expect?
Dr. Aujla first outlines the case for food as medicine. Not just “eat nutritionally balanced meals”, but literally, “here are the medicinal properties of these plants”. Think of some of the herbs and spices we’ve featured in our Monday Research Reviews, and add in medicinal properties of cancer-fighting cruciferous vegetables, bananas with dopamine and dopamine precursors, berries full of polyphenols, hemp seeds that fight cognitive decline, and so forth.
Most of the book is given over to recipes. They’re plant-centric, but mostly not vegan. They’re consistent with the Mediterranean diet, but mostly Indian. They’re economically mindful (favoring cheap ingredients where reasonable) while giving a nod to where an extra dollar will elevate the meal. They don’t give calorie values etc—this is a feature not a bug, as Dr. Aujla is of the “positive dieting” camp that advocates for us to “count colors, not calories”. Which, we have to admit, makes for very stress-free cooking, too.
Dr. Aujla is himself an Indian Brit, by the way, which gives him two intersecting factors for having a taste for spices. If you don’t share that taste, just go easier on the pepper etc.
As for the medicinal properties we mentioned up top? Four pages of references at the back, for any who are curious to look up the science of them. We at 10almonds do love references!
Bottom line: if you like tasty food and you’re looking for a one-stop, well-rounded, food-as-medicine cookbook, this one is a top-tier choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: