How To Keep Warm (Without Sweat Patches!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I saw an advert on the subway for a pillow spray that guarantees a perfect night’s sleep. What does the science say about smells/sleep?❞
That is certainly a bold claim! Unless it’s contingent, e.g. “…or your money back”. Because otherwise, it absolutely cannot guarantee that.
There is some merit:
❝Odors can modulate the latency to sleep onset, as well as the quality and duration of sleep. Olfactory modulation of sleep may be mediated by direct synaptic interaction between the olfactory system and sleep control nuclei, and/or indirectly through odor modulation of arousal and respiration.
Such modulation appears most heavily influenced by past associations and expectations about the odor, beyond any potential direct physicochemical effect❞
Source: Reciprocal relationships between sleep and smell
Translating that from sciencese:
Sometimes we find pleasant smells relaxing, and placebo effect also helps.
That “any potential direct physiochemical effect”, though, when it does occur, is things like this…
Read: Odor blocking of stress hormone responses
…but that’s a mouse study, and those odors may only work to block three specific mouse stress responses to three specific stressors: physical restraint, predator odor, and male–male confrontation.
In other words: if, perchance, those three things are not what’s stressing you in bed at night (we won’t make assumptions), and/or you are not a mouse, it may not help.
(and this, dear readers, is why we must read articles, and not just headlines!)
But! If you are going to go for a pillow fragrance, something well-associated with being relaxing and soporific, such as lavender, is the way to go:
- Effects of aromatherapy on sleep quality and anxiety of patients
- Effects of Aromatherapy on the Anxiety, Vital Signs, and Sleep Quality of Percutaneous Coronary Intervention Patients in Intensive Care Units
- Effect of lavender aromatherapy on vital signs and perceived quality of sleep in the intermediate care unit: a pilot study
tl;dr = patients found lavender fragrances relaxing, experienced less anxiety, got better sleep (significantly or insignificantly, depending on the study) and enjoyed lower blood pressure (significantly or insignificantly, depending on the study).
PS: this writer uses a pillow spray like this one
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Can’t Skimp On Amino Acids
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our body requires 20 amino acids (the building blocks of protein), 9 of which it can’t synthesize (thus called: “essential”) and absolutely must get from food. Normally, we get these amino acids from protein in our diet, and we can also supplement them by taking amino acid supplements if we wish.
Specifically, we require (per kg of bodyweight) a daily average of:
- Histidine: 10 mg
- Isoleucine: 20 mg
- Leucine: 39 mg
- Lysine: 30 mg
- Methionine: 10.4 mg
- Phenylalanine*: 25 mg
- Threonine: 15 mg
- Tryptophan: 4 mg
- Valine: 26 mg
*combined with the non-essential amino acid tyrosine
Source: Protein and Amino Acid Requirements In Human Nutrition: WHO Technical Report
Why this matters
A lot of attention is given to protein, and making sure we get enough of it, especially as we get older, because the risk of sarcopenia (muscle mass loss) increases with age:
However, not every protein comes with a complete set of essential amino acids, and/or have only trace amounts of of some amino acids, meaning that a dietary deficiency can arrive if one’s diet is too restrictive.
And, if we become deficient in even just one amino acid, then bad things start to happen quite soon. We only have so much space, so we’re going to oversimplify here, but:
- Histidine: is needed to produce histamine (vital for immune responses, amongst other things), and is also important for maintaining the myelin sheaths on nerve cells.
- Isoleucine: is very involved in muscle metabolism and makes up the bulk of muscle tissue.
- Leucine: is critical for muscle synthesis and repair, as well as wound healing in general, and blood sugar regulation.
- Lysine: is also critical in muscle synthesis, as well as calcium absorption and hormone production, as well as making collagen.
- Methionine: is very important for energy metabolism, zinc absorption, and detoxification.
- Phenylalanine: is a necessary building block of a lot of neurotransmitters, as well as being a building block of some amino acids not listed here (i.e., the ones your body synthesizes, but can’t without phenylalanine).
- Threonine: is mostly about collagen and elastin production, and is also very important for your joints, as well as fat metabolism.
- Tryptophan: is the body’s primary precursor to serotonin, so good luck making the latter without the former.
- Valine: is mostly about muscle growth and regeneration.
So there you see, the ill effects of deficiency can range from “muscle atrophy” to “brain stops working” and “bones fall apart” and more. In short, any essential amino acid deficiency not remedied will ultimately result in death; we literally become non-viable as organisms without these 9 things.
What to do about it (the “life hack” part)
Firstly, if you eat a lot of animal products, those are “complete” proteins, meaning that they contain all 9 essential amino acids in sensible quantities. The reason that all animal products have these, is because they are just as essential for the other animals as they are for us, so they, just like us, must consume (and thus contain) them.
However, a lot of animal products come with other health risks:
Do We Need Animal Products To Be Healthy? ← this covers which animal products are definitely very health-risky, and which are probably fine according to current best science
…so many people may prefer to get more (or possibly all) dietary protein from plants.
However, plants, unlike us, do not need to consume all 9 essential amino acids, and this may or may not contain them all.
Soy is famously a “complete” protein insofar as it has all the amino acids we need.
But what if you’re allergic to soy?
Good news! Peas are also a “complete” protein and will do the job just fine. They’re also usually cheaper.
Final note
An oft-forgotten thing is that some other amino acids are “conditionally essential”, meaning that while we can technically synthesize them, sometimes we can’t synthesize enough and must get them from our diet.
The conditions that trigger this “conditionally essential” status are usually such things as fighting a serious illness, recovering from a serious injury, or pregnancy—basically, things where your body has to work at 110% efficiency if it wants to get through it in one piece, and that extra 10% has to come from somewhere outside the body.
Examples of commonly conditionally essential amino acids are arginine and glycine.
Arginine is critical for a lot of cell-signalling processes as well as mitochondrial function, as well as being a precursor to other amino acids, including creatine.
As for glycine?
Check out: The Sweet Truth About Glycine
Enjoy!
Share This Post
-
How much weight do you actually need to lose? It might be a lot less than you think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re one of the one in three Australians whose New Year’s resolution involved losing weight, it’s likely you’re now contemplating what weight-loss goal you should actually be working towards.
But type “setting a weight loss goal” into any online search engine and you’ll likely be left with more questions than answers.
Sure, the many weight-loss apps and calculators available will make setting this goal seem easy. They’ll typically use a body mass index (BMI) calculator to confirm a “healthy” weight and provide a goal weight based on this range.
Your screen will fill with trim-looking influencers touting diets that will help you drop ten kilos in a month, or ads for diets, pills and exercise regimens promising to help you effortlessly and rapidly lose weight.
Most sales pitches will suggest you need to lose substantial amounts of weight to be healthy – making weight loss seem an impossible task. But the research shows you don’t need to lose a lot of weight to achieve health benefits.
Using BMI to define our target weight is flawed
We’re a society fixated on numbers. So it’s no surprise we use measurements and equations to score our weight. The most popular is BMI, a measure of our body weight-to-height ratio.
BMI classifies bodies as underweight, normal (healthy) weight, overweight or obese and can be a useful tool for weight and health screening.
But it shouldn’t be used as the single measure of what it means to be a healthy weight when we set our weight-loss goals. This is because it:
- fails to consider two critical factors related to body weight and health – body fat percentage and distribution
- does not account for significant differences in body composition based on gender, ethnicity and age.
How does losing weight benefit our health?
Losing just 5–10% of our body weight – between 6 and 12kg for someone weighing 120kg – can significantly improve our health in four key ways.
1. Reducing cholesterol
Obesity increases the chances of having too much low-density lipoprotein (LDL) cholesterol – also known as bad cholesterol – because carrying excess weight changes how our bodies produce and manage lipoproteins and triglycerides, another fat molecule we use for energy.
Having too much bad cholesterol and high triglyceride levels is not good, narrowing our arteries and limiting blood flow, which increases the risk of heart disease, heart attack and stroke.
But research shows improvements in total cholesterol, LDL cholesterol and triglyceride levels are evident with just 5% weight loss.
2. Lowering blood pressure
Our blood pressure is considered high if it reads more than 140/90 on at least two occasions.
Excess weight is linked to high blood pressure in several ways, including changing how our sympathetic nervous system, blood vessels and hormones regulate our blood pressure.
Essentially, high blood pressure makes our heart and blood vessels work harder and less efficiently, damaging our arteries over time and increasing our risk of heart disease, heart attack and stroke.
Losing weight can lower your blood pressure.
Prostock-studio/ShutterstockLike the improvements in cholesterol, a 5% weight loss improves both systolic blood pressure (the first number in the reading) and diastolic blood pressure (the second number).
A meta-analysis of 25 trials on the influence of weight reduction on blood pressure also found every kilo of weight loss improved blood pressure by one point.
3. Reducing risk for type 2 diabetes
Excess body weight is the primary manageable risk factor for type 2 diabetes, particularly for people carrying a lot of visceral fat around the abdomen (belly fat).
Carrying this excess weight can cause fat cells to release pro-inflammatory chemicals that disrupt how our bodies regulate and use the insulin produced by our pancreas, leading to high blood sugar levels.
Type 2 diabetes can lead to serious medical conditions if it’s not carefully managed, including damaging our heart, blood vessels, major organs, eyes and nervous system.
Research shows just 7% weight loss reduces risk of developing type 2 diabetes by 58%.
4. Reducing joint pain and the risk of osteoarthritis
Carrying excess weight can cause our joints to become inflamed and damaged, making us more prone to osteoarthritis.
Observational studies show being overweight doubles a person’s risk of developing osteoarthritis, while obesity increases the risk fourfold.
Small amounts of weight loss alleviate this stress on our joints. In one study each kilogram of weight loss resulted in a fourfold decrease in the load exerted on the knee in each step taken during daily activities.
Losing weight eases stress on joints.
Shutterstock/Rostislav_SedlacekFocus on long-term habits
If you’ve ever tried to lose weight but found the kilos return almost as quickly as they left, you’re not alone.
An analysis of 29 long-term weight-loss studies found participants regained more than half of the weight lost within two years. Within five years, they regained more than 80%.
When we lose weight, we take our body out of its comfort zone and trigger its survival response. It then counteracts weight loss, triggering several physiological responses to defend our body weight and “survive” starvation.
Just as the problem is evolutionary, the solution is evolutionary too. Successfully losing weight long-term comes down to:
losing weight in small manageable chunks you can sustain, specifically periods of weight loss, followed by periods of weight maintenance, and so on, until you achieve your goal weight
making gradual changes to your lifestyle to ensure you form habits that last a lifetime.
Setting a goal to reach a healthy weight can feel daunting. But it doesn’t have to be a pre-defined weight according to a “healthy” BMI range. Losing 5–10% of our body weight will result in immediate health benefits.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Potatoes & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝My other half considers potatoes a wonder food, except when fried. I don’t. I find, when I am eating potatoes I put on weight; and, when I’m not eating them, I lose it. Also, although I can’t swear to it, potatoes also make me feel a little anxious (someone once told me it could have something to do with where they are on the “glycemic index”). What does the science say?❞
The glycemic index of potatoes depends on the kind of potato (obviously) and also, less obviously, how it’s prepared. For a given white potato, boiling (which removes a lot of starch) might produce a GI of around 60, while instant mash (basically: potato starch) can be more like 80. For reference, pure glucose is 100. And you probably wouldn’t take that in the same quantity you’d take potato, and expect to feel good!
So: as for anxiety, it could be, since spiked blood sugars can cause mood swings, including anxiety.
Outside of the matter of blood sugars, the only reference we could find for potatoes causing anxiety was fried potatoes specifically:
❝frequent fried food consumption, especially fried potato consumption, is strongly associated with 12% and 7% higher risk of anxiety and depression, respectively❞
…which heavily puts the blame not on the potatoes themselves, but on acrylamide (the orange/brown stuff that is made by the Maillard reaction of cooking starches in the absence of water, e.g. by frying, roasting, etc).
Here’s a very good overview of that, by the way:
A Review on Acrylamide in Food: Occurrence, Toxicity, and Mitigation Strategies
Back on the core topic of potatoes and GI and blood sugar spikes and anxiety, you might benefit from a few tweaks that will allow you to enjoy potatoes without spiking blood sugars:
10 Ways To Balance Blood Sugars
Enjoy!
Share This Post
Related Posts
-
What’s Your Vascular Dementia Risk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We often say that “what’s good for your heart is good for your brain”, and this is because the former feeds the latter, with oxygen and nutrients, and also clears away detritus like beta-amyloid (associated with Alzheimer’s) and alpha-synuclein (associated with Parkinson’s).
For more on those, see: How To Clean Your Brain (Glymphatic Health Primer)
For this reason, there are many risk factors that apply equally cardiovascular disease (CVD), and neurodegenerative diseases like Alzheimer’s and other vascular dementias, as well as stroke risk.
The link between the two has also been studied; recently a team of scienists led by Dr. Anisa Dhana asked the question:
❝What is the association between cardiovascular health (CVH) and biomarkers of neurodegeneration, including neurofilament light chain and total tau?❞
To answer this, they looked at data from more than 10,000 Americans aged 65+; of these, they were able to get serum samples from 5,470 of them, and tested those samples for the biomarkers of neurodegeneration mentioned above.
They then tabulated the results with cardiovascular health scores based on the American Heart Association (AHA)’s “Life’s Simple 7” tool, and found, amongst other things:
- 34.6% of participants carried the APOE e4 allele, a genetic risk factor for Alzheimer’s.
- Higher CVH scores were associated with lower NfL levels, but not with t-tau concentrations.
- APOE e4 carriers with high CVH had significantly lower NfL levels.
- Race did not influence the CVH-NfL relationship.
- Higher CVH was linked to a slower annual increase in NfL levels but did not affect t-tau changes.
- Over 10 years, participants with the lowest CVH scores saw a 7.1% annual increase in NfL levels, while those with the highest CVH scores had a 5.2% annual increase.
- Better CVH is linked to lower serum NfL levels, regardless of age, sex, or race.
- CVH is particularly crucial for APOE e4 carriers
In other words: higher cardiovascular health meant lower markers of neurodegeneration, and this not only still held true for APOE e4 carriers, but also, the benefits actually even more pronounced in those participants.
You may be wondering: “but it said it helped with NfL levels, not t-tau concentrations?” And, indeed, it is so. But this means that the overall neurodegeneration risk is still inversely proportional to cardiovascular health; it just means it’s not a magical panacea and we must still do other things too.
See also: How To Reduce Your Alzheimer’s Risk
And as for the study, you can read the paper itself in full here:
Cardiovascular Health and Biomarkers of Neurodegenerative Disease in Older Adults
Life’s Simple 7
We mentioned that they used the AHA’s “Life’s Simple 7” tool to assess cardiovascular health; it is indeed simple, but important. Here it is:
Metric Poor Intermediate Ideal Current smoking Yes Former ≤12 mo Never or quit >12 mo BMI, kg/m2 ≥30 25–29.9 <25 Physical activity None 1–149 min/wk of moderate activity or 1–74 min/wk of vigorous activity or 1–149 min/wk of moderate and vigorous activity ≥150 min/wk of moderate activity or ≥75 min/wk of vigorous activity or ≥150 min/wk of moderate and vigorous activity Diet pattern score* 0–1 2–3 4–5 Total cholesterol, mg/dL ≥240 200–239 or treated to goal <200 Blood pressure, mm Hg SBP ≥140 or DBP ≥90 SBP 120–139 or DBP 80–89 or treated to goal <120/<80 Fasting plasma glucose, mg/dL ≥126 100–125 or treated to goal <100 *Each of the following 5 diet elements is given a score of 1: (1) ≥4.5 cups/day of fruits and vegetables; (2) ≥2 servings/week of fish; (3) ≥3 servings/day of whole grains; (4) no more than 36 oz/wk of sugar‐sweetened beverages; and (5) no more than 1500 mg/d of sodium.
As the AHA notes,
❝Unfortunately, 99% of the U.S. adult population has at least one of seven cardiovascular health risks: tobacco use,
poor diet, physical inactivity, unhealthy weight, high blood pressure, high cholesterol or high blood glucose.❞It then goes on to talk about the financial burden of this on employers, but this was taken from a workplace health resource, and we recognize the rest of it won’t be of pressing concern for most of our readers. In case you are interested though, here it is:
American Heart Association | Life’s Simple 7® Journey to Health™
For a more practical (if you’re just a private individual and employee healthcare is not your main concern) overview, see:
Want to know more?
Here are some very good starting points for improving each of those 7 metrics, as necessary:
- Which Addiction-Quitting Methods Work Best?
- How To Lose Weight (Healthily!)
- The Doctor Who Wants Us To Exercise Less, & Move More
- Which Diet? Top Diets Ranked By Experts
- Lower Cholesterol Naturally, Without Statins
- 10 Ways To Lower Blood Pressure Naturally
- 10 Ways To Balance Your Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Is “75 Hard”?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
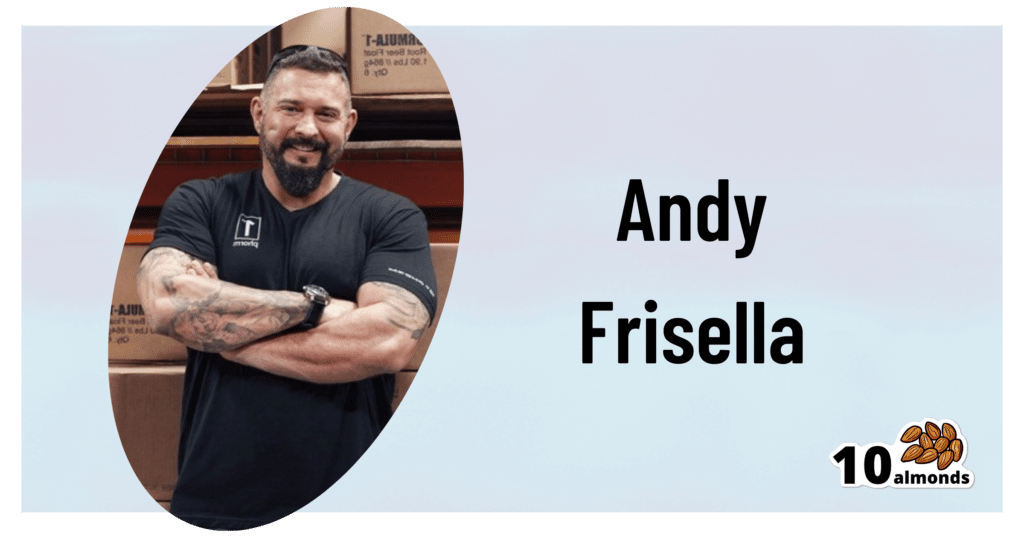
This is Andy Frisella. He’s not a doctor, scientist, nutritionist, personal trainer, or professional athlete, but he has kicked off a viral fitness challenge, so let’s take a look at it:
What it is
Firstly, Frisella asserts that it’s not a fitness challenge, but rather, he describes it as a “transformative mental toughness program”.
Here’s what it consists of:
- Follow a healthy diet plan with no deviations from it (i.e. no “cheat days”)
- Abstain from alcohol
- Exercise 2x per day, 45 minutes each
- One of the exercise sessions each day must be outside
- No rest days
- Drink 3.5 liters of water per day
And the duration? 75 days, hence the name of the
fitness challengetransformative mental toughness program.Why it is
Frisella’s rationale is:
- we must cultivate mental toughness by doing hard things
- allowing ourselves any deviation would be a sign of mental weakness
- if we allow ourselves to deviate, it becomes a habit
For this reason, he does not “allow” any substitutions, for example if somebody wants to do such-and-such a thing slightly differently instead. We put “allow” in quotation marks because of course, he’s not the boss of you, but per the rules of his challenge, at least.
These reasonings are in and of themselves somewhat sound, however, we at 10almonds would argue:
- before doing hard things, it is good to first consider “is it a good idea?” (amputating your leg using only a spork is a “hard thing”, and demonstrates incredible mental toughness, but that doesn’t make it a good idea)
- while being able to decide to do a thing and then do it is great characteristic to have, it’s good to first consider science; for example, restrictive diets with no flexibility simply do not work, and our bodies do require adequate rest, especially if being pushed through hard things, or problems will happen (injuries, illnesses, etc).
- while it’s true that allowing ourselves to deviate can become a habit, it’s good to first consider what habits we want to make, and make those habits, instead of potentially unsustainable or even simply unpleasant ones.
See also: What Flexible Dieting Really Means: When Flexibility Is The Dish Of The Day
And for that matter: How To Really Pick Up (And Keep!) Those Habits
Want a “75 Gentle” instead?
If you like the idea of making new habits, but are not sure if extreme (and perhaps arbitrary) standards are the ones you want to hold, check out:
Cori Lefkowith’s 25 Healthy Habits That Will Change Your Life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, you do need to clean your tongue. Here’s how and why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Has your doctor asked you to stick out your tongue and say “aaah”? While the GP assesses your throat, they’re also checking out your tongue, which can reveal a lot about your health.
The doctor will look for any changes in the tongue’s surface or how it moves. This can indicate issues in the mouth itself, as well as the state of your overall health and immunity.
But there’s no need to wait for a trip to the doctor. Cleaning your tongue twice a day can help you check how your tongue looks and feels – and improve your breath.
luisrsphoto/Shutterstock What does a healthy tongue look like?
Our tongue plays a crucial role in eating, talking and other vital functions. It is not a single muscle but rather a muscular organ, made up of eight muscle pairs that help it move.
The surface of the tongue is covered by tiny bumps that can be seen and felt, called papillae, giving it a rough surface.
These are sometimes mistaken for taste buds – they’re not. Of your 200,000-300,000 papillae, only a small fraction contain taste buds. Adults have up to 10,000 taste buds and they are invisible to the naked eye, concentrated mainly on the tip, sides and back of the tongue. https://www.youtube.com/embed/uYvpUl7li9Y?wmode=transparent&start=0
A healthy tongue is pink although the shade may vary from person to person, ranging from dark to light pink.
A small amount of white coating can be normal. But significant changes or discolouration may indicate a disease or other issues.
How should I clean my tongue?
Cleaning your tongue only takes around 10-15 seconds, but it’s is a good way to check in with your health and can easily be incorporated into your teeth brushing routine.
Build-up can occur if you stop brushing or scraping your tongue even for a few days. Anthony Shkraba/Pexels You can clean your tongue by gently scrubbing it with a regular toothbrush. This dislodges any food debris and helps prevent microbes building up on its rough textured surface.
Or you can use a special tongue scraper. These curved instruments are made of metal or plastic, and can be used alone or accompanied by scrubbing with your toothbrush.
Your co-workers will thank you as well – cleaning your tongue can help combat stinky breath. Tongue scrapers are particularly effective at removing the bacteria that commonly causes bad breath, hidden in the tongue’s surface.
What’s that stuff on my tongue?
So, you’re checking your tongue during your twice-daily clean, and you notice something different. Noting these signs is the first step. If you observe any changes and they worry you, you should talk to your GP.
Here’s what your tongue might be telling you.
White coating
Developing a white coating on the tongue’s surface is one of the most common changes in healthy people. This can happen if you stop brushing or scraping the tongue, even for a few days.
In this case, food debris and microbes have accumulated and caused plaque. Gentle scrubbing or scraping will remove this coating. Removing microbes reduces the risk of chronic infections, which can be transferred to other organs and cause serious illnesses.
Scrubbing or scraping your tongue only takes around ten seconds and can be done while brushing your teeth. Ketut Subiyanto/Pexels Yellow coating
This may indicate oral thrush, a fungal infection that leaves a raw surface when scrubbed.
Oral thrush is common in elderly people who take multiple medications or have diabetes. It can also affect children and young adults after an illness, due to the temporary suppression of the immune system or antibiotic use.
If you have oral thrush, a doctor will usually prescribe a course of anti-fungal medication for at least a month.
Black coating
Smoking or consuming a lot of strong-coloured food and drink – such as tea and coffee, or dishes with tumeric – can cause a furry appearance. This is known as a black hairy tongue. It’s not hair, but an overgrowth of bacteria which may indicate poor oral hygiene.
Smoking can add to poor oral hygiene and make the tongue look black. Sophon Nawit/Shutterstock Pink patches
Pink patches surrounded by a white border can make your tongue look like a map – this is called “geographic tongue”. It’s not known what causes this condition, which usually doesn’t require treatment.
Pain and inflammation
A red, sore tongue can indicate a range of issues, including:
- nutritional deficiencies such as folic acid or vitamin B12
- diseases including pernicious anaemia, Kawasaki disease and scarlet fever
- inflammation known as glossitis
- injury from hot beverages or food
- ulcers, including cold sores and canker sores
- burning mouth syndrome.
Dryness
Many medications can cause dry mouth, also called xerostomia. These include antidepressants, anti-psychotics, muscle relaxants, pain killers, antihistamines and diuretics. If your mouth is very dry, it may hurt.
What about cancer?
White or red patches on the tongue that can’t be scraped off, are long-standing or growing need to checked out by a dental professional as soon as possible, as do painless ulcers. These are at a higher risk of turning into cancer, compared to other parts of the mouth.
Oral cancers have low survival rates due to delayed detection – and they are on the rise. So checking your tongue for changes in colour, texture, sore spots or ulcers is critical.
Dileep Sharma, Professor and Head of Discipline – Oral Health, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: