ADHD medication – can you take it long term? What are the risks and do benefits continue?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Attention deficit hyperactivity disorder (ADHD) is a condition that can affect all stages of life. Medication is not the only treatment, but it is often the treatment that can make the most obvious difference to a person who has difficulties focusing attention, sitting still or not acting on impulse.
But what happens once you’ve found the medication that works for you or your child? Do you just keep taking it forever? Here’s what to consider.
What are ADHD medications?
The mainstay of medication for ADHD is stimulants. These include methylphenidate (with brand names Ritalin, Concerta) and dexamfetamine. There is also lisdexamfetamine (branded Vyvanse), a “prodrug” of dexamfetamine (it has a protein molecule attached, which is removed in the body to release dexamfetamine).
There are also non-stimulants, in particular atomoxetine and guanfacine, which are used less often but can also be highly effective. Non-stimulants can be prescribed by GPs but this may not always be covered by the Pharmaceutical Benefits Scheme and could cost more.
How stimulants work
Some stimulants prescribed for ADHD are “short acting”. This means the effect comes on after around 20 minutes and lasts around four hours.
Longer-acting stimulants give a longer-lasting effect, usually by releasing medication more slowly. The choice between the two will be guided by whether the person wants to take medication once a day or prefers to target the medication effect to specific times or tasks.
For the stimulants (with the possible exception of lisdexamfetamine) there is very little carry-over effect to the next day. This means the symptoms of ADHD may be very obvious until the first dose of the morning takes effect.
One of the main aims of treatment is the person with ADHD should live their best life and achieve their goals. In young children it is the parents who have to consider the risks and benefits on behalf of the child. As children mature, their role in decision making increases.
What about side effects?
The most consistent side effects of the stimulants are they suppress appetite, resulting in weight loss. In children this is associated with temporary slowing of the growth rate and perhaps a slight delay in pubertal development. They can also increase the heart rate and may cause a rise in blood pressure. Stimulants often cause insomnia.
These changes are largely reversible on stopping medication. However, there is concern the small rises in blood pressure could accelerate the rate of heart disease, so people who take medication over a number of years might have heart attacks or strokes slightly sooner than would have happened otherwise.
This does not mean older adults should not have their ADHD treated. Rather, they should be aware of the potential risks so they can make an informed decision. They should also make sure high blood pressure and attacks of chest pain are taken seriously.
Stimulants can be associated with stomach ache or headache. These effects may lessen over time or with a reduction in dose. While there have been reports about stimulants being misused by students, research on the risks of long-term prescription stimulant dependence is lacking.
Will medication be needed long term?
Although ADHD can affect a person’s functioning at all stages of their life, most people stop medication within the first two years.
People may stop taking it because they don’t like the way it makes them feel, or don’t like taking medication at all. Their short period on medication may have helped them develop a better understanding of themselves and how best to manage their ADHD.
In teenagers the medication may lose its effectiveness as they outgrow their dose and so they stop taking it. But this should be differentiated from tolerance, when the dose becomes less effective and there are only temporary improvements with dose increases.
Tolerance may be managed by taking short breaks from medication, switching from one stimulant to another or using a non-stimulant.

Ground Picture/Shutterstock
Too many prescriptions?
ADHD is becoming increasingly recognised, with more people – 2–5% of adults and 5–10% of children – being diagnosed. In Australia stimulants are highly regulated and mainly prescribed by specialists (paediatricians or psychiatrists), though this differs from state to state. As case loads grow for this lifelong diagnosis, there just aren’t enough specialists to fit everyone in.
In November, a Senate inquiry report into ADHD assessment and support services highlighted the desperation experienced by people seeking treatment.
There have already been changes to the legislation in New South Wales that may lead to more GPs being able to treat ADHD. Further training could help GPs feel more confident to manage ADHD. This could be in a shared-care arrangement or independent management of ADHD by GPs like a model being piloted at Nepean Blue Mountains Local Health District, with GPs training within an ADHD clinic (where I am a specialist clinician).
Not every person with ADHD will need or want to take medication. However, it should be more easily available for those who could find it helpful.
Alison Poulton, Senior Lecturer, Brain Mind Centre Nepean, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hungry? How To Beat Cravings
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Science of Hunger, And How To Sate It
This is Dr. David Ludwig. That’s not a typo; he’s a doctor both ways—MD and PhD.
Henceforth we’ll just say “Dr. Ludwig”, though! He’s a professor in the Department of Nutrition at Harvard T.H. Chan School of Public Health, and director of the New Balance Foundation Obesity Prevention Center.
His research focuses on the effects of diet on hormones, metabolism, and body weight, and he’s one of the foremost experts when it comes to carbohydrates, glycemic load, and obesity.
Why are we putting on weight? What are we getting wrong?
Contrary to popular belief, Dr. Ludwig says, weight gain is not caused by a lack of exercise. In fact, people tend to overestimate how many calories are burned by exercise.
A spoonful of sugar may make the medicine go down, but it also contains 60 calories, and that’d take about 1,500 steps for the average person to burn off. Let’s put this another way:
If you walk 10,000 steps per day, that will burn off 400 calories. Still think you can exercise away that ice cream sundae or plate of fries?
Wait, this is interesting and all, but what does this have to do with hunger?
Why we get hungry
Two important things:
- All that exercise makes us hungry, because the more we exercise, the more the body speeds up our metabolism accordingly.
- Empty calories don’t just add weight themselves, they also make us hungrier
What are empty calories, and why do they make us hungrier?
Empty calories are calories that are relatively devoid of other nutrition. This especially means simple sugars (especially refined sugar), white flour and white flour products (quick-release starches), and processed seed oils (e.g. canola, sunflower, and friends).
They zip straight into our bloodstream, and our body sends out an army of insulin to deal with the blood sugar spike. And… that backfires.
Imagine a person whose house is a terrible mess, and they have a date coming over in half an hour.
They’re going to zoom around tidying, but they’re going to stuff things out of sight as quickly and easily as possible, rather than, say, sit down and Marie Kondo the place.
But superficially, they got the job done really quickly!
Insulin does similarly when overwhelmed by a blood sugar spike like that.
So, it stores everything as fat as quickly as possible, and whew, the pancreas needs a break now after all that exertion, and the blood is nice and free from blood sugars.
Wait, the blood is what now?
The body notices the low blood sugar levels, and it also knows you just stored fat so you must be preparing for starvation, and now the low blood sugar levels indicate starvation is upon us. Quick, we must find food if we want to survive! So it sends a hunger signal to make sure you don’t let the body starve.
You make a quick snack, and the cycle repeats.
Dr. Ludwig’s solution:
First, we need to break out of that cycle, and that includes calming down our insulin response (and thus rebuilding our insulin sensitivity, as our bodies will have become desensitized, after the equivalent of an air-raid siren every 40 minutes or so).
How to do that?
First, cut out the really bad things that we mentioned above.
Next: cut healthy carbs too—we’re talking unprocessed grains here, legumes as well, and also starchy vegetables (root vegetables etc). Don’t worry, this will be just for a short while.
The trick here is that we are resensitizing our bodies to insulin.
Keep this up for even just a week, and then gradually reintroduce the healthier carbs. Unprocessed grains are better than root vegetables, as are legumes.
You’re not going to reintroduce the sugars, white flour, canola oil, etc. You don’t have to be a puritan, and if you go to a restaurant you won’t undo all your work if you have a small portion of fries. But it’s not going to be a part of your general diet.
Other tips from Dr. Ludwig:
- Get plenty of high-quality protein—it’s good for you and suppresses your appetite
- Shop for success—make sure you keep your kitchen stocked with healthy easy snack food
- Nuts, cacao nibs, and healthy seeds will be your best friends and allies here
- Make things easy—buy pre-chopped vegetables, for example, so when you’re hungry, you don’t have to wait longer (and work more) to eat something healthy
- Do what you can to reduce stress, and also eat mindfully (that means paying attention to each mouthful, rather than wolfing something down while multitasking)
If you’d like to know more about Dr. Ludwig and his work, you can check out his website for coaching, recipes, meal plans, his blog, and other resources!
Share This Post
-
Doctors From 15 Specialties Tell The Worst Common Mistakes People Make
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whatever your professional background, you probably know many things about it that are very obvious to you, but that most people don’t know. So it is for doctors too; here are the things that doctors from 15 specialties would never do, and thus advise people against doing:
Better safe than sorry
We’ll leap straight into it:
- General Surgery: avoid rushing into musculoskeletal or spinal surgery unless absolutely necessary; conservative treatments like physical therapy are often effective.
- Interventional Gastroenterology: avoid long-term, around-the-clock use of anti-inflammatory pain medications (e.g. Ibuprofen and friends) to prevent stomach ulcers.
- Podiatry: never place feet on the car dashboard due to the risk of severe injuries from airbag deployment.
- Rheumatology: avoid daily use of high heels to prevent joint and foot deformities, bunions, and pain.
- Otorhinolaryngology: never smoke, as it can lead to severe consequences like laryngectomy and other life-altering conditions.
- Pediatrics: avoid dangerous activities for children, such as swimming alone, eating choking hazards, biking or skiing without a helmet, or consuming raw meat/fish/dairy. Also, be cautious with firearms in homes.
- Orthopedic Surgery: avoid riding motorcycles and handling fireworks due to high risks of accidents.
- Emergency Medicine: never drink and drive or ride ATVs. Always use eye protection during activities like woodworking.
- Ophthalmology: always wear safety glasses during activities like grinding metal or woodworking. Sunglasses are essential to prevent UV damage even on cloudy days.
- Urology: avoid shaving pubic hair if diabetic or immunocompromised to prevent severe infections like Fournier’s gangrene.
- Gastroenterology: do not use gut health supplements as they lack proven efficacy and are often a waste of money*
- Plastic Surgery: avoid contour threads (barbed sutures for facial rejuvenation) and butt implants due to risks like infection, complications, and poor outcomes.
- Psychiatry: never take recreational drugs from unknown sources to avoid accidental overdoses, especially from substances laced with fentanyl. Carry Narcan for emergencies.
- Dermatology: use sunscreen daily to prevent skin cancer, aging, pigmentation issues, and texture problems caused by UV exposure.
- Cardiology: avoid the carnivore diet as it increases heart disease risks due to its negligible fiber content and high saturated fat intake.
*We had an article about this a while back; part of the problem is that taking probiotics without prebiotics can mean your new bacteria just die in about 20 minutes, which is their approximate lifespan in which to multiply or else die out. Similar problems arise if taking them with sugar that feeds their competitors instead. See: Stop Sabotaging Your Gut!
For more on each of these, in the words of the respective doctors, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
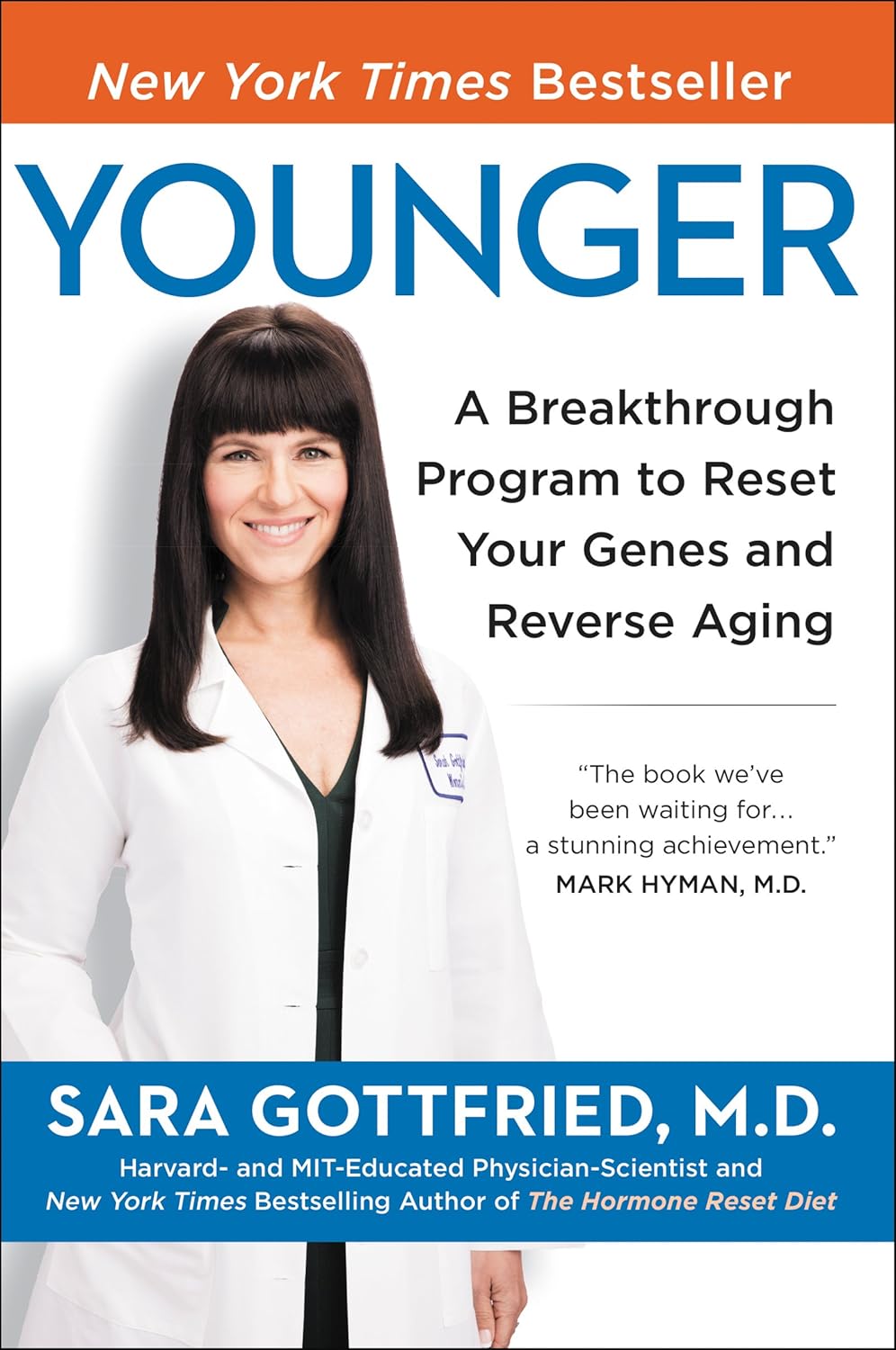
Younger – by Dr. Sara Gottfried
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does this do the things it says in the subtitle? In honestly, not really, no, but what it does do (if implemented) is modify your gene expression, slow aging, and extend healthspan. Which is all good stuff, even if it’s not the snappy SEO-oriented keywords in the subtitle.
A lot of the book pertains to turning certain genes (e.g. SIRT1, mTOR, VDR, APOE4, etc) on or off per what is sensible in each case, noting that while genes are relatively fixed (technically they can be changed, but the science is young and we can’t do much yet), gene expression is something we can control quite a bit. And while it may be unsettling to have the loaded gun that is the APOE4 gene being held against your head, at the end of the day there are things we can do that influence whether the trigger gets pulled, and when. Same goes for other undesirable genes, and also for the desirable ones that are useless if they never actually get expressed.
She offers (contained within the book, not as an upsell) a 7-week program that aims to set the reader up with good healthy habits to do just that and thus help keep age-related maladies at bay, and if we slip up, perhaps later in the year or so, we can always recommence the program.
The advice is also just good health advice, even without taking gene expression into account, because there are a stack of benefits to each of the things in her protocol.
The style is personable without being padded with fluff, accessible without dumbing down, and information-dense without being a challenging read. The formatting helps a lot also; a clear instructional layout is a lot better than a wall of text.
Bottom line: if you’d like to tweak your genes for healthy longevity, this book can help you do just that!
Share This Post
Related Posts
-
Sauerkraut vs Pickled Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sauerkraut to pickled cucumber, we picked the sauerkraut.
Why?
Both of these fermented foods can give a gut-healthy microbiome boost, but how do they stack up otherwise?
In terms of macros, sauerkraut has more protein, carbs, and fiber. They are both low glycemic index foods, so we’ll go with the one that has more fiber out of the two, and that’s the ‘kraut.
In the category of vitamins, sauerkraut has more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, and choline, while pickled cucumbers have more of vitamins A and K. An easy win for sauerkraut.
When it comes to minerals, sauerkraut has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pickled cucumbers are not higher in any mineral, except sodium (on average, pickled cucumbers have about 2x the sodium of sauerkraut). Another clear win for sauerkraut.
In short, enjoy either or both in moderation, but it’s clear which boasts the most nutritional benefits, and that’s the sauerkraut!
Want to learn more?
You might like to read:
Make Friends With Your Gut (You Can Thank Us Later)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Natural Tips for Falling Asleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
How to get to sleep at night as fast and as naturally as possible? Thank you!
We’ll definitely write more on that! You might like these articles we wrote already, meanwhile:
- Beating The Insomnia Blues ← this one is general advice and tips
- Time For Some Pillow Talk ← this one compares and reviews some popular sleep apps
- Insomnia? High Blood Pressure? Try these! ← this one tackles the matter from a dietary angle
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blueberries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blueberries to elderberries, we picked the elderberries.
Why?
Both are certainly top-tier fruits! But…
In terms of macros, elderberries have more than 2x the fiber, while the two berries are approximately equal on other macros. An easy win for elderberries in this category.
In the category of vitamins, blueberries have more of vitamins E, K, and choline, while elderberries have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, and C, scoring another win for elderberries here.
When it comes to minerals, blueberries have more magnesium, manganese, and zinc, while elderberries have more calcium, copper, iron, phosphorus, potassium, and selenium—one more win for elderberries.
In terms of phytochemicals, both berries are (like most berries) an abundant source of polyphenols, but elderberries have more, including more quercetin, too.
Adding up the sections makes for a convincing win for elderberries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Herbs For Evidence-Based Health & Healing ← elderberry significantly hastens recovery from upper respiratory viral infections 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: