Being Mortal – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you want to “live forever or die trying”, and that’s an understandable goal… But are you prepared for “or die trying” being the outcome?
This is not a cheerful book, if you’re anything like this reviewer, you will need a little towel or something to mop up the tears while you read. But it’s worth it.
Dying is one thing; fighting for life is even generally considered a noble endeavor. Suffering alone isn’t fun, losing independence can feel humiliating, and seeing someone who was always a tower of strength, now a frail shadow of their former self, reduced to begging for something that they’re “not allowed”, can be worse.
Do we want that for ourselves? For our loved ones? Can there be a happy medium between that, and the alternative to indeed “go gentle into that good night”?
Dr. Gawande, a surgeon well-acquainted with death and dying, thinks so. But it involves work on our part, and being prepared for hard decisions.
- What is most important to us, and what tradeoffs are we willing to make for it?
- What, even, is actually an option to us with the resources available?
- Can we make peace with a potentially bad lot? And… Should we?
- When is fighting important, and when is it self-destructive?
These (and others) are all difficult questions posed by Dr. Gawande, but critical ones.
We don’t usually quote other people’s reviews when reviewing books here, but let’s consider the following words from the end of a long review on Amazon:
❝If “dying as we lived” is some kind of standard for how we should go, then maybe alone and medicalized makes some sense right now after all.❞
Bottom line: we all deserve better than that. And if we don’t take the time to think about what’s most important, then time will take it from us. This very insightful book may not have all the answers, but it has the questions, and it can help a lot in exploring them and deciding what matters most to us in the end, really.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Grow In Comfort
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Grow (Without Leaving Your Comfort Zone)
“You have to get out of your comfort zone!” we are told, from cradle to grave.
When we are young, we are advised (or sometimes more forcefully instructed!) that we have to try new things. In our middle age, we are expected to be the world’s greatest go-getters, afraid of nothing and always pushing limits. And when we are old, people bid us “don’t be such a dinosaur”.
It is assumed, unquestioned, that growth can only occur through hardship and discomfort.
But what if that’s a discomforting lie?
Butler (2023) posited an idea: “We never achieve success faster and with less effort than when we are in our comfort zone”
Her words are an obvious callback to the ideas of Csikszentmihalyi (1970) in the sense of “flow”, in the sense in which that word is used in psychology.
Flow is: when a person is in a state of energized focus, full involvement, and enjoyment of an activity.
As a necessary truth (i.e: a function of syllogistic logic), the conditions of “in a state of flow” and “outside of one’s comfort zone” cannot overlap.
From there, we can further deduce (again by simple logic) that if flow can be found, and/but cannot be found outside of the comfort zone, then flow can only be found within the comfort zone.
That is indeed comforting, but what about growth?
Imagine you’ve never gone camping in your life, but you want to get outside of your comfort zone, and now’s the time to do it. So, you check out some maps of the Yukon, purchase some camping gear, and off you go into the wilderness. In the event that you survive to report it, you will indeed be able to say “it was not comfortable”.
But, did growth occur? Maybe, but… it’s a folly to say “what doesn’t kill us makes us stronger” as a reason to pursue such things. Firstly, there’s a high chance it may kill us. Secondly, what doesn’t kill us often leaves us incredibly weakened and vulnerable.
When Hannibal famously took his large army of mostly African mercenaries across the Alps during winter to march on Rome from the other side, he lost most of his men on the way, before proceeding to terrorize Northern Italy convincingly with the small remainder. But! Their hard experience hadn’t made them stronger; it had just removed the weaker soldiers, making the resultant formations harder to break.
All this to say, please do not inflict hardship and discomfort and danger in the hopes it’ll make you stronger; it will probably do the opposite.
But…
If, instead of wilderness trekking in the Yukon…
- You start off with a camper van holiday, then you’ll be taking a fair amount of your comfort with you. In effect, you will be stretching and expanding your comfort zone without leaving it.
- Then maybe another year you might try camping in a tent on a well-catered camping site.
- Later, you might try “roughing it” at a much less well-catered camping site.
- And so on.
Congratulations, you have tried new things and undergone growth, taking your comfort zone with you all the way!
This is more than just “easing yourself into” something
It really is about taking your comfort with you too. If you want to take up running, don’t ask “how can I run just a little bit first” or “how can I make it easier” (well, feel free to ask those things too, but) ask yourself: how can I bring my comfort with me? Comfortable shoes, perhaps, an ergonomic water bottle, shade for your head, maybe.
❝Any fool can rough it, but a good soldier can make himself comfortable in any circumstances❞
~ British Army maxim
This goes for more than just physical stuff, too
If you want to learn a new skill, the initial learning curve can be anxiety-inducing, especially if you are taking a course and worried about keeping up or “not being good enough”.
So, “secretly” study in advance, at your leisure, get yourself a head start. Find a degree of comfort in what you’ve learned so far, and then bring that comfort with you into your entry-level course that is now less intimidating.
Discomfort isn’t a badge of honor (and impedes growth)
Take that extra rest stop on the highway. Bring your favorite coffee with you. Use that walking stick, if it helps.
Whatever it takes to bring your comfort with you, bring it.
Trust us, you’ll get further that way.
Share This Post
-
Why does alcohol make my poo go weird?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter the festive season it’s a good time to think about what all those celebratory alcoholic drinks can do to your gut.
Alcohol can interfere with the time it takes for food to go through your gut (also known as the “transit time”). In particular, it can affect the muscles of the stomach and the small bowel (also known as the small intestine).
So, how and why does alcohol make your poos goes weird? Here’s what you need to know.
Diarrhoea and the ‘transit time’
Alcohol’s effect on stomach transit time depends on the alcohol concentration.
In general, alcoholic beverages such as whisky and vodka with high alcohol concentrations (above 15%) slow down the movement of food in the stomach.
Beverages with comparatively low alcohol concentrations (such as wine and beer) speed up the movement of food in the stomach.
These changes in gut transit explain why some people can get a sensation of fullness and abdominal discomfort when they drink vodka or whisky.
How long someone has been drinking a lot of alcohol can affect small bowel transit.
We know from experiments with rats that chronic use of alcohol accelerates the transit of food through the stomach and small bowel.
This shortened transit time through the small bowel also happens when humans drink a lot of alcohol, and is linked to diarrhoea.
Alcohol can also reduce the absorption of carbohydrates, proteins and fats in the duodenum (the first part of the small bowel).
Alcohol can lead to reduced absorption of xylose (a type of sugar). This means diarrhoea is more likely to occur in drinkers who also consume a lot of sugary foods such as sweets and sweetened juices.
Chronic alcohol use is also linked to:
- lactose intolerance
- overgrowth of small bowel bacteria and
- reduced absorption of fats from the pancreas not producing enough digestive enzymes.
This means chronic alcohol use may lead to diarrhoea and loose stools.
How might a night of heavy drinking affect your poos?
When rats are exposed to high doses of alcohol over a short period of time, it results in small bowel transit delay.
This suggests acute alcohol intake (such as an episode of binge drinking) is more likely to lead to constipation than diarrhoea.
This is backed up by recent research studying the effects of alcohol in 507 university students.
These students had their stools collected and analysed, and were asked to fill out a stool form questionnaire known as the Bristol Stool Chart.
The research found a heavy drinking episode was associated with harder, firm bowel motions.
In particular, those who consumed more alcohol had more Type 1 stools, which are separate hard lumps that look or feel a bit like nuts.
The researchers believed this acute alcohol intake results in small bowel transit delay; the food stayed for longer in the intestines, meaning more water was absorbed from the stool back into the body. This led to drier, harder stools.
Interestingly, the researchers also found there was more of a type of bacteria known as “Actinobacteria” in heavy drinkers than in non-drinkers.
This suggests bacteria may have a role to play in stool consistency.
But binge drinking doesn’t always lead to constipation. Binge drinking in patients with irritable bowel syndrom (IBS), for example, clearly leads to diarrhoea, nausea and abdominal pain.
What can I do about all this?
If you’re suffering from unwanted bowel motion changes after drinking, the most effective way to address this is to limit your alcohol intake.
Some alcoholic beverages may affect your bowel motions more than others. If you notice a pattern of troubling poos after drinking certain drinks, it may be sensible to cut back on those beverages.
If you tend to get diarrhoea after drinking, avoid mixing alcohol with caffeinated drinks. Caffeine is known to stimulate contractions of the colon and so could worsen diarrhoea.
If constipation after drinking is the problem, then staying hydrated is important. Drinking plenty of water before drinking alcohol (and having water in between drinks and after the party is over) can help reduce dehydration and constipation.
You should also eat before drinking alcohol, particularly protein and fibre-rich foods.
Food in the stomach can slow the absorption of alcohol and may help protect against the negative effects of alcohol on the gut lining.
Is it anything to worry about?
Changes in bowel motions after drinking are usually short term and, for the most part, resolve themselves pretty efficiently.
But if symptoms such as diarrhoea persist beyond a couple of days after stopping alcohol, it may signify other concerning issues such as an underlying gut disorder like inflammatory bowel disease.
Researchers have also linked alcohol consumption to the development of irritable bowel syndrome.
If problems persist or if there are alarming symptoms such as blood in your stool, seek medical advice from a general practitioner.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Stop Sabotaging Your Gut
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
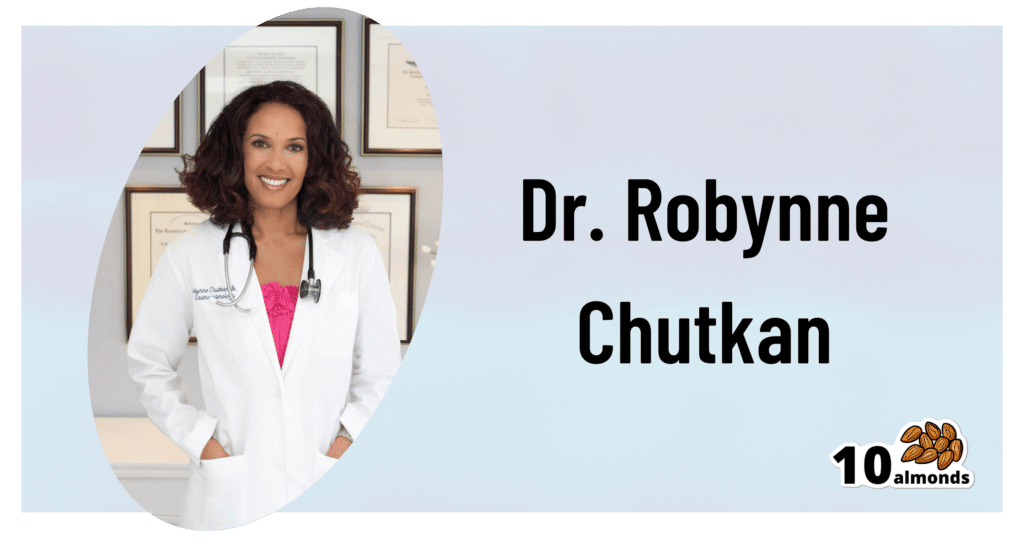
This is Dr. Robynne Chutkan. She’s an integrative gastroenterologist, and founder of the Digestive Center for Wellness, in Washington DC, which for the past 20 years has been dedicated to uncovering the root causes of gastrointestinal disorders, while the therapeutic side of things has been focused on microbial optimization, nutritional therapy, mind-body techniques, and lifestyle changes.
In other words, maximal health for minimal medicalization.
So… What does she want us to know?
Live dirty
While attentive handwashing is important to avoid the spread of communicable diseases*, excessive cleanliness in general can result in an immune system that has no idea how to deal with pathogens when exposure does finally occur.
*See also: The Truth About Handwashing
This goes doubly for babies: especially those who were born by c-section and thus missed out on getting colonized by vaginal bacteria, and especially those who are not breast-fed, and thus miss out on nutrients given in breast milk that are made solely for the benefit of certain symbiotic bacteria (humans can’t even digest those particular nutrients, we literally evolved to produce some nutrients solely for the bacteria).
See also: Breast Milk’s Benefits That Are (So Far) Not Replicable
However, it still goes for the rest of us who are not babies, too. We could, Dr. Chutkan tells us, stand to wash less in general, and definitely ease up on antibacterial soaps and so forth.
See also: Should You Shower Daily?
Take antibiotics only if absolutely necessary (and avoid taking them by proxy)
Dr. Chutkan describes antibiotics as the single biggest threat to our microbiome, not just because of overprescription, but also the antibiotics that are used in animal agriculture and thus enter the food chain (and thus, enter us, if we eat animal products).
Still, while the antibiotics meat/dairy-enjoyers will get from food are better avoided, antibiotics actually taken directly are even worse, and are absolutely a “scorched earth” tactic against whatever they’re being prescribed for.
See also: Antibiotics? Think Thrice ← which also brings up “Four Ways Antibiotics Can Kill You”; seriously, the risks of antibiotics are not to be underestimated, including the risks associated only with them working exactly as intended—let alone if something goes wrong.
Probiotics won’t save you
While like any gastroenterologist (or really, almost any person in general), she notes that probiotics can give a boost to health. However, she wants us to know about two shortcomings that are little-discussed:
1) Your body has a collection of microbiomes each with their own needs, and while it is possible to take “generally good” bacteria in probiotics and assume they’ll do good, taking Lactobacillus sp. will do nothing for a shortage of Bifidobacteria sp, and even taking the correct genus can have similar shortcomings if a different species of that genus is needed, e.g. taking L. acidophilus will do nothing for a shortage of L. reuteri.
It’d be like a person with a vitamin D deficiency taking vitamin B12 supplements and wondering why they’re not getting better.
2) Probiotics are often wasted if not taken mindfully of their recipient environment. For example, most gut bacteria only live for about 20 minutes in the gut. They’re usually inactive in the supplement form, they’re activated in the presence of heat and moisture and appropriate pH etc, and then the clock is ticking for them to thrive or die.
This means that if you take a supplement offering two billion strains of good gut bacteria, and you take it on an empty stomach, then congratulations, 20 minutes later, they’re mostly dead, because they had nothing to eat. Or if you take it after drinking a soda, congratulations, they’re mostly dead because not only were they starved, but also their competing “bad” microbes weren’t starved and changed the environment to make it worse for the “good” ones.
For this reason, taking probiotics with (or immediately after) plenty of fiber is best.
This is all accentuated if you’re recovering from using antibiotics, by the way.
Imagine: a nuclear war devastates the population of the Earth. Some astronauts manage to safely return, finding a mostly-dead world covered in nuclear winter. Is the addition of a few astronauts going to quickly repopulate the world? No, of course not. They are few, the death toll is many, and the environment is very hostile to life. A hundred years later, the population will be pretty much the same—a few straggling survivors.
It’s the same after taking antibiotics, just, generations pass in minutes instead of decades. You can’t wipe out almost everything beneficial in the gut, create a hostile environment there, throw in a couple of probiotic gummies, and expect the population to bounce back.
That said, although “probiotics will not save you”, they can help provided you give them a nice soft bed of fiber to land on, some is better than none, and guessing at what strains are needed is better than giving nothing.
See also: How Much Difference Do Probiotic Supplements Make, Really?
What she recommends
So to recap, we’ve had:
- Wash less, and/or with less harsh chemicals
- Avoid antibiotics like the plague, unless you literally have The Plague, for which the treatment is indeed antibiotics
- Avoid antibiotic-contaminated foods, which in the US is pretty much all animal products unless it’s, for example, your own back-yard hens whom you did not give antibiotics. Do not fall for greenwashing aesthetics in the packaging of “happy cows” and their beef, milk, etc, “happy hens” and their meat, eggs, etc… If it doesn’t explicitly claim to be free from the use of antibiotics, then antibiotics were almost certainly used.
- Dr. Chutkan herself is not even vegan, by the way, but very much wants us to be able to make informed choices about this, and does recommend at least a “plants-forward” diet, for the avoiding-antibiotics reason and for the plenty-of-fiber reason, amongst others.
- Consider probiotics, but don’t expect them to work miracles by themselves; you’ve got to help them to help you.
- Dr. Chutkan also recommends getting microbiome tests done if you think something might be amiss, and then you can supplement with probiotics in a more targetted fashion instead of guessing at what species is needed where.
She also recommends, of course, a good gut-healthy diet in general, especially “leafy green things that were recently alive; not powders”, beans, and nuts, while avoiding gut-unhealthy things such as sugars-without-fiber, alcohol, or some gut-harmful additives (such as most artificial sweeteners, although stevia is a gut-healthy exception, and sucralose is ok in moderation).
For more on gut-healthy eating, check out:
Make Friends With Your Gut (You Can Thank Us Later)
Want to know more from Dr. Chutkan?
We recently reviewed an excellent book of hers:
The Anti-Viral Gut: Tackling Pathogens From The Inside Out – by Dr. Robynne Chutkan
Enjoy!
Share This Post
Related Posts
-
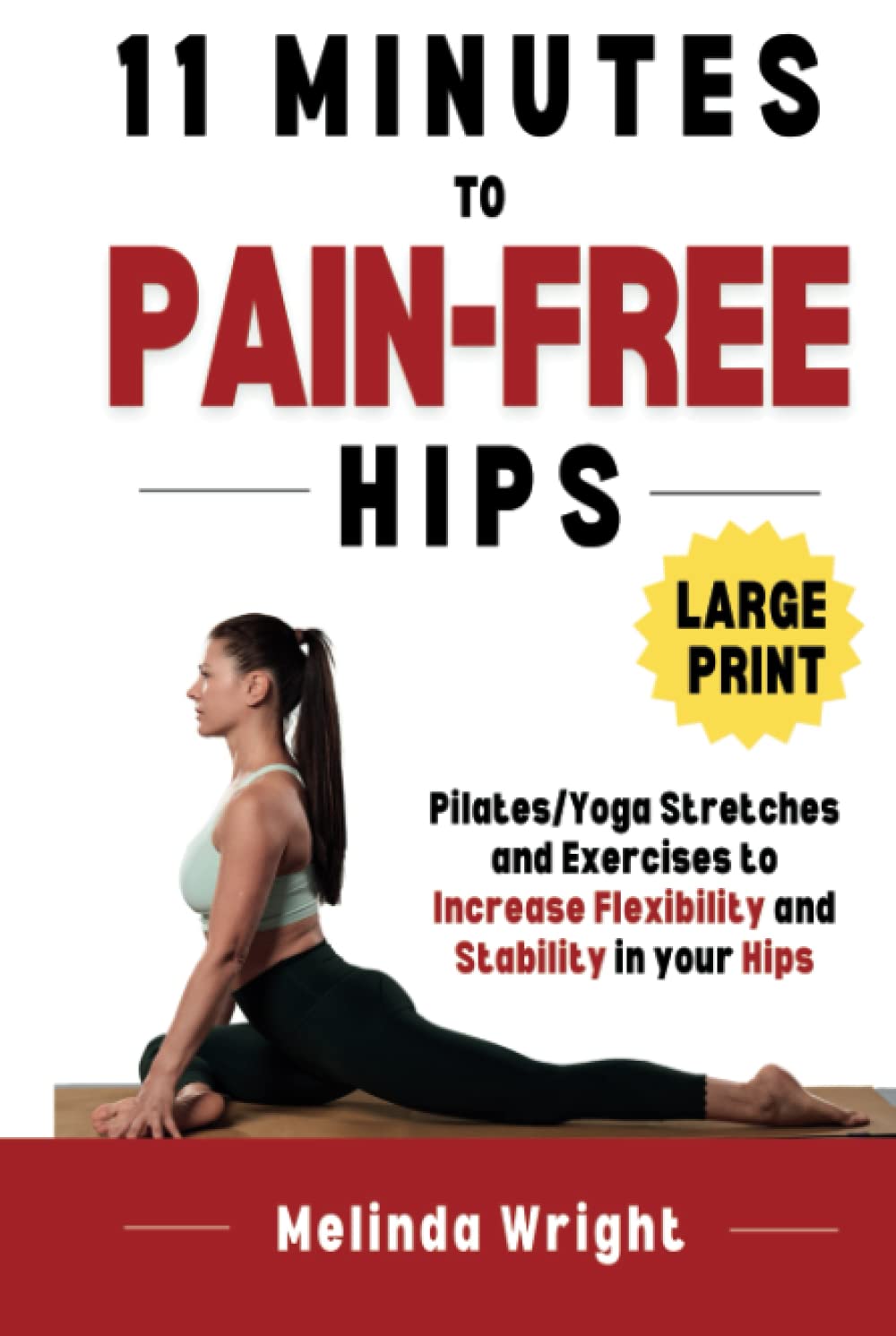
11 Minutes to Pain-Free Hips – by Melinda Wright
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If hips don’t lie, what are yours saying to you? If what they’re saying to you sounds like a cry for help sometimes, this is the book to get you onto a better track.
The hip is the largest joint in your body, and it bears a lot of weight. So it’s little wonder if sometimes they’d like a word with the boss. The question is: what will you do about it? Melinda Wright has suggestions to keep your hips—and you—happy.
She spends the first couple of chapters introducing key concepts, and some anatomy and physiology that’ll be good to know.
Then we’re into resistance stretching, basic hip exercises, all the way through to more advanced stuff. There are very clear photos for each. One thing that stands out about this book is each exercise is not just explained simply and clearly, but also offers “easing oneself in” exercises. After all, we’re not all at the same starting point.
The book finishes off with some more holistic advice about chronic pain management, based on her personal experience with scoliosis, and some dietary tips to reduce joint pain and inflammation too.
All in all, a very helpful book!
Pick up 11 “Minutes to Pain-Free Hips” at Amazon today!
^You will also see options for pain-free back, and pain-free neck, by the same author
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Huperzine A: A Natural Nootropic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Huperzine A: A Natural Nootropic
Huperzine A is a compound, specifically a naturally occurring sesquiterpene alkaloid, that functions as an acetylcholinesterase inhibitor. If that seems like a bunch of big words, don’t worry, we’ll translate in a moment.
First, a nod to its origins: it is found in certain kinds of firmoss, especially the “toothed clubmoss”, Huperzia serrata, which grows in many Asian countries.
What’s an acetylcholinesterase inhibitor?
Let’s do this step-by-step:
- An acetylcholinesterase inhibitor is a compound that inhibits acetylcholinesterase.
- Acetylcholinesterase is an enzyme that catalyzes (speeds up) the breakdown of acetylcholine.
- Acetylcholine is a neurotransmitter; it’s an ester of acetic acid and choline.
- This is the main neurotransmitter of the parasympathetic nervous system, and is also heavily involved in cognitive functions including memory and creative thinking.
What this means: if you take an acetylcholinesterase inhibitor like huperzine A, it will inhibit acetylcholinesterase, meaning you will have more acetylcholine to work with. That’s good.
What can I expect from it?
Huperzine A has been well-studied for a while, mostly for the prevention and treatment of Alzheimer’s disease:
- New insights into huperzine A for the treatment of Alzheimer’s disease
- Huperzine A: Is it an Effective Disease-Modifying Drug for Alzheimer’s Disease?
- Huperzine A and Its Neuroprotective Molecular Signaling in Alzheimer’s Disease
However, research has suggested that huperzine A is much better as a prevention than a treatment:
❝A central event in the pathogenesis of Alzheimer’s disease (AD) is the accumulation of senile plaques composed of aggregated amyloid-β (Aβ) peptides.
Ex vivo electrophysiological experiments showed that 10 μM of Aβ1-40 significantly decreased the effect of the AChE inhibitor huperzine A on the synaptic potential parameters. ❞
~ Dr. Irina Zueva
In other words: the answer to the titular question is “Yes, yes it can”
And, to translate Dr. Zueva’s words into simple English:
- People with Alzheimer’s have amyloid-β plaque in their brains
- That plaque reduces the effectiveness of huperzine A
So, what if we take it in advance? That works much better:
❝Pre-treatment with [huperzine A] at concentrations of 50, 100, and 150 µg/mL completely inhibited the secretion of PGE2, TNF-α, IL-6, and IL-1β compared to post-treatment with [huperzine A].
This suggests that prophylactic treatment is better than post-inflammation treatment. ❞
~ Dr. Thu Kim Dang
Source: Anti-neuroinflammatory effects of alkaloid-enriched extract from Huperzia serrata
As you may know, neuroinflammation is a big part of Alzheimer’s pathology, so we want to keep that down. The above research suggests we should do that sooner rather than later.
Aside from holding off dementia, can it improve memory now, too?
There’s been a lot less research done into this (medicine is generally more concerned with preventing/treating disease, than improving the health of healthy people), but there is some:
^This is a small (n=68) old (1999) study for which the full paper has mysteriously disappeared and we only get to see the abstract. It gave favorable results, though.
The effects of huperzine A and IDRA 21 on visual recognition memory in young macaques
^This, like most non-dementia research into HupA, is an animal study. But we chose to spotlight this one because, unlike most of the studies, it did not chemically lobotomize the animals first; they were and remained healthy. That said, huperzine A improved the memory scores most for the monkeys that performed worst without it initially.
Where can I get it?
As ever, we don’t sell it, but here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I have a stuffy nose, how can I tell if it’s hay fever, COVID or something else?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hay fever (also called allergic rhinitis) affects 24% of Australians. Symptoms include sneezing, a runny nose (which may feel blocked or stuffy) and itchy eyes. People can also experience an itchy nose, throat or ears.
But COVID is still spreading, and other viruses can cause cold-like symptoms. So how do you know which one you’ve got?
Lysenko Andrii/Shutterstock Remind me, how does hay fever cause symptoms?
Hay fever happens when a person has become “sensitised” to an allergen trigger. This means a person’s body is always primed to react to this trigger.
Triggers can include allergens in the air (such as pollen from trees, grasses and flowers), mould spores, animals or house dust mites which mostly live in people’s mattresses and bedding, and feed on shed skin.
When the body is exposed to the trigger, it produces IgE (immunoglobulin E) antibodies. These cause the release of many of the body’s own chemicals, including histamine, which result in hay fever symptoms.
People who have asthma may find their asthma symptoms (cough, wheeze, tight chest or trouble breathing) worsen when exposed to airborne allergens. Spring and sometimes into summer can be the worst time for people with grass, tree or flower allergies.
However, animal and house dust mite symptoms usually happen year-round.
Ryegrass pollen is a common culprit. bangku ceria/Shutterstock What else might be causing my symptoms?
Hay fever does not cause a fever, sore throat, muscle aches and pains, weakness, loss of taste or smell, nor does it cause you to cough up mucus.
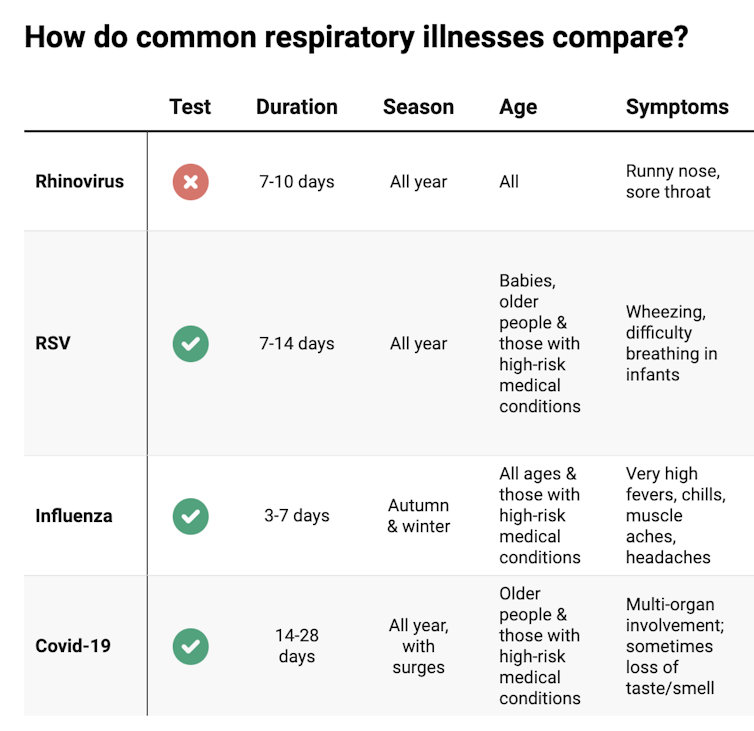
These symptoms are likely to be caused by a virus, such as COVID, influenza, respiratory syncytial virus (RSV) or a “cold” (often caused by rhinoviruses). These conditions can occur all year round, with some overlap of symptoms:
Natasha Yates/The Conversation COVID still surrounds us. RSV and influenza rates appear higher than before the COVID pandemic, but it may be due to more testing.
So if you have a fever, sore throat, muscle aches/pains, weakness, fatigue, or are coughing up mucus, stay home and avoid mixing with others to limit transmission.
People with COVID symptoms can take a rapid antigen test (RAT), ideally when symptoms start, then isolate until symptoms disappear. One negative RAT alone can’t rule out COVID if symptoms are still present, so test again 24–48 hours after your initial test if symptoms persist.
You can now test yourself for COVID, RSV and influenza in a combined RAT. But again, a negative test doesn’t rule out the virus. If your symptoms continue, test again 24–48 hours after the previous test.
If it’s hay fever, how do I treat it?
Treatment involves blocking the body’s histamine release, by taking antihistamine medication which helps reduce the symptoms.
Doctors, nurse practitioners and pharmacists can develop a hay fever care plan. This may include using a nasal spray containing a topical corticosteroid to help reduce the swelling inside the nose, which causes stuffiness or blockage.
Nasal sprays need to delivered using correct technique and used over several weeks to work properly. Often these sprays can also help lessen the itchy eyes of hay fever.
Drying bed linen and pyjamas inside during spring can lessen symptoms, as can putting a smear of Vaseline in the nostrils when going outside. Pollen sticks to the Vaseline, and gently blowing your nose later removes it.
People with asthma should also have an asthma plan, created by their doctor or nurse practitioner, explaining how to adjust their asthma reliever and preventer medications in hay fever seasons or on allergen exposure.
People with asthma also need to be alert for thunderstorms, where pollens can burst into tinier particles, be inhaled deeper in the lungs and cause a severe asthma attack, and even death.
What if it’s COVID, RSV or the flu?
Australians aged 70 and over and others with underlying health conditions who test positive for COVID are eligible for antivirals to reduce their chance of severe illness.
Most other people with COVID, RSV and influenza will recover at home with rest, fluids and paracetamol to relieve symptoms. However some groups are at greater risk of serious illness and may require additional treatment or hospitalisation.
For RSV, this includes premature infants, babies 12 months and younger, children under two who have other medical conditions, adults over 75, people with heart and lung conditions, or health conditions that lessens the immune system response.
For influenza, people at higher risk of severe illness are pregnant women, Aboriginal people, people under five or over 65 years, or people with long-term medical conditions, such as kidney, heart, lung or liver disease, diabetes and decreased immunity.
If you’re concerned about severe symptoms of COVID, RSV or influenza, consult your doctor or call 000 in an emergency.
If your symptoms are mild but persist, and you’re not sure what’s causing them, book an appointment with your doctor or nurse practitioner. Although hay fever season is here, we need to avoid spreading other serious infectious.
For more information, you can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria); use the online Symptom Checker; or visit healthdirect.gov.au or the Australian Society of Clinical Immunology and Allergy.
Deryn Thompson, Eczema and Allergy Nurse; Lecturer, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: