Avocado vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to blueberries, we picked the avocado.
Why?
These two fruits aren’t as similar as some of the comparisons we’ve made—we often go for “can be used in the same way culinarily” comparisons. But! They are both popularly in the “superfood” category, so it’s interesting to consider:
In terms of macros, avocado has more protein, (healthy!) fat, and fiber, while blueberries have more carbs. An easy win for avocado here, unless you’re on a calorie-controlled diet perhaps, since avocado is also higher in those. About that fat; it’s mostly monounsaturated, with some polyunsaturated and saturated, and is famously a good source of omega-3 in the form of ALA.
In the category of vitamins, avocado has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while blueberries are not higher in any vitamins. So, not a tricky decision here.
When it comes to minerals, avocado has more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while blueberries are higher in manganese. Another win for avocados.
There is one other category that’s important to consider in this case, and that’s polyphenols. We’d be here all day if we listed them all, but in total, blueberries have about 1193x the polyphenol content that avocados do. Blueberries got the reputation for antioxidant properties for a reason; it is well-deserved!
So, out of the two, we declare avocado the overall more nutritious of the two, but blueberries absolutely deserve the acclaim they get also.
Want to learn more?
You might like to read:
Give Us This Day Our Daily Dozen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
ADHD For Smart Ass Women – by Tracy Otsuka
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about ADHD in adults before, what makes this one different? It’s the wholly female focus. Which is not to say some things won’t apply to men too, they will.
But while most books assume a male default unless it’s “bikini zone” health issues, this one is written by a woman for women focusing on the (biological and social) differences in ADHD for us.
A strength of the book is that it neither seeks to:
- over-medicalize things in a way that any deviation from the norm is inherently bad and must be fixed, nor
- pretend that everything’s a bonus, that we are superpowered and beautiful and perfect and capable and have no faults that might ever need addressing actually
…instead, it gives a good explanation of the ins and outs of ADHD in women, the strengths and weaknesses that this brings, and good solid advice on how to play to the strengths and reduce (or at least work around) the weaknesses.
Bottom line: this book has been described as “ADHD 2.0 (a very popular book that we’ve reviewed previously), but for women”, and it deserves that.
Click here to check out ADHD for Smart Ass Women, and fall in love with your neurodivergent brain!
Share This Post
-
Life Lessons From A Brain Surgeon – by Dr. Rahul Jandial
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the category of surgeons with a “what to put on your table to stay off mine” angle, this book packs an extra punch. As well as being an experienced brain surgeon, Dr. Jandial also does a lot of cutting edge lab research too. What does this mean for us?
This book gives, as the subtitle promises, “practical strategies for peak health and performance”—with a brain-centric bias, of course.
From diet and nootropic supplements, to exercise and brain-training, we get a good science-based view of which ones actually work, and which don’t. The style is also very readable; Dr. Jandial is a great educator, presenting genuine scientific content with very accessible language.
Bottom line: if you’d indeed like to look after your most important organ optimally, this book gives a lot of key pointers, without unnecessary fluff.
Share This Post
-
Body Image Dissatisfaction/Appreciation Across The Ages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Every second news article about body image issues is talking about teens and social media use, but science tells a different story.
A large (n=1,327) study of people of mixed genders aged 16–88 examined matters relating to people’s body image, expecting…
❝We hypothesized that body dissatisfaction and importance of appearance would be higher in women than in men, that body dissatisfaction would remain stable across age in women, and that importance of appearance would be lower in older women compared to younger women. Body appreciation was predicted to be higher in men than in women.❞
As they discovered, only half of that turned out to be true:
❝In line with our hypotheses, body dissatisfaction was higher in women than in men and was unaffected by age in women, and importance of appearance was higher in women than in men.
However, only in men did age predict a lower level of the importance of appearance. Compared to men, women stated that they would invest more hours of their lives to achieve their ideal appearance.
Contrary to our assumption, body appreciation improved and was higher in women across all ages than in men.❞
You can read the study in full here:
That’s a lot of information, and we don’t have the space to go into all parts of it here, fascinating as that would be. So we’re going to put two pieces of information (from the above) next to each other:
- body dissatisfaction was higher in women than in men and was unaffected by age in women
- body appreciation improved and was higher in women across all ages than in men
…and resolve this apparent paradox.
Dissatisfied appreciation
How is it that women are both more dissatisfied with, and yet also more appreciative of, their bodies?
The answer is that we can have positive and negative feelings about the same thing, without them cancelling each other out. In short, simply, feeling more feelings about it.
Whether the gender-related disparity in this case comes more from hormones or society could be vigorously debated, but chances are, it’s both. And, for our gentleman-readers, note that the principle still applies to you, even if scaled down on average.
Call to action:
- be aware of the negative feelings of body dissatisfaction
- focus on the positive feelings of body appreciation
While in theory both could motivate us to action, in reality, the former will tend to inform us (about what we might wish to change), while the latter will actually motivate us in a useful way (to do something positive about it).
This is because the negative feelings about body image tend to be largely based in shame, and shame is a useless motivator (i.e., it simply doesn’t work) when it comes to taking positive actions:
Why Shame Only Works Negatively
You can’t hate yourself into a body you love
That may sound like a wishy-washy platitude, but given the evidence on how shame works (and doesn’t), it’s true.
Instead, once you’ve identified the things about your body with which you’re dissatisfied, you can then assess:
- what can reasonably be changed
- whether it is important enough to you to change it
- how to go about usefully changing it
While weight issues are perhaps the most commonly-discussed body image consideration, to the point that often all others get forgotten, let’s look at something that’s generally more specific to adults, and also a very common cause of distress for women and men alike: hair loss/thinning.
If your hair is just starting to thin and fall, then if this bothers you, there’s a lot that can be done about it quite easily, but (and this is important) you have to love yourself enough to actually do it. Merely feeling miserable about it, and perhaps like you don’t deserve better, or that it is somehow a personal failing on your part, will not help.
If your hair has been gone for years, then chances are you’ve made your peace with this by now, and might not even take it back if a fairy godmother came along and offered to restore it magically. On the other hand, let’s say that you’re just coming out the other end of a 10-year-long depression, and perhaps you let a lot of things go that you now wish you hadn’t, and maybe your hair is one of them. In this case, now you need to decide whether getting implants (likely the only solution at this late stage) is worth it.
Note that in both cases, whatever the starting point and whether the path ahead is easy or hard, the person who has dissatisfaction and/but still values themself and their body will get what they need.
In contrast, the person who has dissatisfaction and does not value themself and their body, will languish.
The person without dissatisfaction, of course, probably already has what they need.
In short: identification of dissatisfaction + love and appreciation of oneself and one’s body → motivation to usefully take action (out of love, not hate)
Now, dear reader, apply the same thinking to whatever body image issues you may have, and take it from there!
Embodiment
A quick note in closing: if you are a person with no body dissatisfactions, there are two main possible reasons:
- You are genuinely happy with your body in all respects. Congratulations!
- You have disassociated from your body to such an extent that it’s become a mere vehicle to you and you don’t care about it.
This latter may seem like a Zen-level win, but in fact it’s a warning sign for depression, so please do examine that even if you don’t “feel” depressed (depression is often characterized by a lack of feelings), perhaps by taking the (very quick) free PHQ9 Test ← under 2 minutes; immediate results; industry-standard diagnostic tool
Take care!
Share This Post
Related Posts
-
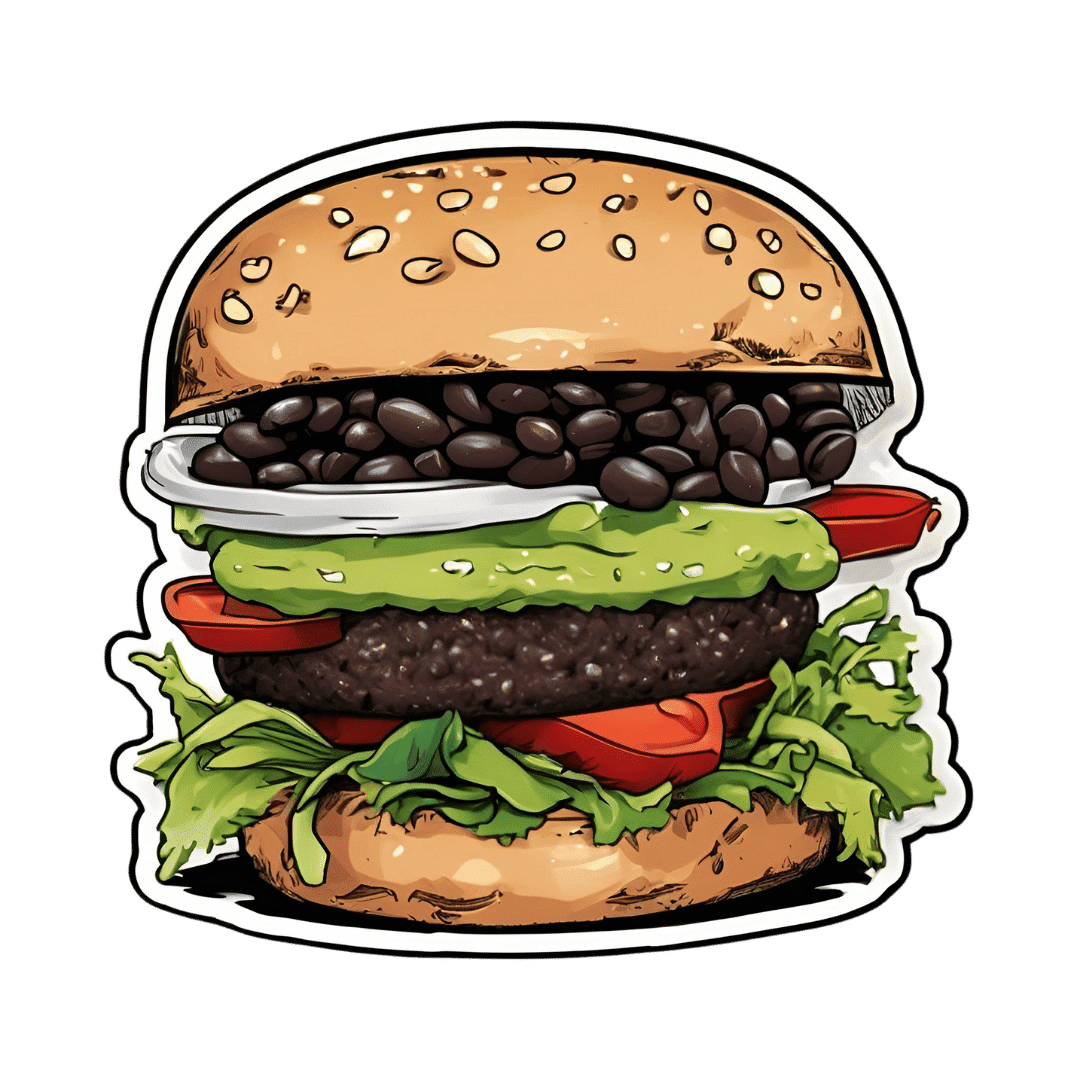
Black Bean Burgers With Guacamole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Once again proving that burgers do not have to be unhealthy, this one’s a nutritional powerhouse full of protein, fiber, vitamins, and minerals, as well as healthy fats and extra health-giving spices.
You will need
- 1 can black beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- 3 oz walnuts (if allergic, substitute with pumpkin seeds)
- 1 tbsp chia seeds
- 1 tbsp flax seeds
- ½ red onion, finely chopped
- 1 small eggplant, diced small (e.g. ½” cubes or smaller)
- 1 small carrot, grated
- 3 tbsp finely chopped cilantro (or if you have the “this tastes like soap” gene, then substitute with parsley)
- 1 tbsp lemon juice
- 1 jalapeño pepper, finely chopped (adjust per heat preferences)
- ¼ bulb garlic, crushed
- 2 tsp black pepper
- 1 tsp smoked paprika
- 1 tsp cayenne pepper (adjust per heat preferences)
- ½ tsp MSG or 1 tsp low-sodium salt
- Burger buns (you can use our Delicious Quinoa Avocado Bread recipe if you like)
For the guacamole:
- 1 large ripe avocado, pitted, skinned, and chopped
- 1 tbsp lime juice
- 1 tomato, finely chopped
- ¼ red onion, finely chopped
- ¼ bulb garlic, crushed
- 1 tsp red chili pepper flakes (adjust per heat preferences)
Method
(we suggest you read everything at least once before doing anything)
1) Process the walnuts, chia seeds, and flax seeds in a food processor/blender, until they become a coarse mixture. Set aside.
2) Heat a little oil in a skillet, and fry the red onion, aubergine, and carrot for 5 minutes stirring frequently, then add the garlic and jalapeño and stir for a further 1 minute. Set aside.
3) Combine both mixtures you set aside with the rest of the ingredients from the burger section of the recipe, except the buns, and process them in the food processor on a low setting if possible, until you have a coarse mixture—you still want some texture, not a paste.
4) Shape into patties; this recipe gives for 4 large patties or 8 small ones. When you’ve done this, put them in the fridge for at least 30 minutes, to firm up.
5) While you wait, make the guacamole by mashing the avocado with the lime juice, and then stirring into the onion, tomato, garlic, and pepper.
6) Cook the patties; you can do this on the grill, in a skillet, or in the oven, per your preference. Grilling or frying should take about 5 minutes on each side, give or take the size and shape of the patties. Baking in the oven should take 20–30 minutes at 400℉ / 200℃ turning over halfway through, but keep an eye on them, because again, the size and shape of the patties will affect this. You may be wondering: aren’t they all going to be patty-shaped? And yes, but for example a wide flat patty will cook more quickly than the same volume of burger mixture in a taller less wide patty.
7) Assemble! We recommend the order: bottom bun, guacamole, burger patty, any additional toppings you want to add (e.g. more salad, pickles, etc), top bun:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Chickpeas vs Black Beans – Which is Healthier?
- Kidney Beans or Black Beans – Which is Healthier?
- Coconut vs Avocado – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From Strength to Strength – by Dr. Arthur Brooks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For most professions, there are ways in which performance can be measured, and the average professional peak varies by profession, but averages are usually somewhere in the 30–45 range, with a pressure to peak between 25–35.
With a peak by age 45 or perhaps 50 at the latest (aside from some statistical outliers, of course), what then to expect at age 50+? Not long after that, there’s a reason for mandatory retirement ages in some professions.
Dr. Brooks examines the case for accepting that rather than fighting it, and/but making our weaknesses into our strengths as we go. If our fluid intelligence slows, our accumulated crystal intelligence (some might call it “wisdom“) can make up for it, for example.
But he also champions the idea of looking outside of ourselves; of the importance of growing and fostering connections; giving to those around us and receiving support in turn; not transactionally, but just as a matter of mutualism of the kind found in many other species besides our own. Indeed, Dr. Brooks gives the example of a grove of aspen trees (hence the cover art of this book) that do exactly that.
The style is very accessible in terms of language but with frequent scientific references, so very much a “best of both worlds” in terms of readability and information-density.
Bottom line: if ever you’ve wondered at what age you might outlive your usefulness, this book will do as the subtitle suggests, and help you carve out your new place.
Click here to check out From Strength To Strength, and find yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: