The AFib Cure – by Dr. John Day & Dr. Jared Bunch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The authors—cardiologists and AFib specialists—make the case that if you have atrial fibrillation, you do in fact have more options than “take these pills and suffer”.
To be clear: they’re not anti-medication per se and they also acknowledge that for some people the meds may still have their place (safety first, and all), but they do fall on the side of “it would be nice to not have to, if possible, so let’s see what we can do”.
Rather, they recommend lifestyle adjustments (no surprises there), and certain biomarker optimizations (this is where it gets more in-depth), which have a good record of reducing symptoms to the point of remission and freedom from medications.
The book is first a primer on the topic of AFib, and then a how-to manual of fixing the problems that you now understand, by biomarker monitoring, lifestyle optimization, and if those things don’t work, ablative therapy which they argue is safer, easier, and more successful than you might think.
The style is clear and easy to understand, with frequent scholarly citations throughout. On the downside, the tone can sometimes be a little on the pushy side for this reviewer’s tastes, but if one overlooks that, it doesn’t detract from the useful content.
Bottom line: if you or a loved one have AFib and would like more treatment/management options than have hitherto been presented, this book will give you that.
Click here to check out The AFib Cure, and look after your heart!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Soba Noodle Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Japanese dish is packed with nutrients and takes very little preparation time, involving only one cooked ingredient, and a healthy one at that!
You will need
- 8 oz dried soba noodles
- ½ bulb garlic, finely chopped
- 2 tbsp avocado oil
- 2 tsp soy sauce
- ¼ cucumber, cut into thin batons (don’t peel it first)
- ½ carrot, grated (don’t peel it first)
- 6 cherry tomatoes, halved (you wouldn’t peel these, right? Please don’t)
- ½ red onion, finely sliced (ok, this one you can peel first! Please do)
- 1 tbsp chia seeds
- 1 tsp crushed red chili flakes
- Garnish: fresh parsley, chopped
Method
(we suggest you read everything at least once before doing anything)
1) Cook the soba noodles (boil in water for 10 mins or until soft). Rinse with cold water (which lowers the glycemic index further, and also we want them cold anyway) and set aside.
2) Make the dressing by blending the garlic, avocado oil, and soy cauce. Set it aside.
3) Assemble the salad by thoroughly but gently mixing the noodles with the cucumber, carrot, tomatoes, and onion. Add the dressing, the chia seeds, and the chili flakes, and toss gently to combine.
4) Serve, adding the parsley garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Rice vs Buckwheat – Which is Healthier? ← soba noodles are made from buckwheat, which by the way is also a good source of rutin, which can strengthen blood vessel walls against damage, reducing the risk of atheroma
- Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Chia: The Tiniest Seeds With The Most Value
Take care!
Share This Post
-
Maca Root’s Benefits For The Mood And The Ability
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maca Root: What It Does And Doesn’t Do
Maca root, or Lepidium meyenii, gets thought of as a root vegetable, though it’s in fact a cruciferous vegetable and more closely related to cabbage—notwithstanding that it also gets called “Peruvian ginseng”.
- Nutritionally, it’s full of all manner of nutrients (vitamins, minerals, fiber, and a wide array of phytochemicals)
- Medicinally, it’s long enjoyed traditional use against a wide variety of illnesses, including respiratory infections and inflammatory diseases.
It’s also traditionally an aphrodisiac.
Is it really anti-inflammatory?
Probably not… Unless fermented. This hasn’t been studied deeply, but a 2023 study found that non-fermented and fermented maca root extracts had opposite effects in this regard:
However, this was an in vitro study, so we can’t say for sure that the results will carry over to humans.
Is it really an aphrodisiac?
Actually yes, it seems so. Here’s a study in which 45 women with antidepressant-induced sexual dysfunction found it significantly improved both libido and sexual function:
❝In summary, maca root may alleviate antidepressant-induced sexual dysfunction as women age, particularly in the domain of orgasm❞
~ Dr. Christina Dording et al.
Read in full: A Double-Blind Placebo-Controlled Trial of Maca Root as Treatment for Antidepressant-Induced Sexual Dysfunction in Women
As for men, well these mice (not technically men) found it beneficial too:
Effects of combined extracts of Lepidium meyenii and Allium tuberosum Rottl. on [e-word] dysfunction
(pardon the censorship; we’re trying to avoid people’s spam filters)
It did also improve fertility (and, actually in real men this time):
Does Lepidium meyenii (Maca) improve seminal quality?
Oh, to be in the mood
Here’s an interesting study in which 3g/day yielded significant mood improvement in these 175 (human) subjects:
And yes, it was found to be “well-tolerated” which is scientist-speak for “this appears to be completely safe, but we don’t want to commit ourselves to an absolutist statement and we can’t prove a negative”.
Oh, to have the energy
As it turns out, maca root does also offer benefits in this regard too:
(that’s not an added ingredient; it’s just a relevant chemical that the root naturally contains)
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Ex-Cyclone Alfred has left flooding in its wake. Here’s how floods affect our health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ex-Cyclone Alfred is bringing significant rainfall to southeast Queensland and the Northern Rivers of New South Wales. Flooding has hit Lismore, Ballina, Grafton, Brisbane and Hervey Bay, which received 150 mm of rainfall in two hours this morning.
Tragically, a 61-year-old man died after being swept away in floodwaters near Dorrigo in northern New South Wales.
More heavy rain and flash flooding is expected in the coming days as the weather system moves inland and weakens.
Climate change is making these weather events more intense and frequent. Earlier this year, far north Queensland experienced major flooding. As residents of the Northern Rivers, this latest disaster is especially tough because only three years ago we faced the catastrophic 2022 floods.
We’ve studied the impact of floods on human health and wellbeing, and found floods are linked to a range of physical and mental health effects in both the short- and long-term.
So what might you experience if you live in an area affected by these floods?
We reviewed the evidence
We recently reviewed research on the physical and mental health impacts of floods across mainland Australia. We included 69 studies in our review, published over 70 years. The majority were from the past ten years, examining the effects of floods in Queensland and NSW.
These studies suggest people can expect a range of health impacts. Immediate physical health effects of floods include drowning, falls and injuries.
Chronic diseases such as diabetes or renal disease can also worsen due to factors such as reduced access to transport, health-care services, medications and hospitals.
Exposure to contaminated floodwaters can lead to skin infections, while respiratory problems can occur due to mould and damp housing in the aftermath of floods.
Floods also create ideal conditions for mosquito borne infections such as Ross River virus and Murray Valley encephalitis, while also spreading infectious diseases including leptospirosis, a bacterial infection from contaminated soil.
There are mental health consequences too
Our review showed floods also affect mental health. The more you’re exposed to floodwaters in your home or business, the worse the mental health impacts are likely to be.
The After the Flood study examined mental health and wellbeing outcomes six months after the 2017 flood in the Northern Rivers. It found people who had floodwater in their home, yard or business, or who were displaced from their home for a more than six months, were much more likely to have probable post-traumatic stress disorder, anxiety or depression, compared to those who didn’t experience flooding or weren’t displaced.
Repeated natural disasters could compound these mental health consequences. Southeast Queensland and the Northern Rivers in NSW have experienced multiple disasters over recent years. The Northern Rivers faced major flooding in 2017, bushfires in 2020, further major floods in 2022, and now Cyclone Alfred in 2025. These repeated disasters have taken a toll on our community, creating a seemingly never-ending cycle of recovery, rebuilding and preparation for the next disaster.
Our understanding of the unique challenges faced by communities which experience multiple disasters is still growing. However, a recent Australian study showed exposure to repeated disasters has a compounding effect on people’s mental health, leading to worse mental health outcomes compared to people who experience a single disaster.
Mums and babies
The health effects of floods extend far beyond the initial emergency and beyond the infections and mental health consequences you might expect.
The Queensland Flood Study tracked pregnant women exposed to the 2011 Brisbane floods. Researchers assessed mothers’ stress related to the flood and tracked them and their children at six weeks old, six months, 16 months, 2.5 years, four and six years. It found some links between prenatal stress and developmental outcomes in children.
Some evidence suggests maternal stress from floods can affect children’s development. Nastyaofly/Shutterstock While the health effects after flooding are diverse, the research to date is not comprehensive. We need to learn more about how floods contribute to or exacerbate existing chronic illnesses, disability and long-term mental health issues.
The impacts are inequitable
Flooding exposes and worsens existing inequalities. Socially vulnerable groups are more likely to be exposed to flooding in their homes and have less access to resources to respond and recover from these events, putting some groups at higher risk of negative health impacts afterwards.
Some research has looked at the disproportionate impacts on people with disabilities and their carers, First Nations communities and people from disadvantaged backgrounds.
After the 2017 Northern Rivers floods, for example, people with disability and their carers were more likely than others to:
- experience disrupted access to food, support networks and essentials such as health care and social services
- continue to be distressed about the flood six months after it happened
- be at relatively high risk of post-traumatic stress disorder six months after the flood.
However, targeted flood research exploring the experiences of these vulnerable groups in Australia is limited.
Moving forward, it’s vital we examine the varied impacts of flood events for more vulnerable groups, so we can better support them in the wake of devastating events such as Cyclone Alfred.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Jodie Bailie, Senior Research Fellow, The University Centre for Rural Health and The Centre for Disability Research and Policy, University of Sydney; Jo Longman, Senior Research Fellow, The University Centre for Rural Health, University of Sydney; Rebecca McNaught, Research Fellow, Rural and Remote Health, University of Sydney, and Ross Bailie, School of Public Health, Honorary Professor, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
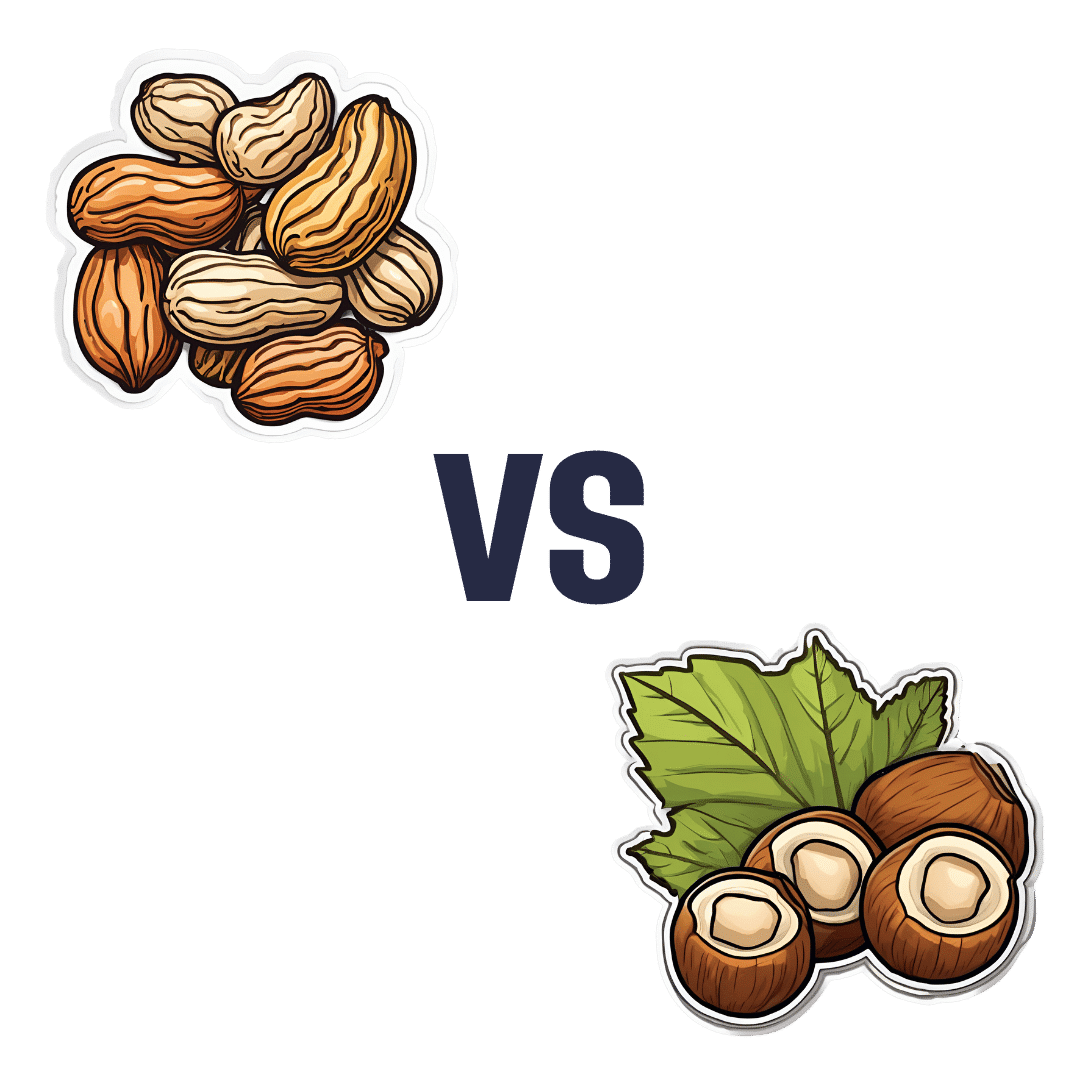
Peanuts vs Hazelnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peanuts to hazelnuts, we picked the hazelnuts.
Why?
It was close!
In terms of macros, peanuts have more protein while hazelnuts have more fiber and fat; the fat is healthy (mostly monounsaturated, some polyunsaturated, and very little saturated; less saturated fat than peanuts), so all in all, we’ll call this category a modest, subjective win for hazelnuts (since it depends on what we consider most important).
In the category of vitamins, peanuts have more of vitamins B2, B3, B5, B9, and choline, while hazelnuts have more of vitamins A, B1, B6, C, E, and K, making this one a marginal win for hazelnuts.
When it comes to minerals, peanuts have more magnesium, phosphorus, selenium, and zinc, while hazelnuts have more calcium, copper, iron, and manganese, so we’re calling it a tie on minerals.
Adding up the sections makes for a very close win for hazelnuts, but by all means enjoy both (unless you are allergic, of course)!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Most People Try The Wrong Way To Unshrimp Their Posture (Here’s How To Do It Better)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many people try to correct posture by pulling the shoulders back and tucking in the chin, but that doesn’t work. Happily, there is a way that does! Kinesiologist Kyle Waugh demonstrates:
Defying gravity
The trick is simple, and is about how maintaining good posture needs to be unconscious and natural, not forced. After all, who is maintaining singular focus for 16 waking hours a day?
Instead, pay attention to how the body relates to gravity without excessive muscle tension, aligning the (oft-forgotten!) hips, and maintaining balance. The importance of hip position is really not to be underestimated, since in many ways the hips are a central axis of the body just as the spine is, and the spine itself sits in the hips.
A lot of what holds the body in poor posture tends to be localized muscle tensions, so address those with stretches and relaxation exercises.
For a few quick tests and exercises to try, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back ← no video on this one, just 6 concepts that you can apply to your daily life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Food for Life – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is, as the author puts it, “an eater’s guide to food and nutrition”. Rather than telling us what to eat or not eat, he provides an overview of what the latest science has to say about various foods, and leaves us to make our own informed decisions.
He also stands firmly by the “personalized nutrition” idea that he introduced in his previous book which we reviewed the other day, and gives advice on what tests we might like to perform.
The writing style is accessible, without shying away from reference to hard science. Dr. Spector provides lots of information about key chemicals, genes, gut bacteria, and more—as well as simply providing a very enjoyable read along the way.
Bottom line: if you’d like a much better idea of what food is (and isn’t) doing what, this book is an invaluable resource.
Click here to check out Food for Life, and make the best decisions for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: