Bird Flu: Children At High Risk; Older Adults Not So Much
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this week’s news roundup…
Children at highest risk for bird flu
When a new infectious disease comes out, we get used to hearing the usual refrain, “children, the elderly, those with compromised immune systems” are those considered at greatest risk, and therefore first in line for vaccines.
In this case, however, it seems that older adults appear to be rather more resilient to bird flu than children, and it’s noted that early childhood influenza exposure can elicit immune responses that last a lifetime. For those whose lifetime was not curtailed by the initial infection, that means they may enjoy extra defenses now.
You may be wondering whether this headline statement is just a hypothesis based on that, and no, it’s not. It’s a (albeit tentative, like most things in any emerging science, as responses to a novel infection will always be) conclusion based on blood samples from a little over 150 people born between 1927 and 2026 (so, quite a range), and examining the antibodies found therein; adults born prior to 1968 are the ones who are most likely to have been exposed to H1N1 or H2N2 in childhood, resulting in them now having antibodies that work against the H5N1 virus (but still, by all means please do take all sensible precautions anyway!):
Read in full: Older adults might be more resistant to bird flu infections than children, research finds
Related: What you need to know about H5N1 bird flu
GLP-1 Receptor Agonists? They work, but at what cost?
We’re not talking about the side effects this time! Nor even the “what happens if you stop taking it” problems.
Rather, the “cost” in this case is the literal financial cost; out of a selection of weight loss drugs examined, semaglutide (such as Ozempic and Wegovy) and tirzepatide (such as Zepbound and Eli Lilly) were the only ones deemed to not be cost-effective for patients:
Read in full: Semaglutide, tirzepatide not deemed cost-effective obesity therapies despite benefits
Related: Most People Who Start GLP-1 RAs Quit Them Within A Year (Here’s Why)
Inflammation now, brittle bones later
Chronic inflammation is a root cause of many diseases (due in part to how it weakens the immune system, but also because of how the body functions so badly in general when it’s constantly at war with itself, as is the case in chronic inflammation), and it worsens many diseases that it doesn’t outright cause.
In this case, the new science is that chronic inflammation also makes changes to bone density over time.
Spoiler: the changes are not good changes
Furthermore, this holds true for young people also, not just people in the usual demographic that one would expect for brittle bones (especially: older women with untreated menopause, but also just anyone older than middle-aged in general, as most people start losing about 1% of bone density per year after their mid-30s).
Read in full: Inflammation proteins linked to bone density changes over time
Related: The Bare-Bones Truth About Osteoporosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grapefruit vs Orange – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to orange, we picked the orange.
Why?
It’s easy, when guessing which is the healthier out of two things, to guess that the more expensive or perhaps less universally available one is the healthier. But it’s not always so, and today is one of those cases!
In terms of macros, they are very similar fruits, with almost identical levels of carbohydrates, proteins, and fats, as well as water. Looking more carefully, we find that grapefruit’s sugars contain a slightly high proportion of fructose; not enough to make it unhealthy by any means (indeed, no whole unprocessed fruit is unhealthy unless it’s literally poisonous), but it is a thing to note if we’re micro-analysing the macronutrients. Also, oranges have slightly more fiber, which is always a plus.
When it comes to vitamins, oranges stand out with more of vitamins B1, B2, B3, B6, B9, C, and E, while grapefruit boasts more vitamin A (hence its color). Still, we’re calling this category another win for oranges.
In the category of minerals, oranges again sweep with more calcium, copper, iron, magnesium, manganese, potassium, and selenium, while grapefruit has just a little more phosphorus. So, another easy win for oranges.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold. It can also be found in lower quantities in Seville (sour) oranges, and it’s not present (or at least, if it is, it’s in truly tiny quantities) in most oranges.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, today’s sections add up to an overwhelming win for oranges!
Want to learn more?
You might like to read:
Take care!
Share This Post
-
The Big Book of Kombucha – by Hannah Crum & Alex LaGory
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve been thinking “I should get into kombucha”, then this is the universe prompting you, because with in this book’s 400 pages is all the information you need and more.
Because, it’s understandable to be wary when starting out, from “what if my jar explodes” to “what if I poison my family”, but the authors (and photographer) take every care to ensure that everything goes perfectly, guiding us through everything from start to finish, including very many high-quality color photos of what things should (and shouldn’t) look like.
On which note, that does mean that to enjoy the color you should get a physical copy or Kindle Fire, not a Kindle e-ink version (as then it’d be black and white).
There’s also a comprehensive section on troubleshooting, as well as hundreds of recipes for all kinds of flavors and occasions.
Bottom line: in the category of books that could reasonably be called “The Bible of…”, this one’s the “The Bible of Kombucha”.
Click here to check out The Big Book Of Kombucha, and get brewing!
Share This Post
-
Measles, Memory, & Mouths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Three important items from this week’s health news:
It’s not about obesity
This news is based on a rodent study, so we don’t know for sure if it’s applicable to humans yet, but there’s no reason to expect that it won’t be.
The crux of the matter is that while it’s long been assumed that when it comes to diet and cognitive decline, obesity is the main driver of problems, it turns out that rats fed a high fat diet—for three days or three months—did much worse in memory tests.
This was observed in older rats, but not in younger ones—the researchers hypothesized that the younger rats benefited from their ability to activate compensatory anti-inflammatory responses, which the older rats could not.
Notably, the three-day window of high-fat diet wasn’t sufficient to cause any metabolic problems or obesity yet, but markers of neuroinflammation skyrocketed immediately, and memory test scores declined at the same rate:
Read in full: High-fat diet could cause memory problems in older adults after just a few days
Related: Can Saturated Fats Be Healthy?
Vax, Lies, & Mortality Rates
Measles is making a comeback in the US.
100 cases were reported in Gaines county, TX, recently, with 1 death there so far (an unvaccinated child). And of course, it’s spreading; in the neighboring Lea county, NM, they now have an outbreak of 30 confirmed cases, and 1 death there so far (an unvaccinated adult).
This comes with the rise of the anti-vax movement which comes with a lot of misleading rhetoric (and some things that are simply factually incorrect), and an increase in “measles parties” whereby children are deliberately exposed to measles in order to “get it out of the way” and confer later immunity. That technically does work if everyone survives, but the downside is your child may die:
Read in full: New Mexico reports 30 measles cases a day after second US death in decade
Related: 4 Ways Vaccine Skeptics Mislead You on Measles and More
What your gums say about your hormones
Times of hormonal change (so, including menopause) can show in one’s gums,
❝Recent research shows that 84% of women over 50 did not know that menopause could affect their oral health; 70% of menopausal women reported at least one new oral health symptom (like dry mouth or sensitive gums), yet only 2% had discussed these issues with their dentist.❞
Because gum disease can progress painlessly for a long while, it’s very important to stay on top of any changes, and look for the cause (enlisting the help of your doctor and/or dentist), lest you find yourself very far into periodontal disease when it could have been stopped and reversed much more easily before getting that bad.
Different life stages’ hormonal changes have different effects; the article we’ll link below also list puberty, menstrual variations, and pregnancy, but for brevity we’ll just quote what they say about menopause:
❝Menopause: the hormonal changes of menopause—primarily the drop in estrogen—can lead to oral health issues. Many menopausal women experience dry mouth, which increases the risk of cavities and gum disease, since saliva helps protect teeth. Gums may also recede or become more sensitive, and some women feel burning sensations in the mouth or changes in taste.❞
As for the rest…
Read in full: Gum health: A key indicator of women’s overall well-being
Related: How To Regrow Receding Gums
Take care!
Share This Post
Related Posts
-
When BMI Doesn’t Measure Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When BMI Doesn’t Quite Measure Up
Last month, we did a “Friday Mythbusters” edition of 10almonds, tackling many of the misconceptions surrounding obesity. Amongst them, we took a brief look at the usefulness (or lack thereof) of the Body Mass Index (BMI) scale of weight-related health for individuals. By popular subscriber request, we’re now going to dive a little deeper into that today!
The wrong tool for the job
BMI was developed as a tool to look at large-scale demographic trends, stemming from a population study of white European men, who were for the purpose of the study (the widescale health of the working class in that geographic area in that era), considered a reasonable default demographic.
In other words: as a system, it’s now being used in a way it was never made for, and the results of that misappropriation of an epidemiological tool for individual health are predictably unhelpful.
If you want to know yours…
Here’s the magic formula for calculating your BMI:
- Metric: divide your weight in kilograms by your height in square meters
- Imperial: divide your weight in pounds by your height in square inches and then multiply by 703
“What if my height doesn’t come in square meters or square inches, because it’s a height, not an area?”
We know. Take your height and square it anyway. If this seems convoluted and arbitrary, yes, it is.
But!
While on the one hand it’s convoluted and arbitrary… On the other hand, it’s also a gross oversimplification. So, yay for the worst of both worlds?
If you don’t want to grab a calculator, here’s a quick online tool to calculate it for you.
So, how did you score?
According to the CDC, a BMI score…
- Under 18.5 is underweight
- 18.5 to 24.9 is normal
- 25 to 29.9 is overweight
- 30 and over is obese
And, if we’re looking at a representative sample of the population, where the representation is average white European men of working age, that’s not a bad general rule of thumb.
For the rest of us, not so representative
BMI is a great and accurate tool as a rule of thumb, except for…
Women
An easily forgotten demographic, due to being a mere 51% of the world’s population, women generally have a higher percentage of body fat than men, and this throws out BMI’s usefulness.
If pregnant or nursing
A much higher body weight and body fat percentage—note that these are two things, not one. Some of the extra weight will be fat to nourish the baby; some will be water weight, and if pregnant, some will be the baby (or babies!). BMI neither knows nor cares about any of these things. And, this is a big deal, because BMI gets used by healthcare providers to judge health risks and guide medical advice.
People under the age of 16 or over the age of 65
Not only do people below and above those ages (respectively) tend to be shorter—which throws out the calculations and mean health risks may increase before the BMI qualifies as overweight—but also:
- BMI under 23 in people over the age of 65 is associated with a higher health risk
- A meta-analysis showed that a BMI of 27 was the best in terms of decreased mortality risk for the over-65 age group
This obviously flies in the face of conventional standards regards BMI—as you’ll recall from the BMI brackets we listed above.
Read the science: BMI and all-cause mortality in older adults: a meta-analysis
Athletic people
A demographic often described in scientific literature as “athletes”, but that can be misleading. When we say “athletes”, what comes to mind? Probably Olympians, or other professional sportspeople.
But also athletic, when it comes to body composition, are such people as fitness enthusiasts and manual laborers. Which makes for a lot more people affected by this!
Athletic people tend to have more lean muscle mass (muscle weighs more than fat), and heavier bones (can’t build strong muscles on weak bones, so the bones get stronger too, which means denser)… But that lean muscle mass can actually increase metabolism and help ward off many of the very same things that BMI is used as a risk indicator for (e.g. heart disease, and diabetes). So people in this category will actually be at lower risk, while (by BMI) getting told they are at higher risk.
If not white
Physical characteristics of race can vary by more than skin color, relevant considerations in this case include, for example:
- Black people, on average, not only have more lean muscle mass and less fat than white people, but also, have completely different risk factors for diseases such as diabetes.
- Asian people, on average, are shorter than white people, and as such may see increased health risks before BMI qualifies as overweight.
- Hispanic people, on average, again have different physical characteristics that throw out the results, in a manner that would need lower cutoffs to be even as “useful” as it is for white people.
Further reading on this: BMI and the BIPOC Community
In summary:
If you’re an average white European working-age man, BMI can sometimes be a useful general guide. If however you fall into one or more of the above categories, it is likely to be inaccurate at best, if not outright telling the opposite of the truth.
What’s more useful, then?
For heart disease risk and diabetes risk both, waist circumference is a much more universally reliable indicator. And since those two things tend to affect a lot of other health risks, it becomes an excellent starting point for being aware of many aspects of health.
Pregnancy will still throw off waist circumference a little (measure below the bump, not around it!), but it will nevertheless be more helpful than BMI even then, as it becomes necessary to just increase the numbers a little, according to gestational month and any confounding factors e.g. twins, triplets, etc. Ask your obstetrician about this, as it’s beyond the scope of today’s newsletter!
As to what’s considered a risk:
- Waist circumference of more than 35 inches for women
- Waist circumference of more than 40 inches for men
These numbers are considered applicable across demographics of age, sex, ethnicity, and lifestyle.
There are more options than just waist circumference though; we delve into them in detail here:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
State Regulators Know Health Insurance Directories Are Full of Wrong Information. They’re Doing Little to Fix It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: America’s Mental Barrier:How Insurers Interfere With Mental Health Care
- Extensive Errors: Many states have sought to make insurers clean up their health plans’ provider directories over the past decade. But the errors are still widespread.
- Paltry Penalties: Most state insurance agencies haven’t issued a fine for provider directory errors since 2019. When companies have been penalized, the fines have been small and sporadic.
- Ghostbusters: Experts said that stricter regulations and stronger fines are needed to protect insurance customers from these errors, which are at the heart of so-called ghost networks.
These highlights were written by the reporters and editors who worked on this story.
To uncover the truth about a pernicious insurance industry practice, staffers with the New York state attorney general’s office decided to tell a series of lies.
So, over the course of 2022 and 2023, they dialed hundreds of mental health providers in the directories of more than a dozen insurance plans. Some staffers pretended to call on behalf of a depressed relative. Others posed as parents asking about their struggling teenager.
They wanted to know two key things about the supposedly in-network providers: Do you accept insurance? And are you accepting new patients?
The more the staffers called, the more they realized that the providers listed either no longer accepted insurance or had stopped seeing new patients. That is, if they heard back from the providers at all.
In a report published last December, the office described rampant evidence of these “ghost networks,” where health plans list providers who supposedly accept that insurance but who are not actually available to patients. The report found that 86% of the listed mental health providers who staffers had called were “unreachable, not in-network, or not accepting new patients.” Even though insurers are required to publish accurate directories, New York Attorney General Letitia James’ office didn’t find evidence that the state’s own insurance regulators had fined any insurers for their errors.
Shortly after taking office in 2021, Gov. Kathy Hochul vowed to combat provider directory misinformation, so there seemed to be a clear path to confronting ghost networks.
Yet nearly a year after the publication of James’ report, nothing has changed. Regulators can’t point to a single penalty levied for ghost networks. And while a spokesperson for New York state’s Department of Financial Services has said that “nation-leading consumer protections” are in the works, provider directories in the state are still rife with errors.
A similar pattern of errors and lax enforcement is happening in other states as well.
In Arizona, regulators called hundreds of mental health providers listed in the networks of the state’s most popular individual health plans. They couldn’t schedule visits with nearly 2 out of every 5 providers they called. None of those companies have been fined for their errors.
In Massachusetts, the state attorney general investigated alleged efforts by insurers to restrict their customers’ mental health benefits. The insurers agreed to audit their mental health provider listings but were largely allowed to police themselves. Insurance regulators have not fined the companies for their errors.
In California, regulators received hundreds of complaints about provider listings after one of the nation’s first ghost network regulations took effect in 2016. But under the new law, they have actually scaled back on fining insurers. Since 2016, just one plan was fined — a $7,500 penalty — for posting inaccurate listings for mental health providers.
ProPublica reached out to every state insurance commission to see what they have done to curb rampant directory errors. As part of the country’s complex patchwork of regulations, these agencies oversee plans that employers purchase from an insurer and that individuals buy on exchanges. (Federal agencies typically oversee plans that employers self-fund or that are funded by Medicare.)
Spokespeople for the state agencies told ProPublica that their “many actions” resulted in “significant accountability.” But ProPublica found that the actual actions taken so far do not match the regulators’ rhetoric.
“One of the primary reasons insurance commissions exist is to hold companies accountable for what they are advertising in their contracts,” said Dr. Robert Trestman, a leading American Psychiatric Association expert who has testified about ghost networks to the U.S. Senate Committee on Finance. “They’re not doing their job. If they were, we would not have an ongoing problem.”
Most states haven’t fined a single company for publishing directory errors since 2019. When they do, the penalties have been small and sporadic. In an average year, fewer than a dozen fines are issued by insurance regulators for directory errors, according to information obtained by ProPublica from almost every one of those agencies. All those fines together represent a fraction of 1% of the billions of dollars in profits made by the industry’s largest companies. Health insurance experts told ProPublica that the companies treat the fines as a “cost of doing business.”
Insurers acknowledge that errors happen. Providers move. They retire. Their open appointments get booked by other patients. The industry’s top trade group, AHIP, has told lawmakers that companies contact providers to verify that their listings are accurate. The trade group also has stated that errors could be corrected faster if the providers did a better job updating their listings.
But providers have told us that’s bogus. Even when they formally drop out of a network, they’re not always removed from the insurer’s lists.
The harms from ghost networks are real. ProPublica reported on how Ravi Coutinho, a 36-year-old entrepreneur from Arizona, had struggled for months to access the mental health and addiction treatment that was covered by his health plan. After nearly two dozen calls to the insurer and multiple hospitalizations, he couldn’t find a therapist. Last spring, he died, likely due to complications from excessive drinking.
Health insurance experts said that, unless agencies can crack down and issue bigger fines, insurers will keep selling error-ridden plans.
“You can have all the strong laws on the books,” said David Lloyd, chief policy officer with the mental health advocacy group Inseparable. “But if they’re not being enforced, then it’s kind of all for nothing.”
The problem with ghost networks isn’t one of awareness. States, federal agencies, researchers and advocates have documented them time and again for years. But regulators have resisted penalizing insurers for not fixing them.
Two years ago, the Arizona Department of Insurance and Financial Institutions began to probe the directories used by five large insurers for plans that they sold on the individual market. Regulators wanted to find out if they could schedule an appointment with mental health providers listed as accepting new patients, so their staff called 580 providers in those companies’ directories.
Thirty-seven percent of the calls did not lead to an appointment getting scheduled.
Even though this secret-shopper survey found errors at a lower rate than what had been found in New York, health insurance experts who reviewed Arizona’s published findings said that the results were still concerning.
Ghost network regulations are intended to keep provider listings as close to error-free as possible. While the experts don’t expect any insurer to have a perfect directory, they said that double-digit error rates can be harmful to customers.
Arizona’s regulators seemed to agree. In a January 2023 report, they wrote that a patient could be clinging to the “last few threads of hope, which could erode if they receive no response from a provider (or cannot easily make an appointment).”
Secret-shopper surveys are considered one of the best ways to unmask errors. But states have limited funding, which restricts how often they can conduct that sort of investigation. Michigan, for its part, mostly searches for inaccuracies as part of an annual review of a health plan. Nevada investigates errors primarily if someone files a complaint. Christine Khaikin, a senior health policy attorney for the nonprofit advocacy group Legal Action Center, said fewer surveys means higher odds that errors go undetected.
Some regulators, upon learning that insurers may not be following the law, still take a hands-off approach with their enforcement. Oregon’s Department of Consumer and Business Services, for instance, conducts spot checks of provider networks to see if those listings are accurate. If they find errors, insurers are asked to fix the problem. The department hasn’t issued a fine for directory errors since 2019. A spokesperson said the agency doesn’t keep track of how frequently it finds network directory errors.
Dave Jones, a former insurance commissioner in California, said some commissioners fear that stricter enforcement could drive companies out of their states, leaving their constituents with fewer plans to choose from.
Even so, staffers at the Arizona Department of Insurance and Financial Institutions wrote in the report that there “needs to be accountability from insurers” for the errors in their directories. That never happened, and the agency concealed the identities of the companies in the report. A department spokesperson declined to provide the insurers’ names to ProPublica and did not answer questions about the report.
Since January 2023, Arizonans have submitted dozens of complaints to the department that were related to provider networks. The spokesperson would not say how many were found to be substantiated, but the department was able to get insurers to address some of the problems, documents obtained through an open records request show.
According to the department’s online database of enforcement actions, not a single one of those companies has been fined.
Sometimes, when state insurance regulators fail to act, attorneys general or federal regulators intervene in their stead. But even then, the extra enforcers haven’t addressed the underlying problem.
For years, the Massachusetts Division of Insurance didn’t fine any company for ghost networks, so the state attorney general’s office began to investigate whether insurers had deceived consumers by publishing inaccurate directories. Among the errors identified: One plan had providers listed as accepting new patients but no actual appointments were available for months; another listed a single provider more than 10 times at different offices.
In February 2020, Maura Healey, who was then the Massachusetts attorney general, announced settlements with some of the state’s largest health plans. No insurer admitted wrongdoing. The companies, which together collect billions in premiums each year, paid a total of $910,000. They promised to remove providers who left their networks within 30 days of learning about that decision. Healey declared that the settlements would lead to “unprecedented changes to help ensure patients don’t have to struggle to find behavioral health services.”
But experts who reviewed the settlements for ProPublica identified a critical shortcoming. While the insurers had promised to audit directories multiple times a year, the companies did not have to report those findings to the attorney general’s office. Spokespeople for Healey and the attorney general’s office declined to answer questions about the experts’ assessments of the settlements.
After the settlements were finalized, Healey became the governor of Massachusetts and has been responsible for overseeing the state’s insurance division since she took office in January 2023. Her administration’s regulators haven’t brought any fines over ghost networks.
Healey’s spokesperson declined to answer questions and referred ProPublica to responses from the state’s insurance division. A division spokesperson said the state has taken steps to strengthen its provider directory regulations and streamline how information about in-network providers gets collected. Starting next year, the spokesperson said that the division “will consider penalties” against any insurer whose “provider directory is found to be materially noncompliant.”
States that don’t have ghost network laws have seen federal regulators step in to monitor directory errors.
In late 2020, Congress passed the No Surprises Act, which aimed to cut down on the prevalence of surprise medical bills from providers outside of a patient’s insurance network. Since then, the Centers for Medicare and Medicaid Services, which oversees the two large public health insurance programs, has reached out to every state to see which ones could handle enforcement of the federal ghost network regulations.
At least 15 states responded that they lacked the ability to enforce the new regulation. So CMS is now tasked with watching out for errors in directories used by millions of insurance customers in those states.
Julie Brookhart, a spokesperson for CMS, told ProPublica that the agency takes enforcement of the directory error regulations “very seriously.” She said CMS has received a “small number” of provider directory complaints, which the agency is in the process of investigating. If it finds a violation, Brookhart said regulators “will take appropriate enforcement action.”
But since the requirement went into effect in January 2022, CMS hasn’t fined any insurer for errors. Brookhart said that CMS intends to develop further guidelines with other federal agencies. Until that happens, Brookhart said that insurers are expected to make “good-faith” attempts to follow the federal provider directory rules.
Last year, five California lawmakers proposed a bill that sought to get rid of ghost networks around the state. If it passed, AB 236 would limit the number of errors allowed in a directory — creating a cap of 5% of all providers listed — and raise penalties for violations. California would become home to one of the nation’s toughest ghost network regulations.
The state had already passed one of America’s first such regulations in 2015, requiring insurers to post directories online and correct inaccuracies on a weekly basis.
Since the law went into effect in 2016, insurance customers have filed hundreds of complaints with the California Department of Managed Health Care, which oversees health plans for nearly 30 million enrollees statewide.
Lawyers also have uncovered extensive evidence of directory errors. When San Diego’s city attorney, Mara Elliott, sued several insurers over publishing inaccurate directories in 2021, she based the claims on directory error data collected by the companies themselves. Citing that data, the lawsuits noted that error rates for the insurers’ psychiatrist listings were between 26% and 83% in 2018 and 2019. The insurers denied the accusations and convinced a judge to dismiss the suits on technical grounds. A panel of California appeals court judges recently reversed those decisions; the cases are pending.
The companies have continued to send that data to the DMHC each year — but the state has not used it to examine ghost networks. California is among the states that typically waits for a complaint to be filed before it investigates errors.
“The industry doesn’t take the regulatory penalties seriously because they’re so low,” Elliott told ProPublica. “It’s probably worth it to take the risk and see if they get caught.”
California’s limited enforcement has resulted in limited fines. Over the past eight years, the DMHC has issued just $82,500 in fines for directory errors involving providers of any kind. That’s less than one-fifth of the fines issued in the two years before the regulation went into effect.
A spokesperson for the DMHC said its regulators continue “to hold health plans accountable” for violating ghost network regulations. Since 2018, the DMHC has discovered scores of problems with provider directories and pushed health plans to correct the errors. The spokesperson said that the department’s oversight has also helped some customers get reimbursed for out-of-network costs incurred due to directory errors.
“A lower fine total does not equate to a scaling back on enforcement,” the spokesperson said.
Dr. Joaquin Arambula, one of the state Assembly members who co-sponsored AB 236, disagreed. He told ProPublica that California’s current ghost network regulation is “not effectively being enforced.” After clearing the state Assembly this past winter, his bill, along with several others that address mental health issues, was suddenly tabled this summer. The roadblock came from a surprising source: the administration of the state’s Democratic governor.
Officials with the DMHC, whose director was appointed by Gov. Gavin Newsom, estimated that more than $15 million in extra funding would be needed to carry out the bill’s requirements over the next five years. State lawmakers accused officials of inflating the costs. The DMHC’s spokesperson said that the estimate was accurate and based on the department’s “real experience” overseeing health plans.
Arambula and his co-sponsors hope that their colleagues will reconsider the measure during next year’s session. Sitting before state lawmakers in Sacramento this year, a therapist named Sarah Soroken told the story of a patient who had called 50 mental health providers in her insurer’s directory. None of them could see her. Only after the patient attempted suicide did she get the care she’d sought.
“We would be negligent,” Soroken told the lawmakers, “if we didn’t do everything in our power to ensure patients get the health care they need.”
Paige Pfleger of WPLN/Nashville Public Radio contributed reporting.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bird flu has been detected in a pig in the US. Why does that matter?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States Department of Agriculture last week reported that a pig on a backyard farm in Oregon was infected with bird flu.
As the bird flu situation has evolved, we’ve heard about the A/H5N1 strain of the virus infecting a range of animals, including a variety of birds, wild animals and dairy cattle.
Fortunately, we haven’t seen any sustained spread between humans at this stage. But the detection of the virus in a pig marks a worrying development in the trajectory of this virus.
David MG/Shutterstock How did we get here?
The most concerning type of bird flu currently circulating is clade 2.3.4.4b of A/H5N1, a strain of influenza A.
Since 2020, A/H5N1 2.3.4.4b has spread to a vast range of birds, wild animals and farm animals that have never been infected with bird flu before.
While Europe is a hotspot for A/H5N1, attention is currently focused on the US. Dairy cattle were infected for the first time in 2024, with more than 400 herds affected across at least 14 US states.
Bird flu has enormous impacts on farming and commercial food production, because infected poultry flocks have to be culled, and infected cows can result in contaminated diary products. That said, pasteurisation should make milk safe to drink.
While farmers have suffered major losses due to H5N1 bird flu, it also has the potential to mutate to cause a human pandemic.
Birds and humans have different types of receptors in their respiratory tract that flu viruses attach to, like a lock (receptors) and key (virus). The attachment of the virus allows it to invade a cell and the body and cause illness. Avian flu viruses are adapted to birds, and spread easily among birds, but not in humans.
So far, human cases have mainly occurred in people who have been in close contact with infected farm animals or birds. In the US, most have been farm workers.
The concern is that the virus will mutate and adapt to humans. One of the key steps for this to happen would be a shift in the virus’ affinity from the bird receptors to those found in the human respiratory tract. In other words, if the virus’ “key” mutated to better fit with the human “lock”.
A recent study of a sample of A/H5N1 2.3.4.4b from an infected human had worrying findings, identifying mutations in the virus with the potential to increase transmission between human hosts.
Why are pigs a problem?
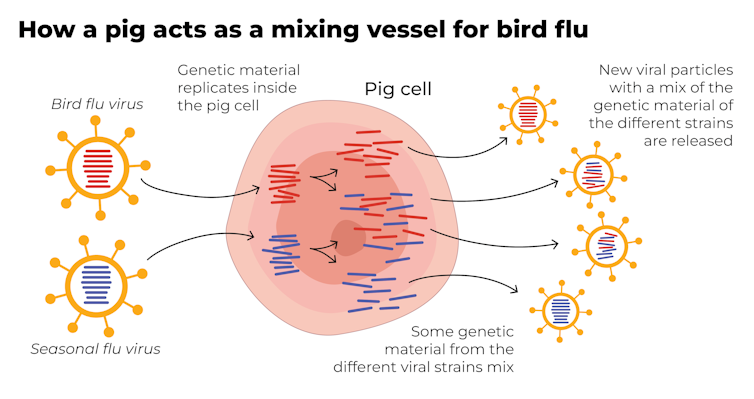
A human pandemic strain of influenza can arise in several ways. One involves close contact between humans and animals infected with their own specific flu viruses, creating opportunities for genetic mixing between avian and human viruses.
Pigs are the ideal genetic mixing vessel to generate a human pandemic influenza strain, because they have receptors in their respiratory tracts which both avian and human flu viruses can bind to.
This means pigs can be infected with a bird flu virus and a human flu virus at the same time. These viruses can exchange genetic material to mutate and become easily transmissible in humans.
The Conversation, CC BY-SA Interestingly, in the past pigs were less susceptible to A/H5N1 viruses. However, the virus has recently mutated to infect pigs more readily.
In the recent case in Oregon, A/H5N1 was detected in a pig on a non-commercial farm after an outbreak occurred among the poultry housed on the same farm. This strain of A/H5N1 was from wild birds, not the one that is widespread in US dairy cows.
The infection of a pig is a warning. If the virus enters commercial piggeries, it would create a far greater level of risk of a pandemic, especially as the US goes into winter, when human seasonal flu starts to rise.
How can we mitigate the risk?
Surveillance is key to early detection of a possible pandemic. This includes comprehensive testing and reporting of infections in birds and animals, alongside financial compensation and support measures for farmers to encourage timely reporting.
Strengthening global influenza surveillance is crucial, as unusual spikes in pneumonia and severe respiratory illnesses could signal a human pandemic. Our EPIWATCH system looks for early warnings of such activity, which can speed up vaccine development.
If a cluster of human cases occurs, and influenza A is detected, further testing (called subtyping) is essential to ascertain whether it’s a seasonal strain, an avian strain from a spillover event, or a novel pandemic strain.
Early identification can prevent a pandemic. Any delay in identifying an emerging pandemic strain enables the virus to spread widely across international borders.
Australia’s first human case of A/H5N1 occurred in a child who acquired the infection while travelling in India, and was hospitalised with illness in March 2024. At the time, testing revealed Influenza A (which could be seasonal flu or avian flu), but subtyping to identify A/H5N1 was delayed.
This kind of delay can be costly if a human-transmissible A/H5N1 arises and is assumed to be seasonal flu because the test is positive for influenza A. Only about 5% of tests positive for influenza A are subtyped further in Australia and most countries.
In light of the current situation, there should be a low threshold for subtyping influenza A strains in humans. Rapid tests which can distinguish between seasonal and H5 influenza A are emerging, and should form part of governments’ pandemic preparedness.
A higher risk than ever before
The US Centers for Disease Control and Prevention states that the current risk posed by H5N1 to the general public remains low.
But with H5N1 now able to infect pigs, and showing worrying mutations for human adaptation, the level of risk has increased. Given the virus is so widespread in animals and birds, the statistical probability of a pandemic arising is higher than ever before.
The good news is, we are better prepared for an influenza pandemic than other pandemics, because vaccines can be made in the same way as seasonal flu vaccines. As soon as the genome of a pandemic influenza virus is known, the vaccines can be updated to match it.
Partially matched vaccines are already available, and some countries such as Finland are vaccinating high-risk farm workers.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney and Haley Stone, Research Associate, Biosecurity Program, Kirby Institute & CRUISE lab, Computer Science and Engineering, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: