Your Heart In Their Hands: Surgeon Preferences & Survival Rates
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unless you are paying entirely out-of-pocket for a heart surgery, you will not usually get final say over which surgeon you get.
The surgeon, however, will have final say over what they actually do when they open you up.
And their preferences, it seems, can make all the difference:
MAG vs SAG
When doing coronary artery bypass grafting, (CABG), surgeons may prefer to do multi-arterial grafting (MAG) or single-arterial grafting (SAG).
Recently, there was a study analysing more than a million Americans who underwent CABG on Medicare over an 18-year period, looking at outcomes for MAG vs SAG.
The superficial news: those who received MAG had much better long-term survival chances than those who received SAG.
However: this may be less to do with the relative merits of the procedures themselves, and more to do with the preferences of the surgeon.
The “eyeball test”
If surgeons look at a patient and think they will not have many years to live after surgery, they may opt for the SAG, as the long-term benefits of the MAG will only manifest in the long-term.
This may seem a little self-defeating (indeed, maybe you won’t live to see the long-term if you don’t get the surgery type with the longer-term survival chances), there can be other factors involved, that may make surgeons more interested in your short-term survival chances.
Or you might just not have enough donor artery tissue available to pick and choose; after all, a person having a coronary artery bypass quite possibly won’t have great arteries in their arm or leg, either.
Or a person could be missing limbs (a common complication, given the comorbidities of both peripheral artery disease, and diabetes).
See also: How To Stay A Step Ahead Of Peripheral Artery Disease
Why it might be ok that things are like this
When factoring in surgeon preference for MAG or SAG as an instrumental variable, no significant difference in long-term survival was observed. This may explain inconsistencies with randomized controlled trials like the Arterial Revascularization Trial (ART), which also found no survival benefit of MAG over SAG.
Also, MAG recipients were generally younger, healthier, and from more resourceful areas, which likely had a further impact on MAG-giving decisions, and/but at the same time, may also have increased survival chances for reasons other than that they got MAG rather than SAG.
Here’s a pop-science article that goes into more detail about this:
Surgeon preferences may explain differences in CABG survival rates
How to look out for yourself, and advocate for yourself
…or your loved one, of course. Now, having a coronary artery bypass surgery of any kind is not a fun activity; it will be dangerous, it’ll be stressful before and after, and the recovery will often not be an easy time either. However, it is possible to learn more about what is going on / what will happen, ask the right questions, and get the best options for you (which may not always be the same as the best options for someone else).
We wrote about that in more detail here:
Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Jumping Rope Changes The Human Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most popularly enjoyed by professional boxers and six-year-old girls, jumping rope is one of the most metabolism-boosting exercises around:
Just a hop, skip, and a jump away from good health
Maybe you haven’t tried it since your age was in single digits, so, if you do…
What benefits can you expect?
- Improves cardiovascular fitness, equivalent to 30 minutes of running with just 10 minutes of jumping.
- Increases bone density and boosts immunity by aiding the lymphatic system.
- Enhances explosiveness in the lower body, agility, and stamina.
- Improves shoulder endurance, coordination, and spatial awareness.
What kind of rope is best for you?
- Beginner ropes: licorice ropes (nylon/vinyl), beaded ropes for rhythm and durability.
- Advanced ropes: speed ropes (denser, faster materials) for higher speeds and more difficult skills.
- Weighted ropes: build upper body muscles (forearms, shoulders, chest, back).
What length should you get?
- Recommended rope length varies by height (8 ft for 5’0″–5’4″, 9 ft for 5’5″–5’11”, 10 ft for 6’0″ and above).
- Beginners should start with longer ropes for clearance.
What should you learn?
- Initial jump rope skills: start with manageable daily jump totals, gradually increasing as ankles, calves, and feet adapt.
- Further skills: learn the two-foot jump and then the boxer’s skip for efficient, longer sessions and advanced skills. Keep arms close and hands at waist level for a smooth swing.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Do High Intensity Interval Training (Without Wrecking Your Body)
Take care!
Share This Post
-
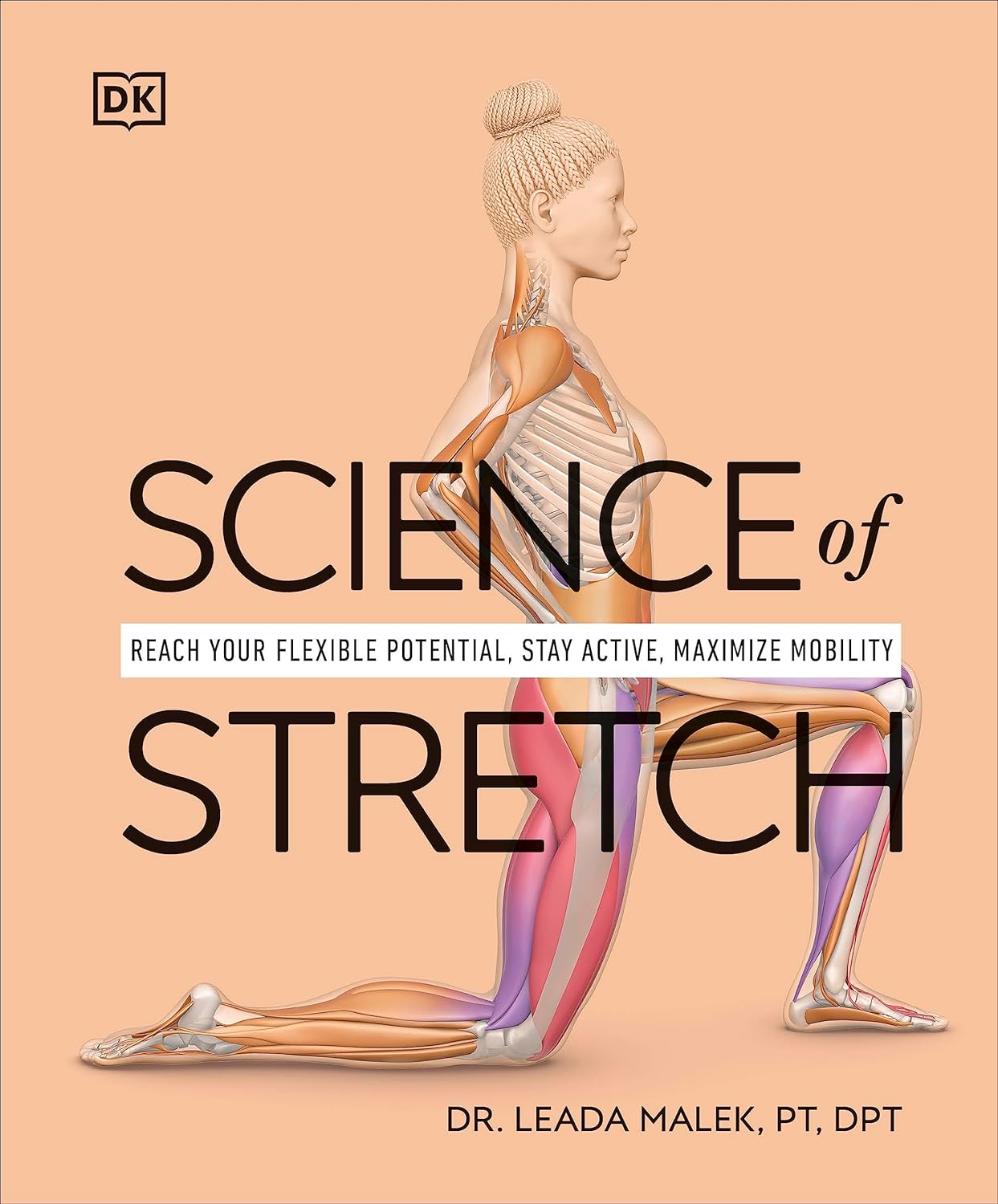
Science of Stretch – by Dr. Leada Malek
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is part of a “Science of…” series, of which we’ve reviewed some others before (Yoga | HIIT | Pilates), and needless to say, we like them.
You may be wondering: is this just that thing where a brand releases the same content under multiple names to get more sales, and no, it’s not (long-time 10almonds readers will know: if it were, we’d say so!).
While flexibility and mobility are indeed key benefits in yoga and Pilates, they looked into the science of what was going on in yoga asanas and Pilates exercises, stretchy or otherwise, so the stretching element was not nearly so deep as in this book.
In this one, Dr. Malek takes us on a wonderful tour of (relevant) human anatomy and physiology, far deeper than most pop-science books go into when it comes to stretching, so that the reader can really understand every aspect of what’s going on in there.
This is important, because it means busting a lot of myths (instead of busting tendons and ligaments and things), understanding why certain things work and (critically!) why certain things don’t, how certain stretching practices will sabotage our progress, things like that.
It’s also beautifully clearly illustrated! The cover art is a fair representation of the illustrations inside.
Bottom line: if you want to get serious about stretching, this is a top-tier book and you won’t regret it.
Click here to check out Science of Stretching, and learn what you can do and how!
Share This Post
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
Related Posts
-
Staying Healthy and Active After 60
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: How to be your best self after 60: Self motivation / Avoiding or limiting salt, sugar & alcohol: Alternatives / Ways to sneak in more movements/exercise
…and, from a different subscriber…
Q: Inflammation & over 60 weight loss. Thanks!
Here are some of our greatest hits on those topics:
- Where Nutrition Meets Habits ← focusing on food that’s all three of: healthy + easy + cheap
- How To Keep On Keeping On ← exercise tips for when the motivation wanes
- Keep Inflammation At Bay ← science-based tips and advice
Also, while we’ve recommended a couple of books on stopping (or reducing) drinking, we’ve not done a main feature on that, so we definitely will one of these days!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Outsmart Your Pain – by Dr. Christiane Wolf
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Wolf is a physician turned mindfulness teacher. As such, and holding an MD as well as a PhD in psychosomatic medicine, she knows her stuff.
A lot of what she teaches is mindfulness-based stress reduction (MBSR), but this book is much more specific than that. It doesn’t promise you won’t continue to experience pain—in all likelihood you will—but it does change the relationship with pain, and this greatly lessens the suffering and misery that comes with it.
For many, the most distressing thing about pain is not the sensation itself, but how crippling it can be—getting in the way of life, preventing enjoyment of other things, and making every day a constant ongoing exhausting battle… And every night, a “how much rest am I actually going to be able to get, and in what condition will I wake up, and how will I get through tomorrow?” stress-fest.
Dr. Wolf helps the reader to navigate through all these challenges and more; minimize the stress, maximize the moments of respite, and keep pain’s interference with life to a minimum. Each chapter addresses different psychological aspects of chronic pain management, and each comes with specific mindfulness meditations to explore the new ideas learned.
The style is personal and profound, while coming from a place of deep professional understanding as well as compassion.
Bottom line: if you’ve been looking for a life-ring to help you reclaim your life, this one could be it; we wholeheartedly recommend it.
Click here to check out Outsmart Your Pain, and recover the beauty and joy of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Figs vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to banana, we picked the banana.
Why?
Both of these fruits have a reputation for being carb-heavy (though their glycemic index is low in both cases because of the fiber), and they both have approximately the same macros across the board. So a tie on macros.
When it comes to vitamins, figs have more of vitamins A, B1, E, and K, while banana has more of vitamins B2, B3, B5, B6, B9, C, and choline. So, a win for banana there.
In the category of minerals, figs have more calcium and iron, while banana has more copper, magnesium, manganese, phosphorus, potassium, and selenium. Another win for banana.
Adding up the section makes for a win for bananas, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: