Midwives Blame California Rules for Hampering Birth Centers Amid Maternity Care Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jessie Mazar squeezed the grab handle in her husband’s pickup and groaned as contractions struck her during the 90-minute drive from her home in rural northeastern California to the closest hospital with a maternity unit.
She could have reached Plumas District Hospital, in Quincy, in just seven minutes. But it no longer delivers babies.
Local officials have a plan for a birth center in Quincy, where midwives could deliver babies with backup from on-call doctors and a standby perinatal unit at the hospital, but state health officials have yet to approve it.
That left Mazar to brave the long, winding road — one sometimes blocked by snow, floods, or forest fires — to have her baby. Women across California are facing similar ordeals as hospitals increasingly close money-losing maternity units, especially in rural areas.
Midwife-operated birth centers offer an alternative for women with low-risk pregnancies and can play a crucial role in filling the gap left by hospitals’ retreat from obstetrics, maternal health advocates say.
Declining birth rates, staffing shortages, and financial pressures have led 56 California hospitals — about 1 in 6 — to shutter maternity units over the past dozen years.
But midwives say California’s regulatory regime around birth centers is unnecessarily preventing new centers from opening and leading some existing facilities to close. Obtaining a license can take as long as four years.
“All they’ve essentially done is made it more dangerous to have a baby,” said Sacramento midwife Bethany Sasaki. “People have to drive two hours now because a birth center can’t open, so it’s more dangerous. People are going to be having babies in cars on the side of the road.”
Last month, state Assembly member Mia Bonta introduced legislation to streamline the regulatory process and fix what she calls “a broken system” for licensing birth centers.
“We know that alternative birth centers lead to often better outcomes, lower-risk births, more opportunity for children to be born healthy, and also to lower maternal mortality and morbidity,” she said.
The proposed bill would remove various bureaucratic requirements, though many details have yet to be finalized. Bonta introduced the bill in its current form as a jumping-off point for discussions about how to expedite licensing.
“It’s a starting place,” said Sandra Poole, health policy advocate for the Western Center on Law & Poverty, a co-sponsor of the legislation.
For now, birth centers struggle with a gantlet of rules, only some clearly connected to patient safety. Over the past decade, the number of licensed birth centers in California dropped from 12 to five, according to Bonta.
Plumas County officials are trying to address one key issue: how far a birth center can be from a hospital with a round-the-clock obstetrics unit. State regulations say it can be no more than a 30-minute drive, a distance set when many more hospitals had maternity units.
The first-of-its-kind “Plumas model” aims to take advantage of flexibility provisions in the law to address the obstacle in a way that could potentially be replicated elsewhere in the state.
But the hospital’s application for a birth center and a perinatal unit has been “languishing” with the California Department of Public Health, which is “looking for cover from the legislature,” said Robert Moore, chief medical officer of Partnership HealthPlan of California, a Medi-Cal managed-care plan serving most of Northern California. Asked about the application, a CDPH spokesperson said only that it was under review.
The goal should be for all women to be within an hour’s drive of a hospital with an obstetrics unit, Moore said. Data shows the complication rate goes up after an hour and even higher after two hours, he said, while the benefit is less compelling between 30 and 60 minutes.
Numerous other regulations have made it difficult for birth centers to keep their doors open.
Since August, birth centers in Sacramento and Monterey have had to stop operating because their heating ducts failed to meet licensing requirements. The facilities fall under the same state Department of Health Care Access and Information regulations as primary care clinics, though birth centers see healthy families, not sick ones, and don’t need hospital-grade ventilation, said midwife Caroline Cusenza.
She had spent $50,000 remodeling the Monterey Birth & Wellness Center to include state-required items, such as nursing and hand-washing stations and a housekeeping closet. In the end, a requirement for galvanized steel heating vents, which would have required opening the ceiling at an unaffordable cost, prompted her heart-wrenching decision to close.
“We’re turning women away in tears,” said Sasaki, who owned Midtown Birth Center in Sacramento. She bought the building for $760,000 and spent $250,000 remodeling it in a way she believed met all licensing requirements. But regulators would not license it unless the heating system was redone. Sasaki estimated it would have cost an additional $50,000 to bring it into compliance — too much to keep operating.
She blamed her closure on “regulatory dysfunction.”
Legislation signed by Gov. Gavin Newsom last year could ease onerous building codes such as those governing Sasaki’s and Cusenza’s heating systems, said Poole, the health policy advocate.
The state has taken two to four years to issue birth center licenses, according to a brief by the Osher Center for Integrative Health at the University of California-San Francisco. The state Department of Public Health “works tirelessly to ensure health facilities are able to be properly licensed and follow all applicable requirements within our authority before and during their operation,” spokesperson Mark Smith said.
Bonta, an Oakland Democrat who chairs the Assembly’s health committee, said she would consider increasing the allowable drive time between a birth center and a hospital maternity unit as part of her new legislation.
The state last updated birth center regulations more than a decade ago, before hospitals’ mass exodus from obstetrics. “The hurdle is the time and distance standards without compromising safety,” Poole said. “But where there’s nothing right now, we would say a birth center is certainly a better alternative to not having any maternal care.”
Moore noted that midwife-led births in homes and birth centers are the mainstay of obstetric care in Europe, where the infant mortality rate is considerably lower than in the U.S. More than 98% of American babies are born in hospitals.
Babies delivered by midwives are more likely to be born vaginally, less likely to require intensive care, and more likely to breastfeed, the California Maternal Quality Care Collaborative has found. Midwife-led births also lead to fewer infant emergency room visits, hospitalizations, and neonatal deaths. And they cost far less: Birth centers generally charge one-quarter or less of the average cost of about $36,000 for a vaginal birth in a California hospital.
If they catered only to private-pay clients, Cusenza and Sasaki could have continued operating without licenses. They must be licensed, however, to receive payments from Medi-Cal and some private insurance companies, which they needed to remain in business. Medi-Cal, the state’s Medicaid health insurance program, which covers low-income residents, paid for about 40% of the state’s births in 2022.
Bonta has heard reports from midwives that the key to getting licensed is hunting down the right state health department advocate. “I don’t believe that we should be building resources based on the model of ‘Where’s Waldo?’ in finding a champion inside CDPH,” she said.
Lori Link, director of midwifery at Plumas District Hospital, believes the Plumas model can turn what’s become a maternity desert into an oasis. Jessie Mazar, whose son was born in September without complications at a Truckee hospital, would welcome the opportunity to deliver her planned second child in Quincy.
“That would be convenient,” she said. “We’re not holding our breath.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dandelion Greens vs Collard Greens – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dandelion greens to collard greens, we picked the dandelion greens.
Why?
Collard greens are great—they even beat kale in one of our previous “This or That” articles!—but dandelion greens simply pack more of a nutritional punch:
In terms of macros, dandelions have slightly more carbs (+3g/100g) for the same protein and fiber, and/but the glycemic index is equal (zero), so those carbs aren’t anything to worry about. Nobody is getting metabolic disease by getting their carbs from dandelion leaves. In short, we’re calling it a tie on macros, though it could nominally swing either way if you have an opinion (one way or the other) about the extra 3g of carbs.
In the category of vitamins, things are more exciting: dandelion greens have more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K, while collard greens have more vitamin B5. An easy and clear win for dandelions.
Looking at the minerals tells a similar story; dandelion greens have much more calcium, copper, iron, magnesium, phosphorus, potassium, and zinc, while collard greens have slightly more manganese. Another overwhelming win for dandelions.
One more category, polyphenols. We’d be here until next week if we listed all the polyphenols that dandelion greens have, but suffice it to say, dandelion greens have a total of 385.55mg/100g polyphenols, while collard greens have a total of 0.08mg/100g polyphenols. Grabbing a calculator, we see that this means dandelions have more than 4819x the polyphenol content that collard greens do.
So, “eat leafy greens” is great advice, but they are definitely not all created equal!
Let us take this moment to exhort: if you have any space at home where you can grow dandelions, grow them!
Not only are they great for pollinators, but also they beat the collard greens that beat kale. And you can have as much as you want, for free, right there.
Want to learn more?
You might like to read:
Collard Greens vs Kale – Which is Healthier?
Enjoy!
Share This Post
-
Vital Aspects of Holistic Wellness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I am interested in the following: Aging, Exercise, Diet, Relationships, Purpose, Lowering Stress
You’re going to love our Psychology Sunday editions of 10almonds! You might like some of these…
- Relationships: Seriously Useful Communication Skills!
- Purpose: Are You Flourishing? (There’s a Scale)
- Managing stress: Lower Your Cortisol! (Here’s Why & How)
- Also about managing stress: Sunday Stress-Buster
- Also applicable to stress: How To Set Your Anxiety Aside
Share This Post
-
The BAT-pause!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Cold Weather & The Menopause Battle It Out
You may know that (moderate, safe) exposure to the cold allows our body to convert our white and yellow fat into the much healthier brown fat—also called brown adipose tissue, or “BAT” to its friends.
If you didn’t already know that, then well, neither did scientists until about 15 years ago:
The Changed Metabolic World with Human Brown Adipose Tissue: Therapeutic Visions
You can read more about it here:
Cool Temperature Alters Human Fat and Metabolism
This is important, especially because the white fat that gets converted is the kind that makes up most visceral fat—the kind most associated with all-cause mortality:
Visceral Belly Fat & How To Lose It ← this is not the same as your subcutaneous fat, the kind that sits directly under your skin and keeps you warm; this is the fat that goes between your organs and of which we should only have a small amount!
The BAT-pause
It’s been known (since before the above discovery) that BAT production slows considerably as we get older. Not too shocking—after all, many metabolic functions slow as we get older, so why should fat regulation be any different?
But! Rodent studies found that this was tied less to age, but to ovarian function: rats who underwent ovariectomies suffered reduced BAT production, regardless of their age.
Naturally, it’s been difficult to recreate such studies in humans, because it’s difficult to find a large sample of young adults willing to have their ovaries whipped out (or even suppressed chemically) to see how badly their metabolism suffers as a result.
Nor can an observational study (for example, of people who incidentally have ovaries removed due to ovarian cancer) usefully be undertaken, because then the cancer itself and any additional cancer treatments would be confounding factors.
Perimenopausal study to the rescue!
A recent (published last month, at time of writing!) study looked at women around the age of menopause, but specifically in cohorts before and after, measuring BAT metabolism.
By dividing the participants into groups based on age and menopausal status, and dividing the post-menopausal group into “takes HRT” and “no HRT” groups, and dividing the pre-menopausal group into “normal ovarian function” and “ovarian production of estrogen suppressed to mimic slightly early menopause” groups (there’s a drug for that), and then having groups exposed to warm and cold temperatures, and measuring BAT metabolism in all cases, they were able to find…
It is about estrogen, not age!
You can read more about the study here:
“Good” fat metabolism changes tied to estrogen loss, not necessarily to aging, shows study
…and the study itself, here:
Brown adipose tissue metabolism in women is dependent on ovarian status
What does this mean for men?
This means nothing directly for (cis) men, sorry.
But to satisfy your likely curiosity: yes, testosterone does at least moderately suppress BAT metabolism—based on rodent studies, anyway, because again it’s difficult to find enough human volunteers willing to have their testicles removed for science (without there being other confounding variables in play, anyway):
Testosterone reduces metabolic brown fat activity in male mice
So, that’s bad per se, but there isn’t much to be done about it, since the rest of your (addressing our male readers here) metabolism runs on testosterone, as do many of your bodily functions, and you would suffer many unwanted effects without it.
However, as men do typically have notably less body fat in general than women (this is regulated by hormones), the effects of changes in BAT metabolism are rather less pronounced in men (per testosterone level changes) than in women (per estrogen level changes), because there’s less overall fat to convert.
In summary…
While menopausal HRT is not necessarily a silver bullet to all metabolic problems, its BAT-maintaining ability is certainly one more thing in its favor.
See also:
Dr. Jen Gunter | What You Should Have Been Told About The Menopause Beforehand
Take care!
Share This Post
Related Posts
-
What’s the difference between a heart attack and cardiac arrest? One’s about plumbing, the other wiring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In July 2023, rising US basketball star Bronny James collapsed on the court during practice and was sent to hospital. The 18-year-old athlete, son of famous LA Lakers’ veteran LeBron James, had experienced a cardiac arrest.
Many media outlets incorrectly referred to the event as a “heart attack” or used the terms interchangeably.
A cardiac arrest and a heart attack are distinct yet overlapping concepts associated with the heart.
With some background in how the heart works, we can see how they differ and how they’re related.
Explode/Shutterstock Understanding the heart
The heart is a muscle that contracts to work as a pump. When it contracts it pushes blood – containing oxygen and nutrients – to all the tissues of our body.
For the heart muscle to work effectively as a pump, it needs to be fed its own blood supply, delivered by the coronary arteries. If these arteries are blocked, the heart muscle doesn’t get the blood it needs.
This can cause the heart muscle to become injured or die, and results in the heart not pumping properly.
Heart attack or cardiac arrest?
Simply put, a heart attack, technically known as a myocardial infarction, describes injury to, or death of, the heart muscle.
A cardiac arrest, sometimes called a sudden cardiac arrest, is when the heart stops beating, or put another way, stops working as an effective pump.
In other words, both relate to the heart not working as it should, but for different reasons. As we’ll see later, one can lead to the other.
Why do they happen? Who’s at risk?
Heart attacks typically result from blockages in the coronary arteries. Sometimes this is called coronary artery disease, but in Australia, we tend to refer to it as ischaemic heart disease.
The underlying cause in about 75% of people is a process called atherosclerosis. This is where fatty and fibrous tissue build up in the walls of the coronary arteries, forming a plaque. The plaque can block the blood vessel or, in some instances, lead to the formation of a blood clot.
Atherosclerosis is a long-term, stealthy process, with a number of risk factors that can sneak up on anyone. High blood pressure, high cholesterol, diet, diabetes, stress, and your genes have all been implicated in this plaque-building process.
Other causes of heart attacks include spasms of the coronary arteries (causing them to constrict), chest trauma, or anything else that reduces blood flow to the heart muscle.
Regardless of the cause, blocking or reducing the flow of blood through these pipes can result in the heart muscle not receiving enough oxygen and nutrients. So cells in the heart muscle can be injured or die.
Here’s a simple way to remember the difference. Author provided But a cardiac arrest is the result of heartbeat irregularities, making it harder for the heart to pump blood effectively around the body. These heartbeat irregularities are generally due to electrical malfunctions in the heart. There are four distinct types:
- ventricular tachycardia: a rapid and abnormal heart rhythm in which the heartbeat is more than 100 beats per minute (normal adult, resting heart rate is generally 60-90 beats per minute). This fast heart rate prevents the heart from filling with blood and thus pumping adequately
- ventricular fibrillation: instead of regular beats, the heart quivers or “fibrillates”, resembling a bag of worms, resulting in an irregular heartbeat greater than 300 beats per minute
- pulseless electrical activity: arises when the heart muscle fails to generate sufficient pumping force after electrical stimulation, resulting in no pulse
- asystole: the classic flat-line heart rhythm you see in movies, indicating no electrical activity in the heart.
Remember this flat-line rhythm from the movies? It’s asystole, when there’s no electrical activity in the heart. Kateryna Kon/Shutterstock Cardiac arrest can arise from numerous underlying conditions, both heart-related and not, such as drowning, trauma, asphyxia, electrical shock and drug overdose. James’ cardiac arrest was attributed to a congenital heart defect, a heart condition he was born with.
But among the many causes of a cardiac arrest, ischaemic heart disease, such as a heart attack, stands out as the most common cause, accounting for 70% of all cases.
So how can a heart attack cause a cardiac arrest? You’ll remember that during a heart attack, heart muscle can be damaged or parts of it may die. This damaged or dead tissue can disrupt the heart’s ability to conduct electrical signals, increasing the risk of developing arrhythmias, possibly causing a cardiac arrest.
So while a heart attack is a common cause of cardiac arrest, a cardiac arrest generally does not cause a heart attack.
What do they look like?
Because a cardiac arrest results in the sudden loss of effective heart pumping, the most common signs and symptoms are a sudden loss of consciousness, absence of pulse or heartbeat, stopping of breathing, and pale or blue-tinged skin.
But the common signs and symptoms of a heart attack include chest pain or discomfort, which can show up in other regions of the body such as the arms, back, neck, jaw, or stomach. Also frequent are shortness of breath, nausea, light-headedness, looking pale, and sweating.
What’s the take-home message?
While both heart attack and cardiac arrest are disorders related to the heart, they differ in their mechanisms and outcomes.
A heart attack is like a blockage in the plumbing supplying water to a house. But a cardiac arrest is like an electrical malfunction in the house’s wiring.
Despite their different nature both conditions can have severe consequences and require immediate medical attention.
Michael Todorovic, Associate Professor of Medicine, Bond University and Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
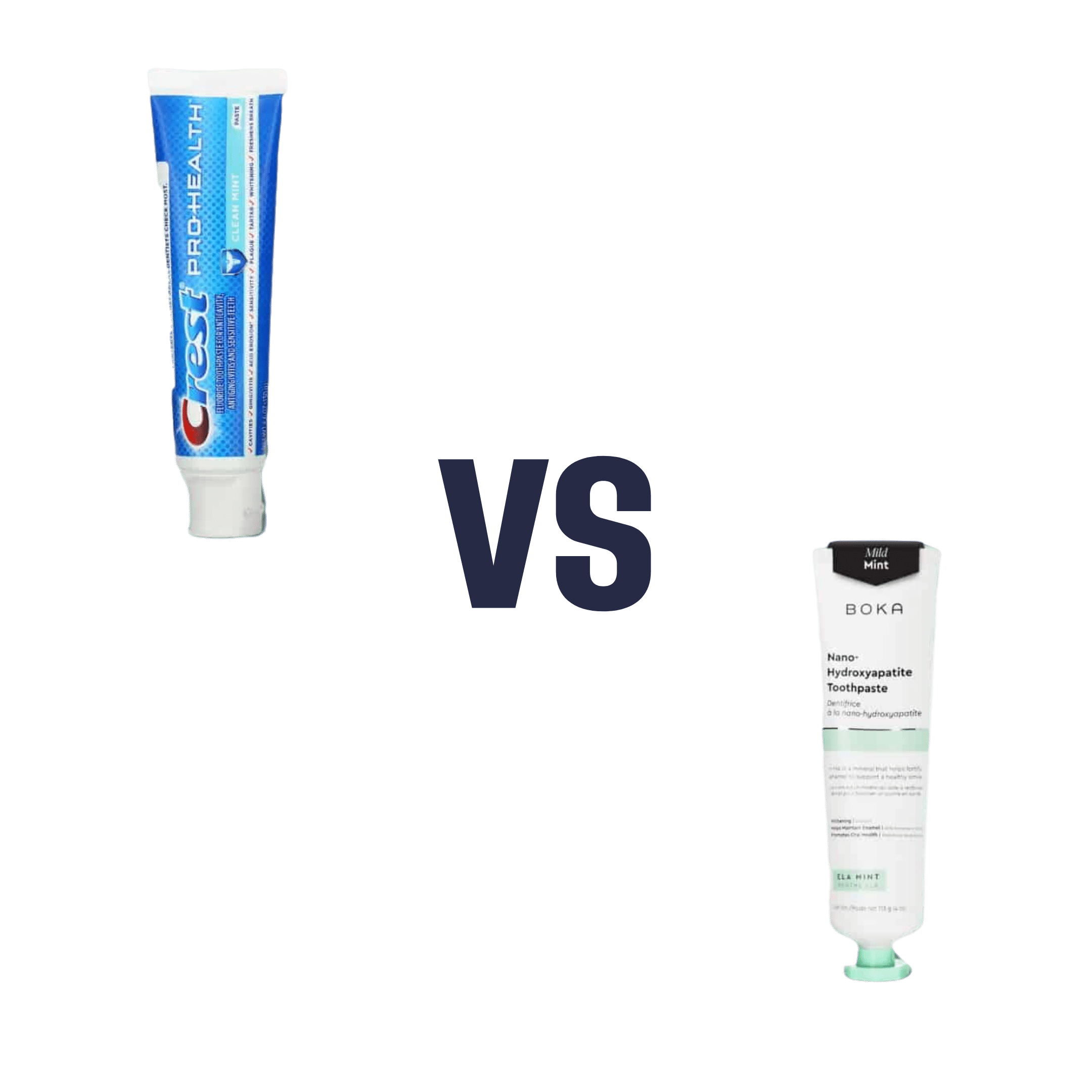
Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fluoride toothpaste to non-fluoride toothpaste, we picked the fluoride.
Why?
Fluoride is indeed toxic; that’s why it’s in toothpaste (to kill things; namely, bacteria whose waste products would harm our teeth). However, we are much bigger than those bacteria.
Given the amount of fluoride in toothpaste (usually under 1mg per strip of toothpaste to cover a toothbrush head), the amount that people swallow unintentionally (about 1/20th of that, so about 0.1mg daily if brushing teeth twice daily), and the toxicity level of fluoride (32–64mg/kg), then even if we take the most dangerous ends of all those numbers (and an average body size), to suffer ill effects from fluoride due to brushing your teeth, would require that you brush your teeth more than 23,000 times per day.
Alternatively, if you were to ravenously eat the toothpaste instead of spitting it out, you’d only need to brush your teeth a little over 1,000 times per day.
All the same, please don’t eat toothpaste; that’s not the message here.
However! In head-to-head tests, fluoride toothpaste has almost always beaten non-fluoride toothpaste.
Almost? Yes, almost: hydroxyapatite performed equally in one study, but that’s not usually an option on as many supermarket shelves.
We found some on Amazon, though, which is the one we used for today’s head-to-head. Here it is:
However, before you rush to buy it, do be aware that the toxicity of hydroxyapatite appears to be about twice that of fluoride:
Scientific Committee on Consumer Safety Opinion On Hydroxyapatite (Nano)
…which is still very safe (you’d need to brush your teeth, and eat all the toothpaste, about 500 times per day, to get to toxic levels, if we run with the same numbers we discussed before. Again, please do not do that, though).
But, since the science so far suggests it’s about twice as toxic as fluoride, then regardless of that still being very safe, the fluoride is obviously (by the same metric) twice as safe, hence picking the fluoride.
Want more options?
Check out our previous main feature:
Less Common Oral Hygiene Options
(the above article also links back to our discussion of different toothpastes and mouthwashes, by the way)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How often should you really weigh yourself?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Few topics are more debated in health than the value of the humble bathroom scale. Some experts advocate daily self-weigh-ins to promote accountability for weight management, particularly when we’re following a diet and exercise program to lose weight.
Others suggest ditching self-weigh-ins altogether, arguing they can trigger negative psychological responses and unhealthy behaviours when we don’t like, or understand, the number we see on the scale.
Many, like me, recommend using scales to weigh yourself weekly, even when we’re not trying to lose weight. Here’s why.
Diva Plavalaguna/Pexels 1. Weighing weekly helps you manage your weight
Research confirms regular self-weighing is an effective weight loss and management strategy, primarily because it helps increase awareness of our current weight and any changes.
A systematic review of 12 studies found participants who weighed themselves weekly or daily over several months lost 1–3 BMI (body mass index) units more and regained less weight than participants who didn’t weight themselves frequently. The weight-loss benefit was evident with weekly weighing; there was no added benefit with daily weighing.
Weighing regularly means we know when our weight changes. Andres Ayrton/Pexels Self-weigh-ins are an essential tool for weight management as we age. Adults tend to gain weight progressively through middle age. While the average weight gain is typically between 0.5–1kg per year, this modest accumulation of weight can lead to obesity over time. Weekly weighing and keeping track of the results helps avoid unnecessary weight gain.
Tracking our weight can also help identify medical issues early. Dramatic changes in weight can be an early sign of some conditions, including problems with our thyroid, digestion and diabetes.
2. Weekly weighing accounts for normal fluctuations
Our body weight can fluctuate within a single day and across the days of the week. Studies show body weight fluctuates by 0.35% within the week and it’s typically higher after the weekend.
Daily and day-to-day body weight fluctuations have several causes, many linked to our body’s water content. The more common causes include:
The type of food we’ve consumed
When we’ve eaten a dinner higher in carbohydrates, we’ll weigh more the next day. This change is a result of our bodies temporarily carrying more water. We retain 3–4 grams of water per gram of carbohydrate consumed to store the energy we take from carbs.
Our water content also increases when we consume foods higher in salt. Our bodies try to maintain a balance of sodium and water. When the concentration of salt in our bloodstream increases, a mechanism is triggered to restore balance by retaining water to dilute the excess salt.
The morning after a big pasta dinner, we’ll carry more water weight. Dana Tentis/Pexels Our food intake
Whether it’s 30 grams of nuts or 65 grams of lean meat, everything we eat and drink has weight, which increases our body weight temporarily while we digest and metabolise what we’ve consumed.
Our weight also tends to be lower first thing in the morning after our food intake has been restricted overnight and higher in the evening after our daily intake of food and drinks.
Exercise
If we weigh ourselves at the gym after a workout, there’s a good chance we’ll weigh less due to sweat-induced fluid loss. The amount of water lost varies depending on things like our workout intensity and duration, the temperature and humidity, along with our sweat rate and hydration level. On average, we lose 1 litre of sweat during an hour of moderate-intensity exercise.
Hormonal changes
Fluctuations in hormones within your menstrual cycle can also affect fluid balance. Women may experience fluid retention and temporarily gain 0.5–2kg of weight at this time. Specifically, the luteal phase, which represents the second half of a woman’s cycle, results in a shift of fluid from your blood plasma to your cells, and bloating.
Most of our weight fluctuations are water-related. Engin Akyurt/Unsplash Bowel movements
Going to the bathroom can lead to small but immediate weight loss as waste is eliminated from the body. While the amount lost will vary, we generally eliminate around 100 grams of weight through our daily bowel movements.
All of these fluctuations are normal, and they’re not indicative of significant changes in our body fat or muscle mass. However, seeing these fluctuations can lead to unnecessary stress and a fixation with our weight.
3. Weekly weighing avoids scale obsession and weight-loss sabotage
Weighing too frequently can create an obsession with the number on the scales and do more harm than good.
Often, our reaction when we see this number not moving in the direction we want or expect is to further restrict our food intake or embark on fad dieting. Along with not being enjoyable or sustainable, fad diets also ultimately increase our weight gain rather than reversing it.
This was confirmed in a long-term study comparing intentional weight loss among more than 4,000 twins. The researchers found the likelihood of becoming overweight by the age of 25 was significantly greater for a twin who dieted to lose 5kg or more. This suggests frequent dieting makes us more susceptible to weight gain and prone to future weight gain.
So what should you do?
Weighing ourselves weekly gives a more accurate measure of our weight trends over time.
Aim to weigh yourself on the same day, at the same time and in the same environment each week – for example, first thing every Friday morning when you’re getting ready to take a shower, after you’ve gone to the bathroom, but before you’ve drunk or eaten anything.
Weigh yourself at the same time on the same day of the week. Alexanderstock23/Shutterstock Use the best quality scales you can afford. Change the batteries regularly and check their accuracy by using a “known” weight – for example, a 10kg weight plate. Place the “known” weight on the scale and check the measurement aligns with the “known” weight.
Remember, the number on the scale is just one part of health and weight management. Focusing solely on it can overshadow other indicators, such as how your clothes fit. It’s also essential to pay equal attention to how we’re feeling, physically and emotionally.
Stop weighing yourself – at any time interval – if it’s triggering anxiety or stress, and get in touch with a health-care professional to discuss this.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: