What’s Keeping the US From Allowing Better Sunscreens?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When dermatologist Adewole “Ade” Adamson sees people spritzing sunscreen as if it’s cologne at the pool where he lives in Austin, Texas, he wants to intervene. “My wife says I shouldn’t,” he said, “even though most people rarely use enough sunscreen.”
At issue is not just whether people are using enough sunscreen, but what ingredients are in it.
The Food and Drug Administration’s ability to approve the chemical filters in sunscreens that are sold in countries such as Japan, South Korea, and France is hamstrung by a 1938 U.S. law that has required sunscreens to be tested on animals and classified as drugs, rather than as cosmetics as they are in much of the world. So Americans are not likely to get those better sunscreens — which block the ultraviolet rays that can cause skin cancer and lead to wrinkles — in time for this summer, or even the next.
Sunscreen makers say that requirement is unfair because companies including BASF Corp. and L’Oréal, which make the newer sunscreen chemicals, submitted safety data on sunscreen chemicals to the European Union authorities some 20 years ago.
Steven Goldberg, a retired vice president of BASF, said companies are wary of the FDA process because of the cost and their fear that additional animal testing could ignite a consumer backlash in the European Union, which bans animal testing of cosmetics, including sunscreen. The companies are asking Congress to change the testing requirements before they take steps to enter the U.S. marketplace.
In a rare example of bipartisanship last summer, Sen. Mike Lee (R-Utah) thanked Rep. Alexandria Ocasio-Cortez (D-N.Y.) for urging the FDA to speed up approvals of new, more effective sunscreen ingredients. Now a bipartisan bill is pending in the House that would require the FDA to allow non-animal testing.
“It goes back to sunscreens being classified as over-the-counter drugs,” said Carl D’Ruiz, a senior manager at DSM-Firmenich, a Switzerland-based maker of sunscreen chemicals. “It’s really about giving the U.S. consumer something that the rest of the world has. People aren’t dying from using sunscreen. They’re dying from melanoma.”
Every hour, at least two people die of skin cancer in the United States. Skin cancer is the most common cancer in America, and 6.1 million adults are treated each year for basal cell and squamous cell carcinomas, according to the Centers for Disease Control and Prevention. The nation’s second-most-common cancer, breast cancer, is diagnosed about 300,000 times annually, though it is far more deadly.
Dermatologists Offer Tips on Keeping Skin Safe and Healthy
– Stay in the shade during peak sunlight hours, 10 a.m. to 4 p.m. daylight time.– Wear hats and sunglasses.– Use UV-blocking sun umbrellas and clothing.– Reapply sunscreen every two hours.You can order overseas versions of sunscreens from online pharmacies such as Cocooncenter in France. Keep in mind that the same brands may have different ingredients if sold in U.S. stores. But importing your sunscreen may not be affordable or practical. “The best sunscreen is the one that you will use over and over again,” said Jane Yoo, a New York City dermatologist.
Though skin cancer treatment success rates are excellent, 1 in 5 Americans will develop skin cancer by age 70. The disease costs the health care system $8.9 billion a year, according to CDC researchers. One study found that the annual cost of treating skin cancer in the United States more than doubled from 2002 to 2011, while the average annual cost for all other cancers increased by just 25%. And unlike many other cancers, most forms of skin cancer can largely be prevented — by using sunscreens and taking other precautions.
But a heavy dose of misinformation has permeated the sunscreen debate, and some people question the safety of sunscreens sold in the United States, which they deride as “chemical” sunscreens. These sunscreen opponents prefer “physical” or “mineral” sunscreens, such as zinc oxide, even though all sunscreen ingredients are chemicals.
“It’s an artificial categorization,” said E. Dennis Bashaw, a retired FDA official who ran the agency’s clinical pharmacology division that studies sunscreens.
Still, such concerns were partly fed by the FDA itself after it published a study that said some sunscreen ingredients had been found in trace amounts in human bloodstreams. When the FDA said in 2019, and then again two years later, that older sunscreen ingredients needed to be studied more to see if they were safe, sunscreen opponents saw an opening, said Nadim Shaath, president of Alpha Research & Development, which imports chemicals used in cosmetics.
“That’s why we have extreme groups and people who aren’t well informed thinking that something penetrating the skin is the end of the world,” Shaath said. “Anything you put on your skin or eat is absorbed.”
Adamson, the Austin dermatologist, said some sunscreen ingredients have been used for 30 years without any population-level evidence that they have harmed anyone. “The issue for me isn’t the safety of the sunscreens we have,” he said. “It’s that some of the chemical sunscreens aren’t as broad spectrum as they could be, meaning they do not block UVA as well. This could be alleviated by the FDA allowing new ingredients.”
Ultraviolet radiation falls between X-rays and visible light on the electromagnetic spectrum. Most of the UV rays that people come in contact with are UVA rays that can penetrate the middle layer of the skin and that cause up to 90% of skin aging, along with a smaller amount of UVB rays that are responsible for sunburns.
The sun protection factor, or SPF, rating on American sunscreen bottles denotes only a sunscreen’s ability to block UVB rays. Although American sunscreens labeled “broad spectrum” should, in theory, block UVA light, some studies have shown they fail to meet the European Union’s higher UVA-blocking standards.
“It looks like a number of these newer chemicals have a better safety profile in addition to better UVA protection,” said David Andrews, deputy director of Environmental Working Group, a nonprofit that researches the ingredients in consumer products. “We have asked the FDA to consider allowing market access.”
The FDA defends its review process and its call for tests of the sunscreens sold in American stores as a way to ensure the safety of products that many people use daily, rather than just a few times a year at the beach.
“Many Americans today rely on sunscreens as a key part of their skin cancer prevention strategy, which makes satisfactory evidence of both safety and effectiveness of these products critical for public health,” Cherie Duvall-Jones, an FDA spokesperson, wrote in an email.
D’Ruiz’s company, DSM-Firmenich, is the only one currently seeking to have a new over-the-counter sunscreen ingredient approved in the United States. The company has spent the past 20 years trying to gain approval for bemotrizinol, a process D’Ruiz said has cost $18 million and has advanced fitfully, despite attempts by Congress in 2014 and 2020 to speed along applications for new UV filters.
Bemotrizinol is the bedrock ingredient in nearly all European and Asian sunscreens, including those by the South Korean brand Beauty of Joseon and Bioré, a Japanese brand.
D’Ruiz said bemotrizinol could secure FDA approval by the end of 2025. If it does, he said, bemotrizinol would be the most vetted and safest sunscreen ingredient on the market, outperforming even the safety profiles of zinc oxide and titanium dioxide.
As Congress and the FDA debate, many Americans have taken to importing their own sunscreens from Asia or Europe, despite the risk of fake products.
“The sunscreen issue has gotten people to see that you can be unsafe if you’re too slow,” said Alex Tabarrok, a professor of economics at George Mason University. “The FDA is just incredibly slow. They’ve been looking at this now literally for 40 years. Congress has ordered them to do it, and they still haven’t done it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Avoiding/Managing Osteoarthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Osteoarthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation).
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
Some forms, such as rheumatoid arthritis, are of the inflammatory kind. We wrote about that previously:
See: Avoiding/Managing Rheumatoid Arthritis
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause.
So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can; it’s just not the prime focus.
So, what should we focus on?
First and foremost: avoiding wear-and-tear if possible. Naturally, we all must live our lives, and sometimes that means taking a few knocks, and definitely it means using our joints. An unused joint would suffer just as much as an abused one. But, we can take care of our joints!
We wrote on that previously, too:
See: How To Really Look After Your Joints
New osteoarthritis medication (hot off the press!)
At 10almonds, we try to keep on top of new developments, and here’s a shiny new one from this month:
- Methotrexate to treat hand osteoarthritis with synovitis (12th Oct, clinical trial)
- New research has found an existing drug could help many people with painful hand osteoarthritis (24th Oct, pop-science article about the above, but still written by one of the study authors!)
Note also that Dr. Flavia Cicuttini there talks about what we talked about above—that calling it non-inflammatory arthritis is a little misleading, as the inflammation still occurs.
And finally…
You might consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though!
- Rest—while keeping mobility going.
- Mobility aids—if it helps, it helps.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility.
- Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
See: Managing Chronic Pain (Realistically!)
Take good care of yourself!
Share This Post
-
On This Bright Day – by Dr. Susan Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is principally aimed at those who have struggled with emotional/comfort eating, over-eating, and/or compulsive eating of some kind.
However, its advices go for the “little compulsions” too, the many small unhealthy choices that add up. Thus, this book has value for most if not all of us.
The format is: each day has a little quotation, followed by a short discussion of that, which is then underlined by an affirmation for the day.
The main thrust of the book is to promote mindful eating, and it does this well with daily reminders that are helpful without being preachy.
Bottom line: if you enjoy “daily reader” type books and would like a daily reminder to practice mindful eating, then this book is for you!
Click here to check out On This Bright Day, and enjoy your food mindfully, every day!
Share This Post
-
The Fiber Effect – by Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a registered dietician-nutritionist (RDN), brings to this work her decades of professional experience specializing in heart disease, diabetes, sports nutrition, and women’s health—and it shows.
The main premise is, of course “eat more fiber”, but she also talks us through what happens if we don’t, and how very many people (including 95% of Americans) suffer the consequences of a fiber-deficient diet, usually without even knowing that that’s the reason.
This book details the many different kinds of fiber (which is one of the reasons for consuming a wide variety of plants, not just one or two star-performers), what they do, what we need to prioritize for what, and more.
The recipes, of which there are 40 (enough to furnish us with a 14-day meal plan, which she does) are plant-based and varied.
The style is energetic and friendly, with plenty of (well-referenced) scientific information, but little-to-no jargon.
Bottom line: if you’d like to improve your fiber intake, then this book can help you supercharge that!
Click here to check out The Fiber Effect, and feel the difference!
Share This Post
Related Posts
-
A Correction, And A New, Natural Way To Boost Daily Energy Levels
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
First: a correction and expansion!
After yesterday’s issue of 10almonds covering breast cancer risks and checks, a subscriber wrote to say, with regard to our opening statement, which was:
“Anyone (who has not had a double mastectomy, anyway) can get breast cancer”
❝I have been enjoying your newsletter. This statement is misleading and should have a disclaimer that says even someone who has had a double mastectomy can get breast cancer, again. It is true and nothing…nothing is 100% including a mastectomy. I am a 12 year “thriver” (I don’t like to use the term survivor) who has had a double mastectomy. I work with a local hospital to help newly diagnosed patients deal with their cancer diagnosis and the many decisions that follow. A double mastectomy can help keep recurrence from happening but there are no guarantees. I tried to just delete this and let it go but it doesn’t feel right. Thank you!❞
Thank you for writing in about this! We wouldn’t want to mislead, and we’re always glad to hear from people who have been living with conditions for a long time, as (assuming they are a person inclined to learning) they will generally know topics far more deeply than someone who has researched it for a short period of time.
Regards a double mastectomy (we’re sure you know this already, but noting here for greater awareness, prompted by your message), a lot of circumstances can vary. For example, how far did a given cancer spread, and especially, did it spread to the lymph nodes at the armpits? And what tissue was (and wasn’t) removed?
Sometimes a bilateral prophylactic mastectomy will leave the lymph nodes partially or entirely intact, and a cancer could indeed come back, if not every last cancerous cell was removed.
A total double mastectomy, by definition, should have removed all tissue that could qualify as breast tissue for a breast cancer, including those lymph nodes. However, if the cancer spread unnoticed somewhere else in the body, then again, you’re quite correct, it could come back.
Some people have a double mastectomy without having got cancer first. Either because of a fear of cancer due to a genetic risk (like Angelina Jolie), or for other reasons (like Elliot Page).
This makes a difference, because doing it for reasons of cancer risk may mean surgeons remove the lymph nodes too, while if that wasn’t a factor, surgeons will tend to leave them in place.
In principle, if there is no breast tissue, including lymph nodes, and there was no cancer to spread, then it can be argued that the risk of breast cancer should now be the same “zero” as the risk of getting prostate cancer when one does not have a prostate.
But… Surgeries are not perfect, and everyone’s anatomy and physiology can differ enough from “textbook standard” that surprises can happen, and there’s almost always a non-zero chance of certain health outcomes.
For any unfamiliar, here’s a good starting point for learning about the many types of mastectomy, that we didn’t go into in yesterday’s edition. It’s from the UK’s National Health Service:
NHS: Mastectomy | Types of Mastectomy
And for the more sciency-inclined, here’s a paper about the recurrence rate of cancer after a prophylactic double mastectomy, after a young cancer was found in one breast.
The short version is that the measured incidence rate of breast cancer after prophylactic bilateral mastectomy was zero, but the discussion (including notes about the limitations of the study) is well worth reading:
Breast Cancer after Prophylactic Bilateral Mastectomy in Women with a BRCA1 or BRCA2 Mutation
❝[Can you write about] the availability of geriatric doctors Sometimes I feel my primary isn’t really up on my 70 year old health issues. I would love to find a doctor that understands my issues and is able to explain them to me. Ie; my worsening arthritis in regards to food I eat; in regards to meds vs homeopathic solutions.! Thanks!❞
That’s a great topic, worthy of a main feature! Because in many cases, it’s not just about specialization of skills, but also about empathy, and the gap between studying a condition and living with a condition.
About arthritis, we’re going to do a main feature specifically on that quite soon, but meanwhile, you might like our previous article:
Keep Inflammation At Bay (arthritis being an inflammatory condition)
As for homeopathy, your question prompts our poll today!
(and then we’ll write about that tomorrow)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tastes from our past can spark memories, trigger pain or boost wellbeing. Here’s how to embrace food nostalgia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever tried to bring back fond memories by eating or drinking something unique to that time and place?
It could be a Pina Colada that recalls an island holiday? Or a steaming bowl of pho just like the one you had in Vietnam? Perhaps eating a favourite dish reminds you of a lost loved one – like the sticky date pudding Nanna used to make?
If you have, you have tapped into food-evoked nostalgia.
As researchers, we are exploring how eating and drinking certain things from your past may be important for your mood and mental health.
Halfpoint/Shutterstock Bittersweet longing
First named in 1688 by Swiss medical student, Johannes Hoffer, nostalgia is that bittersweet, sentimental longing for the past. It is experienced universally across different cultures and lifespans from childhood into older age.
But nostalgia does not just involve positive or happy memories – we can also experience nostalgia for sad and unhappy moments in our lives.
In the short and long term, nostalgia can positively impact our health by improving mood and wellbeing, fostering social connection and increasing quality of life. It can also trigger feelings of loneliness or meaninglessness.
We can use nostalgia to turn around a negative mood or enhance our sense of self, meaning and positivity.
Research suggests nostalgia alters activity in the brain regions associated with reward processing – the same areas involved when we seek and receive things we like. This could explain the positive feelings it can bring.
Nostalgia can also increase feelings of loneliness and sadness, particularly if the memories highlight dissatisfaction, grieving, loss, or wistful feelings for the past. This is likely due to activation of brain areas such as the amygdala, responsible for processing emotions and the prefrontal cortex that helps us integrate feelings and memories and regulate emotion.
How to get back there
There are several ways we can trigger or tap into nostalgia.
Conversations with family and friends who have shared experiences, unique objects like photos, and smells can transport us back to old times or places. So can a favourite song or old TV show, reunions with former classmates, even social media posts and anniversaries.
What we eat and drink can trigger food-evoked nostalgia. For instance, when we think of something as “comfort food”, there are likely elements of nostalgia at play.
Foods you found comforting as a child can evoke memories of being cared for and nurtured by loved ones. The form of these foods and the stories we tell about them may have been handed down through generations.
Food-evoked nostalgia can be very powerful because it engages multiple senses: taste, smell, texture, sight and sound. The sense of smell is closely linked to the limbic system in the brain responsible for emotion and memory making food-related memories particularly vivid and emotionally charged.
But, food-evoked nostalgia can also give rise to negative memories, such as of being forced to eat a certain vegetable you disliked as a child, or a food eaten during a sad moment like a loved ones funeral. Understanding why these foods evoke negative memories could help us process and overcome some of our adult food aversions. Encountering these foods in a positive light may help us reframe the memory associated with them.
Just like mum used to make. Food might remind you of the special care you received as a child. Galina Kovalenko/Shutterstock What people told us about food and nostalgia
Recently we interviewed eight Australians and asked them about their experiences with food-evoked nostalgia and the influence on their mood. We wanted to find out whether they experienced food-evoked nostalgia and if so, what foods triggered pleasant and unpleasant memories and feelings for them.
They reported they could use foods that were linked to times in their past to manipulate and influence their mood. Common foods they described as particularly nostalgia triggering were homemade meals, foods from school camp, cultural and ethnic foods, childhood favourites, comfort foods, special treats and snacks they were allowed as children, and holiday or celebration foods. One participant commented:
I guess part of this nostalgia is maybe […] The healing qualities that food has in mental wellbeing. I think food heals for us.
Another explained
I feel really happy, and I guess fortunate to have these kinds of foods that I can turn to, and they have these memories, and I love the feeling of nostalgia and reminiscing and things that remind me of good times.
Yorkshire pudding? Don’t mind if I do. Rigsbyphoto/Shutterstock Understanding food-evoked nostalgia is valuable because it provides us with an insight into how our sensory experiences and emotions intertwine with our memories and identity. While we know a lot about how food triggers nostalgic memories, there is still much to learn about the specific brain areas involved and the differences in food-evoked nostalgia in different cultures.
In the future we may be able to use the science behind food-evoked nostalgia to help people experiencing dementia to tap into lost memories or in psychological therapy to help people reframe negative experiences.
So, if you are ever feeling a little down and want to improve your mood, consider turning to one of your favourite comfort foods that remind you of home, your loved ones or a holiday long ago. Transporting yourself back to those times could help turn things around.
Megan Lee, Senior Teaching Fellow, Psychology, Bond University; Doug Angus, Assistant Professor of Psychology, Bond University, and Kate Simpson, Sessional academic, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
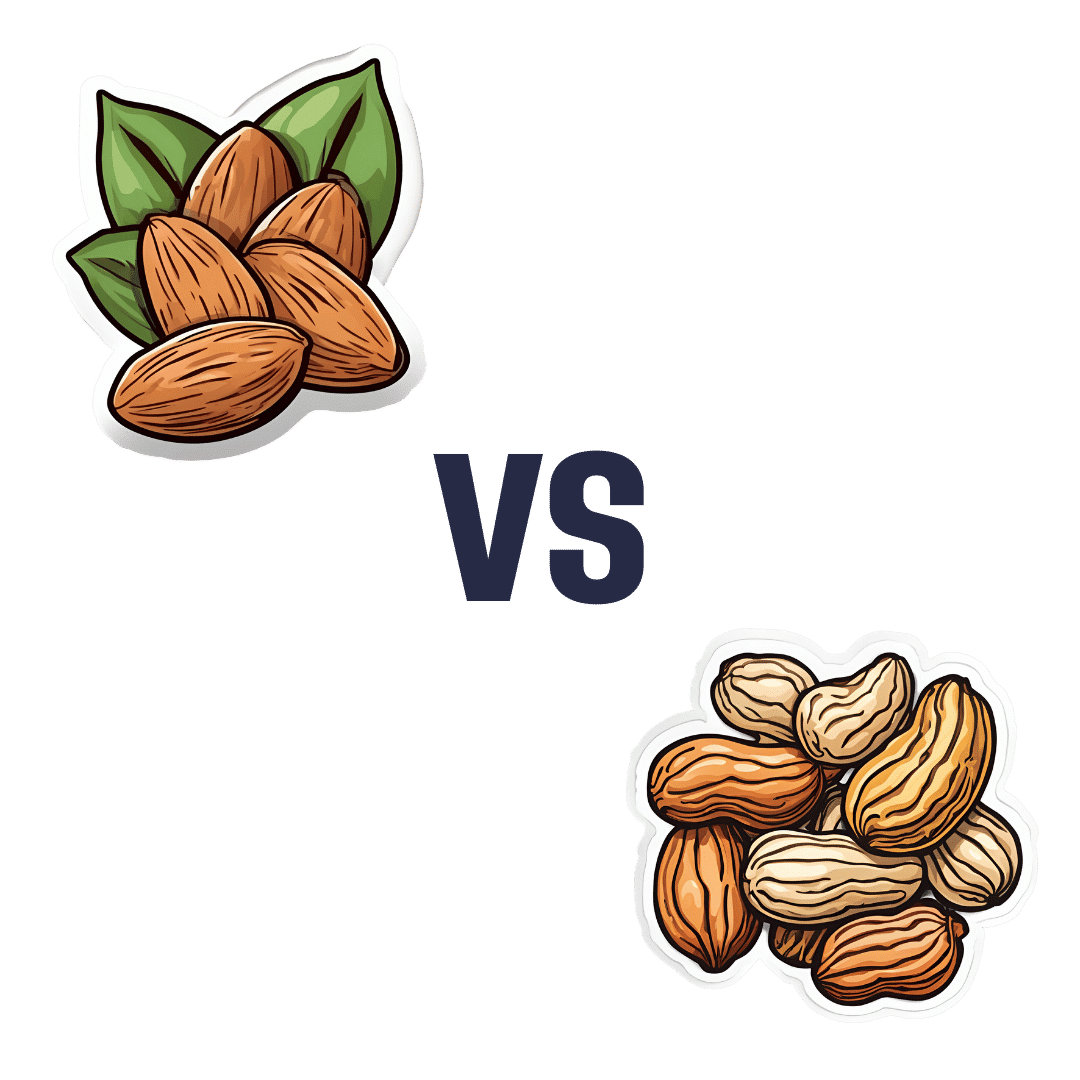
Almonds vs Peanuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to peanuts, we picked the almonds.
Why?
No, it’s not just our pro-almonds bias… But it’s also not as one-sided, nutritionally speaking, as you might think!
In terms of macros, almonds have a lot more fiber, and moderately more carbs, the ratio of which give almonds the lower glycemic index. On the other hand, peanuts have a little more protein. Both of these nuts are equally fatty, but peanuts have the higher saturated fat content. All in all, we say the biggest deciding factor is the fiber, and hand this one to the almonds.
In the category of vitamins, almonds have more of vitamins B2 and E, while peanuts have more of vitamins B1, B3, B5, B6, B7, and B9. An easy win for peanuts this time.
When it comes to minerals, almonds have more calcium, magnesium, manganese, phosphorus, and potassium, while peanuts have more copper, iron, selenium, and zinc. Thus, a 5:4 marginal win for almonds.
Adding up the sections makes for an overall win for almonds, but as you can see, it was close and peanuts certainly have their merits too, so by all means enjoy either or both; diversity is good!
Unless you are allergic, in which case, obviously please don’t do that.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: