How the HHS impacts your community’s health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. Department of Health and Human Services is responsible for programs that impact every community in the country. But most Americans aren’t aware of the department’s scope.
“Most of the power in the agency, most of the administrative authority comes from laws that Congress has passed,” former HHS Secretary Kathleen Sebelius told NPR. She added that the HHS secretary “could redefine terms that had a huge impact on people. And that could be done all administratively, not by going back to Congress.”
HHS is comprised of 13 agencies, all of which play an important role in promoting the health of all Americans. These are just some of the ways that HHS affects people’s lives and health.
Vaccines
One of HHS’s most salient roles is developing, approving, and monitoring vaccines after they are on the market. The National Institutes of Health funds and conducts research to develop new vaccines and improve existing ones. The NIH’s Vaccine Research Center spearheads research to develop vaccines against deadly diseases like HIV/AIDS, malaria, and tuberculosis.
The Food and Drug Administration is responsible for overseeing clinical trials that test product safety and effectiveness, approving new vaccines, and monitoring the safety of all vaccines before and after approval. In conjunction with the Centers for Disease Control and Prevention, the FDA also manages the national surveillance systems that record and flag potential vaccine side effects.
In addition to safety monitoring, the CDC conducts research on vaccine safety and effectiveness and issues vaccination guidance. The agency’s recommended immunization schedule guides school and child care vaccination requirements and health care provider recommendations nationwide.
Although the CDC does not have the authority over school and childcare vaccination requirements at the state level, changes to the agency’s recommendations could have wide-ranging impacts.
“If this recommendation changes, there’s downstream effects, like insurance companies could stop covering them. And adding cost could easily deter uptake,” epidemiologist and creator of the Your Local Epidemiologist newsletter Katelyn Jetelina told PBS.
However, CDC vaccine recommendations are just that: recommendations. The agency cannot dictate, for example, vaccine requirements for school enrollment. Those standards are set at the state level, with the possible exception during a national public health emergency.
Drug safety
The FDA oversees all clinical trials in the United States. Every prescription drug and many medical products undergo a rigorous, closely regulated, multistep trial to test their safety and effectiveness. At the end of that process, the FDA determines whether a drug meets its standards for approval. Without FDA approval, a drug cannot be sold in the U.S.
Like with vaccines, the FDA monitors potential safety concerns related to over-the-counter and prescription medications, medical devices, and other products the agency regulates. Health care providers, FDA-regulated companies, and patients can report suspected safety issues to the agency, which evaluates each report for further investigation.
The FDA also alerts the public to safety concerns related to medical products by releasing safety notices, adding warning labels, and issuing drug recalls.
Pandemic and public health emergency response
Several HHS agencies are tasked with preventing, preparing for, and responding to disease outbreaks. This responsibility includes tracking potentially dangerous infectious diseases in the U.S. and globally, developing pandemic response strategies, and issuing guidance to contain ongoing outbreaks.
Both the CDC and FDA inform the public about public health concerns, including pandemics. The Administration for Strategic Preparedness and Response works with communities, medical facilities, local and state governments, and industry partners to enhance responses to disasters and public health emergencies.
The CDC also tracks pathogens like the flu, norovirus, and sexually transmitted infections to better understand where diseases are spreading, how they are evolving, and how best to prepare for outbreaks.
In the event of a public health emergency, the CDC may issue guidance on how to stay safe and minimize health impacts. For example, in January, the agency released tips on how to protect against smoke during the wildfires affecting southern California and how to avoid frostbite and hypothermia, as extreme cold weather affected much of the country.
The FDA can issue emergency use authorizations, which allow the use of “unapproved medical products or unapproved uses of approved medical products … to diagnose, treat, or prevent serious or life-threatening diseases … when certain criteria are met” during public health emergencies. These authorizations help ensure that the standard FDA approval process is not a barrier to the public receiving lifesaving medical products, such as authorizing specific vaccines during a pandemic.
Food and water safety
The FDA, along with the U.S. Department of Agriculture, plays an important role in regulating food safety. The agency approves and monitors the safety of food additives, like sweeteners, dyes, and preservatives. It also regulates how food is prepared, packaged, and stored, including conducting inspections of food facilities and farms.
FDA food safety testing detects dangerous foodborne illnesses like salmonella and E. coli. For example, in late December 2024, the FDA began testing raw (unpasteurized) milk products for bird flu contamination. The CDC investigates outbreaks of foodborne illnesses and, along with the FDA and USDA, provides the public with information about food safety.
The FDA also regulates most food labels, including nutrition facts, ingredient lists, and health claims on food packaging. In January, the agency proposed new front-of-package nutrition labels that highlight sugar, fat, and sodium content in packaged food products.
HHS and the USDA are responsible for updating the Dietary Guidelines for Americans, which are updated every five years. These guidelines are the basis of all federal food assistance programs for children, older adults, and low-income families.
HHS sets the guidelines for the maximum fluoride level in drinking water and periodically makes recommendations about fluoride levels. However, the department has no authority to require or ban fluoridation, which is regulated at the state and local level. U.S. cities began adding fluoride to drinking water in the 1940s to improve dental health and reduce cavities by 25 percent.
Health care access
The HHS secretary regulates the Centers for Medicare & Medicaid Services, which provides health insurance to adults 65 and older, people with disabilities, low-income families, and eligible children through the Children’s Health Insurance Program. Together, Medicare, Medicaid, and CHIP insure over 145 million Americans, or roughly 42 percent of the U.S. population. Changes to either of these programs could impact health care access and quality for millions of Americans.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When A Period Is Very Late (Post-Menopause)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Knowledge Is
PowerSafety, Post-Menopause TooNote: this article will be most relevant for a subset of our subscribership, but it’s a very large subset, so we’re going to go ahead and address the reader as “you”.
If, for example, you are a man and this doesn’t apply to you, we hope it will interest you anyway (we imagine there are women in your life).
PS: the appendicitis check near the end, works for anyone with an appendix
We’ve talked before about things that come with (and continue after) menopause:
- What You Should Have Been Told About The Menopause Beforehand
- What Menopause Does To The Heart
- Alzheimer’s Sex Differences May Not Be What They Appear
But what’s going on if certain menstrual symptoms reappear post-menopause (e.g. after more than a year with no menstruation)?
Bleeding
You should not, of course, be experiencing vaginal bleeding post-menopause. You may have seen “PSA” style posts floating around social media warning that this is a sign of cancer. And, it can be!
But it’s probably not.
Endometrial cancer (the kind that causes such bleeding) affects 2–3% of women, and of those reporting post-menopausal bleeding, the cause is endometrial cancer only 9% of those times.
So in other words, it’s not to be ignored, but for 9 people out of 10 it won’t be cancer:
Read more: Harvard Health | Postmenopausal bleeding: Don’t worry—but do call your doctor
Other more likely causes are uterine fibroids or polyps. These are unpleasant but benign, and can be corrected with surgery if necessary.
The most common cause, however is endometrial and/or vaginal atrophy resulting in tears and bleeding.
Tip: Menopausal HRT will often correct this.
Read more: The significance of “atrophic endometrium” in women with postmenopausal bleeding
(“atrophic endometrium” and “endometrial atrophy” are the same thing)
In summary: no need to panic, but do get it checked out at your earliest convenience. This is not one where we should go “oh that’s weird” and ignore.
Cramps
If you are on menopausal HRT, there is a good chance that these are just period cramps. They may feel different than they did before, because you didn’t ovulate and thus you’re not shedding a uterine lining now, but your body is going to do its best to follow the instructions given by the hormones anyway (hormones are just chemical messengers, after all).
If it is just this, then they will probably settle down to a monthly cycle and become quite predictable.
Tip: if it’s the above, then normal advice for period cramps will go here. We recommend ginger! It’s been found to be as effective as Novafen (a combination drug of acetaminophen (Tylenol), caffeine, and ibuprofen), in the task of relieving menstrual pain:
See: Effect of Ginger and Novafen on menstrual pain: A cross-over trial
It could also be endometriosis. Normally this affects those of childbearing age, but once again, exogenous hormones (as in menopausal HRT) can fool the body into doing it.
If you are not on menopausal HRT (or sometimes even if you are), uterine fibroids (as discussed previously) are once again a fair candidate, and endometriosis is also still possible, though less likely.
Special last note
Important self-check: if you are experiencing a sharp pain in that general area and are worrying if it is appendicitis (also a possibility), then pressing on the appropriately named McBurney’s point is a first-line test for appendicitis. If, after pressing, it hurts a lot more upon removal of pressure (rather than upon application of pressure), this is considered a likely sign of appendicitis. Get thee to a hospital, quickly.
And if it doesn’t? Still get it checked out at your earliest convenience, of course (better safe than sorry), but you might make an appointment instead of calling an ambulance.
Take care!
Share This Post
-
I Will Make You Passionate About Exercise – by Bevan Eyles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What this isn’t: a “just do it!” motivational pep-talk.
What this is:a compassionate and thoughtful approach to help non-exercisers become regular exercisers, by looking at the real life factors of what holds people back (learning from his own early failures as a coach, by paying attention now to things he inadvertently neglected back then), both in the material/practical and in the psychological/emotional.
Further, he gives a 10-step method, for those who would like to be walked through it by the hand, making the transition to exercising regularly (and as a leisure habit, rather than as a chore) as frictionless as possible.
The style is friendly and energetic, and very easy-reading throughout.
Bottom line: if you are someone who finds exercising to be a chore, this book can definitely help you “get from here to there” in terms of finding joy in it, and finding exercise even easier than not exercising. Yes, really.
Share This Post
-
GABA Against Stress/Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Neurotransmitter Less Talked-About
GABA is taken by many people as a supplement, mostly as a mood modifier, though its health claims go beyond the recreational—and also, we’re of the opinion that mental health is also just health, and if it works, it works. We’ll explore some of the claims and science behind them today…
What is GABA?
GABA stands for gamma-aminobutyric acid, and it’s a neurotransmitter. It’s a lot less talked-about than for example dopamine or serotonin, but it’s very important nonetheless.
We make it ourselves inside our body, and we can also get it from our food, or supplement it, and some drugs will also have an effect on its presence and/or activity in our body.
What foods is it found in?
- Animals, obviously (just like in human brains*)
- Fermented foods (many kinds)
- Yeast
- Tea
- Tomatoes
- Mulberries
For more details, see:
γ-Aminobutyric acid found in fermented foods and beverages: current trends
*However, we do not recommend eating human brains, due to the risk of CJD and prion diseases in general.
What claims are made about it and are they true?
For brevity, we’ll give a little spoiler up-front: all the popular claims for it appear to be valid, though there’s definitely room for a lot more human trials (we skipped over a lot of rodent studies today!).
So we’ll just drop some of its main benefits, and human studies to back those.
Reduction of stress and anxiety
GABA decreases task-related stress and anxiety within 30 minutes of being taken, both in subjective measures (i.e., self-reports) and in objective clinical physiological measures:
Cognitive enhancement
It’s not a does-everything nootropic like some, but it does have clear benefits to episodic memory:
❝GABA intake might help to distribute limited attentional resources more efficiently, and can specifically improve the identification and ordering of visual events that occur in close temporal succession❞
One of the things that makes this one important is that it also deals with the often-asked question of “does GABA pass the blood-brain barrier”:
❝The present findings do give further credence to the idea that oral ingestion does allow GABA to reach the brain and exert direct effects on cognition, which in the present case were specific to temporal attention.❞
Read more:
Supplementation of gamma-aminobutyric acid (GABA) affects temporal, but not spatial visual attention
Potential for more
We take care to give good quality sources, so the following study comes with a big caveat that it has since been retracted. Why was it retracted, you wonder?
It’s about the sample; they cite “30 healthy adults”, but neglected tp mention that this figure was initially 46. What happened to the other 16 participants is unclear, but given that this was challenged and the challenge not answered, it was sufficient for the journal (Nature) to pull the study, in case of deliberate sample bias.
However! Running the numbers in their results section, a probability of 0.03 is very compelling unless the disappearance of 16 subjects was outright fraudulent (which we regrettably cannot know either way).
Here’s the study (so take it with a pinch of salt, considering the above), and taken at face value, it shows how GABA supplementation improves accurate reactions to fast-moving visual and auditory stimuli:
RETRACTED ARTICLE: γ-Aminobutyric acid (GABA) administration improves action selection processes: a randomised controlled trial
…so, hopefully this experiment will be repeated, without disappearing participants!
The sweet spot
You may be wondering how something that slows a person down (having a relaxing effect) can also speed a person up. This has to do with what it is and isn’t affecting; think of it like a “focus mode” on your computer or other device that greys-out everything else a bit so that you can focus on what you’re doing.
It’s in some ways (by different neurochemical pathways, though) a similar effect to the “relaxed alertness” created by l-theanine supplementation.
There’s also a sweet spot whereby GABA is toning some things down just the right amount, without adversely affecting performance in areas we don’t want slowed down. For the science of this, see:
Is it safe?
GABA is “Generally Recognized As Safe”. However:
- you should speak with your pharmacist if you are taking any medications for blood pressure or epilepsy, as GABA supplementation may cause them to work too well.
- you should absolutely not take GABA with alcohol or opioids as (dose-dependent for all the substances involved, and also depending on your metabolic base rate and other factors) its acute depression of the CNS can mean you relax and slow down too much, and you may find yourself not breathing often enough to sustain life.
Aside from that, it is considered safe up to at least 1g/kg/day*. Given that popular doses are 120–750mg, and most people weigh more than 750g, this is very safe for most people:
United States Pharmacopeia (USP) Safety Review of Gamma-Aminobutyric Acid (GABA)
Where can I get it?
We don’t sell it, but for your convenience, here’s an example product on Amazon
Enjoy!
Share This Post
Related Posts
-
Why do I keep getting urinary tract infections? And why are chronic UTIs so hard to treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing with chronic urinary tract infections (UTIs) means facing more than the occasional discomfort. It’s like being on a never ending battlefield against an unseen adversary, making simple daily activities a trial.
UTIs happen when bacteria sneak into the urinary system, causing pain and frequent trips to the bathroom.
Chronic UTIs take this to the next level, coming back repeatedly or never fully going away despite treatment. Chronic UTIs are typically diagnosed when a person experiences two or more infections within six months or three or more within a year.
They can happen to anyone, but some are more prone due to their body’s makeup or habits. Women are more likely to get UTIs than men, due to their shorter urethra and hormonal changes during menopause that can decrease the protective lining of the urinary tract. Sexually active people are also at greater risk, as bacteria can be transferred around the area.
Up to 60% of women will have at least one UTI in their lifetime. While effective treatments exist, about 25% of women face recurrent infections within six months. Around 20–30% of UTIs don’t respond to standard antibiotic. The challenge of chronic UTIs lies in bacteria’s ability to shield themselves against treatments.
Why are chronic UTIs so hard to treat?
Once thought of as straightforward infections cured by antibiotics, we now know chronic UTIs are complex. The cunning nature of the bacteria responsible for the condition allows them to hide in bladder walls, out of antibiotics’ reach.
The bacteria form biofilms, a kind of protective barrier that makes them nearly impervious to standard antibiotic treatments.
This ability to evade treatment has led to a troubling increase in antibiotic resistance, a global health concern that renders some of the conventional treatments ineffective.
Some antibiotics no longer work against UTIs.
Michael Ebardt/ShutterstockAntibiotics need to be advanced to keep up with evolving bacteria, in a similar way to the flu vaccine, which is updated annually to combat the latest strains of the flu virus. If we used the same flu vaccine year after year, its effectiveness would wane, just as overused antibiotics lose their power against bacteria that have adapted.
But fighting bacteria that resist antibiotics is much tougher than updating the flu vaccine. Bacteria change in ways that are harder to predict, making it more challenging to create new, effective antibiotics. It’s like a never-ending game where the bacteria are always one step ahead.
Treating chronic UTIs still relies heavily on antibiotics, but doctors are getting crafty, changing up medications or prescribing low doses over a longer time to outwit the bacteria.
Doctors are also placing a greater emphasis on thorough diagnostics to accurately identify chronic UTIs from the outset. By asking detailed questions about the duration and frequency of symptoms, health-care providers can better distinguish between isolated UTI episodes and chronic conditions.
The approach to initial treatment can significantly influence the likelihood of a UTI becoming chronic. Early, targeted therapy, based on the specific bacteria causing the infection and its antibiotic sensitivity, may reduce the risk of recurrence.
For post-menopausal women, estrogen therapy has shown promise in reducing the risk of recurrent UTIs. After menopause, the decrease in estrogen levels can lead to changes in the urinary tract that makes it more susceptible to infections. This treatment restores the balance of the vaginal and urinary tract environments, making it less likely for UTIs to occur.
Lifestyle changes, such as drinking more water and practising good hygiene like washing hands with soap after going to the toilet and the recommended front-to-back wiping for women, also play a big role.
Some swear by cranberry juice or supplements, though researchers are still figuring out how effective these remedies truly are.
What treatments might we see in the future?
Scientists are currently working on new treatments for chronic UTIs. One promising avenue is the development of vaccines aimed at preventing UTIs altogether, much like flu shots prepare our immune system to fend off the flu.
Emerging treatments could help clear chronic UTIs.
guys_who_shoot/ShutterstockAnother new method being looked at is called phage therapy. It uses special viruses called bacteriophages that go after and kill only the bad bacteria causing UTIs, while leaving the good bacteria in our body alone. This way, it doesn’t make the bacteria resistant to treatment, which is a big plus.
Researchers are also exploring the potential of probiotics. Probiotics introduce beneficial bacteria into the urinary tract to out-compete harmful pathogens. These good bacteria work by occupying space and resources in the urinary tract, making it harder for harmful pathogens to establish themselves.
Probiotics can also produce substances that inhibit the growth of harmful bacteria and enhance the body’s immune response.
Chronic UTIs represent a stubborn challenge, but with a mix of current treatments and promising research, we’re getting closer to a day when chronic UTIs are a thing of the past.
Iris Lim, Assistant Professor, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Some women’s breasts can’t make enough milk, and the effects can be devastating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many new mothers worry about their milk supply. For some, support from a breastfeeding counsellor or lactation consultant helps.
Others cannot make enough milk no matter how hard they try. These are women whose breasts are not physically capable of producing enough milk.
Our recently published research gives us clues about breast features that might make it difficult for some women to produce enough milk. Another of our studies shows the devastating consequences for women who dream of breastfeeding but find they cannot.
Some breasts just don’t develop
Unlike other organs, breasts are not fully developed at birth. There are key developmental stages as an embryo, then again during puberty and pregnancy.
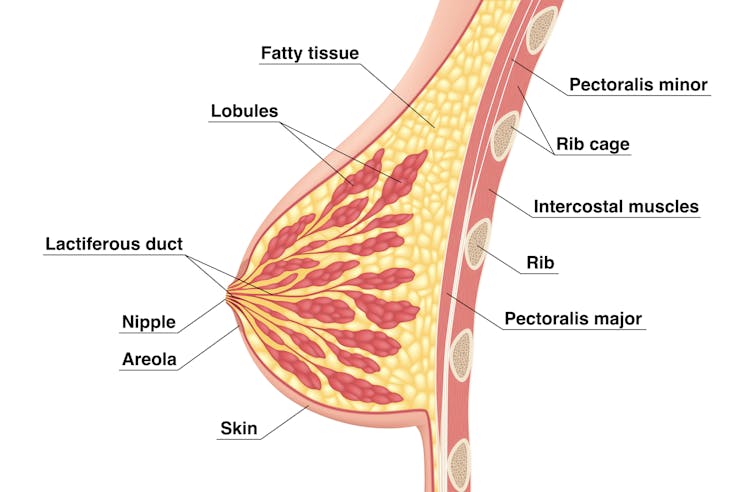
At birth, the breast consists of a simple network of ducts. Usually during puberty, the glandular (milk-making) tissue part of the breast begins to develop and the ductal network expands. Then typically, further growth of the ductal network and glandular tissue during pregnancy prepares the breast for lactation.
But our online survey of women who report low milk supply gives us clues to anomalies in how some women’s breasts develop.
We’re not talking about women with small breasts, but women whose glandular tissue (shown in this diagram as “lobules”) is underdeveloped and have a condition called breast hypoplasia.
Sometimes not enough glandular tissue, shown here as lobules, develop.
Tsuyna/ShutterstockWe don’t know how common this is. But it has been linked with lower rates of exclusive breastfeeding.
We also don’t know what causes it, with much of the research conducted in animals and not humans.
However, certain health conditions have been associated with it, including polycystic ovary syndrome and other endocrine (hormonal) conditions. A high body-mass index around the time of puberty may be another indicator.
Could I have breast hypoplasia?
Our survey and other research give clues about who may have breast hypoplasia.
But it’s important to note these characteristics are indicators and do not mean women exhibiting them will definitely be unable to exclusively breastfeed.
Indicators include:
- a wider than usual gap between the breasts
- tubular-shaped (rather than round) breasts
- asymmetric breasts (where the breasts are different sizes or shapes)
- lack of breast growth in pregnancy
- a delay in or absence of breast fullness in the days after giving birth
In our survey, 72% of women with low milk supply had breasts that did not change appearance during pregnancy, and about 70% reported at least one irregular-shaped breast.
The effects
Mothers with low milk supply – whether or not they have breast hyoplasia or some other condition that limits their ability to produce enough milk – report a range of emotions.
Research, including our own, shows this ranges from frustration, confusion and surprise to intense or profound feelings of failure, guilt, grief and despair.
Some mothers describe “breastfeeding grief” – a prolonged sense of loss or failure, due to being unable to connect with and nourish their baby through breastfeeding in the way they had hoped.
These feelings of failure, guilt, grief and despair can trigger symptoms of anxiety and depression for some women.
Feelings of failure, guilt, grief and despair were common.
Bricolage/ShutterstockOne woman told us:
[I became] so angry and upset with my body for not being able to produce enough milk.
Many women’s emotions intensified when they discovered that despite all their hard work, they were still unable to breastfeed their babies as planned. A few women described reaching their “breaking point”, and their experience felt “like death”, “the worst day of [my] life” or “hell”.
One participant told us:
I finally learned that ‘all women make enough milk’ was a lie. No amount of education or determination would make my breasts work. I felt deceived and let down by all my medical providers. How dare they have no answers for me when I desperately just wanted to feed my child naturally.
Others told us how they learned to accept their situation. Some women said they were relieved their infant was “finally satisfied” when they began supplementing with formula. One resolved to:
prioritise time with [my] baby over pumping for such little amounts.
Where to go for help
If you are struggling with low milk supply, it can help to see a lactation consultant for support and to determine the possible cause.
This will involve helping you try different strategies, such as optimising positioning and attachment during breastfeeding, or breastfeeding/expressing more frequently. You may need to consider taking a medication, such as domperidone, to see if your supply increases.
If these strategies do not help, there may be an underlying reason why you can’t make enough milk, such as insufficient glandular tissue (a confirmed inability to make a full supply due to breast hypoplasia).
Even if you have breast hypoplasia, you can still breastfeed by giving your baby extra milk (donor milk or formula) via a bottle or using a supplementer (which involves delivering milk at the breast via a tube linked to a bottle).
More resources
The following websites offer further information and support:
- Australian Breastfeeding Association
- Lactation Consultants of Australia and New Zealand
- Royal Women’s Hospital, Melbourne
- Supply Line Breastfeeders Support Group of Australia Facebook support group
- IGT And Low Milk Supply Support Group Facebook support group
- Breastfeeding Medicine Network Australia/New Zealand
- Supporting breastfeeding grief (a collection of resources).
Shannon Bennetts, a research fellow at La Trobe University, contributed to this article.
Renee Kam, PhD candidate and research officer, La Trobe University and Lisa Amir, Professor in Breastfeeding Research, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs Of Iodine Deficiency You Might Not Expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Coach Kait (BSc Nutrition & Exercise) is a certified health and nutrition coach, and today she’s here to talk about iodine—which is important for many of our body functions, from thyroid hormone production to metabolic regulation to heart rate management, as well as more superficial-but-important-too things like our skin and hair.
Kait’s hitlist
Here’s what she recommends we look out for:
- Swollen neck: even a slightly swollen neck might indicate low iodine levels (this is because that’s where the thyroid glands are)
- Hair loss: iodine is needed for healthy hair growth, so a deficiency can lead to hair loss / thinning hair
- Dry and flaky skin: with iodine’s role in our homeostatic system not being covered, our skin can dry out as a result
- Feeling cold all the time: because of iodine’s temperature-regulating activities
- Slow heart rate: A metabolic slump due to iodine deficiency can slow down the heart rate, leading to fatigue and weakness (and worse, if it persists)
- Brain fog: trouble focusing can be a symptom of the same metabolic slump
- Fatigue: this is again more or less the same thing, but she said eight signs, so we’re giving you the eight!
- Irregular period (if you normally have such, of course): because iodine affects reproductive hormones too, an imbalance can disrupt menstrual cycles.
For more on each of these, as well as how to get more iodine in your diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might also like to read:
- A Fresh Take On Hypothyroidism
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: