Wildfires ignite infection risks, by weakening the body’s immune defences and spreading bugs in smoke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past several days, the world has watched on in shock as wildfires have devastated large parts of Los Angeles.
Beyond the obvious destruction – to landscapes, homes, businesses and more – fires at this scale have far-reaching effects on communities. A number of these concern human health.
We know fire can harm directly, causing injuries and death. Tragically, the death toll in LA is now at least 24.
But wildfires, or bushfires, can also have indirect consequences for human health. In particular, they can promote the incidence and spread of a range of infections.
Effects on the immune system
Most people appreciate that fires can cause burns and smoke inhalation, both of which can be life-threatening in their own right.
What’s perhaps less well known is that both burns and smoke inhalation can cause acute and chronic changes in the immune system. This can leave those affected vulnerable to infections at the time of the injury, and for years to come.
Burns induce profound changes in the immune system. Some parts go into overdrive, becoming too reactive and leading to hyper-inflammation. In the immediate aftermath of serious burns, this can contribute to sepsis and organ failure.
Other parts of the immune system appear to be suppressed. Our ability to recognise and fight off bugs can be compromised after sustaining burns. Research shows people who have experienced serious burns have an increased risk of influenza, pneumonia and other types of respiratory infections for at least the first five years after injury compared to people who haven’t experienced burns.
Wildfire smoke is a complex mixture containing particulate matter, volatile organic compounds, ozone, toxic gases, and microbes. When people inhale smoke during wildfires, each of these elements can play a role in increasing inflammation in the airways, which can lead to increased susceptibility to respiratory infections and asthma.
Research published after Australia’s Black Summer of 2019–20 found a higher risk of COVID infections in areas of New South Wales where bushfires had occurred weeks earlier.
We need more research to understand the magnitude of these increased risks, how long they persist after exposure, and the mechanisms. But these effects are thought to be due to sustained changes to the immune response.
Microbes travel in smoky air
Another opportunity for infection arises from the fire-induced movement of microbes from niches they usually occupy in soils and plants in natural areas, into densely populated urban areas.
Recent evidence from forest fires in Utah shows microbes, such as bacteria and fungal spores, can be transported in smoke. These microbes are associated with particles from the source, such as burned vegetation and soil.
There are thousands of different species of microbes in smoke, many of which are not common in background, non-smoky air.
Only a small number of studies on this have been published so far, but researchers have shown the majority of microbes in smoke are still alive and remain alive in smoke long enough to colonise the places where they eventually land.
How far specific microbes can be transported remains an open question, but fungi associated with smoke particles have been detected hundreds of miles downwind from wildfires, even weeks after the fire.
So does this cause human infections?
A subset of these airborne microbes are known to cause infections in humans.
Scientists are probing records of human fungal infections in relation to wildfire smoke exposure. In particular, they’re looking at soil-borne infectious agents such as the fungi Coccidioides immitis and Coccidioides posadasii which thrive in dry soils that can be picked up in dust and smoke plumes.
These fungi cause valley fever, a lung infection with symptoms that can resemble the flu, across arid western parts of the United States.
A study of wildland firefighters in California showed high rates of valley fever infections, which spurred occupational health warnings including recommended use of respirators when in endemic regions.
A California-based study of the wider population showed a 20% increase in hospital admissions for valley fever following any amount of exposure to wildfire smoke.
However, another found only limited evidence of excess cases after smoke exposure in wildfire-adjacent populations in California’s San Joaquin Valley.
These contrasting results show more research is needed to evaluate the infectious potential of wildfire smoke from this and other fungal and bacterial causes.
Staying safe
Much remains to be learned about the links between wildfires and infections, and the multiple pathways by which wildfires can increase the risk of certain infections.
There’s also a risk people gathering together after a disaster like this, such as in potentially overcrowded shelters, can increase the transmission of infections. We’ve seen this happen after previous natural disasters.
Despite the gaps in our knowledge, public health responses to wildfires should encompass infection prevention (such as through the provision of effective masks) and surveillance to enable early detection and effective management of any outbreaks.
Christine Carson, Senior Research Fellow, School of Medicine, The University of Western Australia and Leda Kobziar, Professor of Wildland Fire Science, University of Idaho
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your Brain On (And Off) Estrogen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
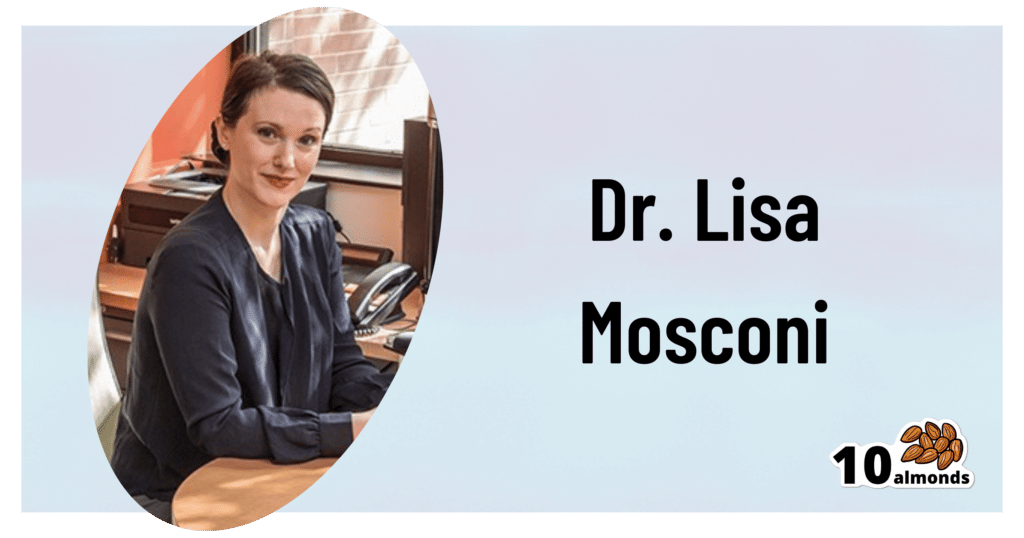
This is Dr. Lisa Mosconi. She’s a professor of Neuroscience in Neurology and Radiology, and is one of the 1% most influential scientists of the 21st century. That’s not a random number or an exaggeration; it has to do with citation metrics collated over 20 years:
A standardized citation metrics author database annotated for scientific field
What does she want us to know?
Women’s brains age differently from men’s
This is largely, of course, due to menopause, and as such is a generalization, but it’s a statistically safe generalization, because:
- Most women go through menopause—and most women who don’t, avoid it by dying pre-menopause, so the aging also does not occur in those cases
- Menopause is very rarely treated immediately—not least of all because menopause is diagnosed officially when it has been one year since one’s last period, so there’s almost always a year of “probably” first, and often numerous years, in the case of periods slowing down before stopping
- Menopausal HRT is great, but doesn’t completely negate that menopause occurred—because of the delay in starting HRT, some damage can be done already and can take years to reverse.
Medicated and unmedicated menopause proceed very differently from each other, and this fact has historically caused obfuscation of a lot of research into age-related neurodegeneration.
For example, it is well-established that women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
Superficially, one might conclude “estrogen is to blame” or maybe “the xx-chromosomal karyotype is to blame”.
The opposite, however, is true with regard to estrogen—estrogen appears to be a protective factor in women’s neurological health, which is why increased neurodegeneration occurs when estrogen levels decline (for example, in menopause).
For a full rundown on this, see:
Alzheimer’s Sex Differences May Not Be What They Appear
It’s not about the extra X
Dr. Mosconi examines this in detail in her book “The XX Brain”. To summarize and oversimplify a little: the XX karyotype by itself makes no difference, or more accurately, the XY karyotype by itself makes no difference (because biologically speaking, female physiological attributes are more “default” than male ones; it is only 12,000ish* years of culture that has flipped the social script on this).
*Why 12,000ish years? It’s because patriarchalism largely began with settled agriculture, for reasons that are fascinating but beyond the scope of this article, which is about health science, not archeology.
The topic of “which is biologically default” is relevant, because the XY karyotype (usually) informs the body “ignore previous instructions about ovaries, and adjust slightly to make them into testes instead”, which in turn (usually) results in a testosterone-driven system instead of an estrogen-driven system. And that is what makes the difference to the brain.
One way we can see that it’s about the hormones not the chromosomes, is in cases of androgen insensitivity syndrome, in which the natal “congratulations, it’s a girl” pronouncement may later be in conflict with the fact it turns out she had XY chromosomes all along, but the androgenic instructions never got delivered successfully, so she popped out with fairly typical female organs. And, relevantly for Dr. Mosconi, a typically female brain that will age in a typically female fashion, because it’s driven by estrogen, regardless of the Y-chromosome.
The good news
The good news from all of this is that while we can’t (with current science, anyway) do much about our chromosomes, we can do plenty about our hormones, and also, the results of changes in same.
Remember, Dr. Mosconi is not an endocrinologist, nor a gynecologist, but a neurologist. As such, she makes the case for how a true interdisciplinary team for treating menopause should not confined to the narrow fields usually associated with “bikini medicine”, but should take into account that a lot of menopause-related changes are neurological in nature.
We recently reviewed another book by Dr. Mosconi:
The Menopause Brain – by Dr. Lisa Mosconi
…and as we noted there, many sources will mention “brain fog” as a symptom of menopause, Dr. Mosconi can (and will) point to a shadowy patch on a brain scan and say “that’s the brain fog, there”.
And so on, for other symptoms that are often dismissed as “all in your head”, as though that’s a perfectly acceptable place for problems to be.
This is critical, because it’s treating real neurological things as the real things they are.
Dr. Mosconi’s advice, beyond HRT
Dr. Mosconi notes that brain health tends to dip during perimenopause but often recovers, showing the brain’s resilience to hormonal shifts. As such, all is not lost if for whatever reason, hormone replacement therapy isn’t a viable option for you.
Estrogen plays a crucial role in brain energy, and women’s declining estrogen levels during menopause increase the need for antioxidants to protect brain health—something not often talked about.
Specifically, Dr. Mosconi tells us, women need more antioxidants and have different metabolic responses to diets compared to men.*
*Yes, even though men usually have negligible estrogen, because their body (and thus brain, being also part of their body) is running on testosterone instead, which is something that will only happen if either you are producing normal male amounts of testosterone (requires normal male testes) or you are taking normal male amounts of testosterone (requires big bottles of testosterone; this isn’t the kind of thing you can get from a low dose of testogel as sometimes prescribed as part of menopausal HRT to perk your metabolism up).
Note: despite women being a slight majority on Earth, and despite an aging population in wealthy nations, meaning “a perimenopausal woman” is thus the statistically average person in, for example, the US, and despite the biological primacy of femaleness… Medicine still mostly looks to men as the “default person”, which in this case can result in seriously low-balled estimates of what antioxidants are needed.
In terms of supplements, therefore, she recommends:
- Antioxidants: key for brain health, especially in women. Rich sources include fruits (especially berries) and vegetables. Then there’s the world’s most-consumed antioxidant, which is…
- Coffee: Italian-style espresso has the highest antioxidant power. Adding a bit of fat (e.g. oat milk) helps release caffeine more slowly, reducing jitters. Taking it alongside l-theanine also “flattens the curve” and thus improves its overall benefits.
- Flavonoids: important for both men and women but particularly essential for women. Found in many fruits and vegetables.
- Chocolate: dark chocolate is an excellent source of antioxidants and flavonoids!
- Turmeric: a natural neuroprotectant with anti-inflammatory properties, best boosted by taking with black pepper, which improves absorption as well as having many great qualities of its own.
- B Vitamins: B6, B9, and B12 are essential for anti-aging and brain health; deficiency in B6 is rare, while deficiency in B9 (folate) and especially B12 is very common later in life.
- Vitamins C & E: important antioxidants, but caution is needed with fat-soluble vitamins to avoid toxicity.
- Omega-3s: important for brain health; can be consumed in the diet, but supplements may be necessary.
- Caution with zinc: zinc can support immunity and endocrine health (and thus, indirectly, brain health) but may be harmful in excess, particularly for brain health.
- Probiotics & Prebiotics: beneficial for gut health, and in Dr. Mosconi’s opinion, hard to get sufficient amounts from diet alone.
For more pointers, you might want to check out the MIND diet, that is to say, the “Mediterranean-DASH Intervention for Neurodegenerative Delay” upgrade to make the Mediterranean diet even brain-healthier than it is by default:
Four Ways To Upgrade The Mediterranean Diet
Want to know more from Dr. Mosconi?
Here’s her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically!
Enjoy!
Share This Post
-
Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Share This Post
-
Guava vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing guava to passion fruit, we picked the guava.
Why?
There aren’t many fruits that can beat passion fruit for nutritional density! And even in this case, it wasn’t completely so in every category:
In terms of macros, passion fruit has more carbs and fiber, the ratio of which give it the slightly lower glycemic index. Thus, a modest win for passion fruit in this category.
In the category of vitamins, guava has more of vitamins B1, B5, B6, B9, C, E, and K, while passion fruit has more of vitamins A, B2, and B3. A clear win for guava this time.
When it comes to minerals, it’s a little closer, but: guava has more calcium, copper, manganese, potassium, and zinc, while passion fruit has more iron, magnesium, and phosphorus. So, another win for guava.
Adding up the sections makes for guava winning the day, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Fruit Is Healthy; Juice Isn’t (Here’s Why)
Enjoy!
Share This Post
Related Posts
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance Is Useful! (Especially As We Get Older)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Resistance Is Useful!
At 10almonds we talk a lot about the importance of regular moderate exercise (e.g. walking, gardening, housework, etc), and with good reason: getting in those minutes (at least 150 minutes per week, so, a little over 20 minutes per day, or 25 minutes per day with one day off) is the exericise most consistently linked to better general health outcomes and reduced mortality risk.
We also often come back to mobility, because at the end of the day, being able to reach for something from a kitchen cabinet without doing oneself an injury is generally more important in life than being able to leg-press a car.
Today though, we’re going to talk about resistance training.
What is resistance training?
It can be weight-lifting, or it can be bodyweight exercises. In those cases, what you’re resisting is gravity. It can also be exercises with resistance bands or machines. In all cases, it’s about building and/or maintaining strength.
Why does it matter?
Let’s say you’re not an athlete, soldier, or laborer, and the heaviest thing you have to pick up is a bag of groceries. Strength still matters, for two main reasons:
- Muscle strength correlates to bone strength. You can’t build (or maintain) strong muscles on weak bones, so if you take care of your muscles, then your body will keep your bones strong too.
- That’s assuming you have a good diet as well—but today’s not about that. If you’d like to know more about eating for bone health though, do check out this previous article about that!
- Muscle strength correlates to balance and stability. You can’t keep yourself from falling over if you are physically frail.
Both of those things matter, because falls and fractures often have terrible health outcomes (e.g., slower recovery and more complications) the older we get. So, we want to:
- Ideally, not fall in the first place
- If we do fall, have robust bones
See also: Effects of Resistance Exercise on Bone Health
How much should we do?
Let’s go to the Journal of Strength and Conditioning Research on this one:
❝There is strong evidence to support the benefits of resistance exercise for countering many age-related processes of sarcopenia, muscle weakness, mobility loss, chronic disease, disability, and even premature mortality.
In addition, this Position Statement provides specific evidence-based practice recommendations to aid in the implementation of resistance exercise programs for healthy older adults and those with special considerations.
While there are instances where low-intensity, low-volume programs are appropriate (i.e., beginning programs for individuals with frailty or CVDs), the greatest benefits are possible with progression to moderate to higher intensity programs.❞
~ Fragala et al
Read the statement in full:
There’s a lot of science there and it’s well worth reading if you have the time. It’s particularly good at delineating how much is not enough vs how much is too much, and the extent to which we should (or shouldn’t) train to exhaustion.
If you don’t fancy that, though, and/or just want to start with something accessible and work your way up, the below is a very good (and also evidence-based) start-up plan:
Healthline’s Exercise Plan For Seniors—For Strength, Balance, & Flexibility
(it has a weekly planner, step-by-step guides to the exercises, and very clear illustrative animations of each)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Muscle strength correlates to bone strength. You can’t build (or maintain) strong muscles on weak bones, so if you take care of your muscles, then your body will keep your bones strong too.
-
Pain Clinics Made Millions From ‘Unnecessary’ Injections Into ‘Human Pin Cushions’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McMINNVILLE, Tenn. — Each month, Michelle Shaw went to a pain clinic to get the shots that made her back feel worse — so she could get the pills that made her back feel better.
Shaw, 56, who has been dependent on opioid painkillers since she injured her back in a fall a decade ago, said in both an interview with KFF Health News and in sworn courtroom testimony that the Tennessee clinic would write the prescriptions only if she first agreed to receive three or four “very painful” injections of another medicine along her spine.
The clinic claimed the injections were steroids that would relieve her pain, Shaw said, but with each shot her agony would grow. Shaw said she eventually tried to decline the shots, then the clinic issued an ultimatum: Take the injections or get her painkillers somewhere else.
“I had nowhere else to go at the time,” Shaw testified, according to a federal court transcript. “I was stuck.”
Shaw was among thousands of patients of Pain MD, a multistate pain management company that was once among the nation’s most prolific users of what it referred to as “tendon origin injections,” which normally inject a single dose of steroids to relieve stiff or painful joints. As many doctors were scaling back their use of prescription painkillers due to the opioid crisis, Pain MD paired opioids with monthly injections into patients’ backs, claiming the shots could ease pain and potentially lessen reliance on painkillers, according to federal court documents.
Now, years later, Pain MD’s injections have been proved in court to be part of a decade-long fraud scheme that made millions by capitalizing on patients’ dependence on opioids. The Department of Justice has successfully argued at trial that Pain MD’s “unnecessary and expensive injections” were largely ineffective because they targeted the wrong body part, contained short-lived numbing medications but no steroids, and appeared to be based on test shots given to cadavers — people who felt neither pain nor relief because they were dead.
Four Pain MD employees have pleaded guilty or been convicted of health care fraud, including company president Michael Kestner, who was found guilty of 13 felonies at an October trial in Nashville, Tennessee. According to a transcript from Kestner’s trial that became public in December, witnesses testified that the company documented giving patients about 700,000 total injections over about eight years and said some patients got as many as 24 shots at once.
“The defendant, Michael Kestner, found out about an injection that could be billed a lot and paid well,” said federal prosecutor James V. Hayes as the trial began, according to the transcript. “And they turned some patients into human pin cushions.”
The Department of Justice declined to comment for this article. Kestner’s attorneys either declined to comment or did not respond to requests for an interview. At trial, Kestner’s attorneys argued that he was a well-intentioned businessman who wanted to run pain clinics that offered more than just pills. He is scheduled to be sentenced on April 21 in a federal court in Nashville.
According to the transcript of Kestner’s trial, Shaw and three other former patients testified that Pain MD’s injections did not ease their pain and sometimes made it worse. The patients said they tolerated the shots only so Pain MD wouldn’t cut off their prescriptions, without which they might have spiraled into withdrawal.
“They told me that if I didn’t take the shots — because I said they didn’t help — I would not get my medication,” testified Patricia McNeil, a former patient in Tennessee, according to the trial transcript. “I took the shots to get my medication.”
In her interview with KFF Health News, Shaw said that often she would arrive at the Pain MD clinic walking with a cane but would leave in a wheelchair because the injections left her in too much pain to walk.
“That was the pain clinic that was supposed to be helping me,” Shaw said in her interview. “I would come home crying. It just felt like they were using me.”
‘Not Actually Injections Into Tendons at All’
Pain MD, which sometimes operated under the name Mid-South Pain Management, ran as many as 20 clinics in Tennessee, Virginia, and North Carolina throughout much of the 2010s. Some clinics averaged more than 12 injections per patient each month, and at least two patients each received more than 500 shots in total, according to federal court documents.
All those injections added up. According to Medicare data filed in federal court, Pain MD and Mid-South Pain Management billed Medicare for more than 290,000 “tendon origin injections” from January 2010 to May 2018, which is about seven times that of any other Medicare biller in the U.S. over the same period.
Tens of thousands of additional injections were billed to Medicaid and Tricare during those same years, according to federal court documents. Pain MD billed these government programs for about $111 per injection and collected more than $5 million from the government for the shots, according to the court documents.
More injections were billed to private insurance too. Christy Wallace, an audit manager for BlueCross BlueShield of Tennessee, testified that Pain MD billed the insurance company about $40 million for more than 380,000 injections from January 2010 to March 2013. BlueCross paid out about $7 million before it cut off Pain MD, Wallace said.
These kinds of enormous billing allegations are not uncommon in health care fraud cases, in which fraudsters sometimes find a legitimate treatment that insurance will pay for and then overuse it to the point of absurdity, said Don Cochran, a former U.S. attorney for the Middle District of Tennessee.
Tennessee alone has seen fraud allegations for unnecessary billing of urine testing, skin creams, and other injections in just the past decade. Federal authorities have also investigated an alleged fraud scheme involving a Tennessee company and hundreds of thousands of catheters billed to Medicare, according to The Washington Post, citing anonymous sources.
Cochran said the Pain MD case felt especially “nefarious” because it used opioids to make patients play along.
“A scheme where you get Medicare or Medicaid money to provide a medically unnecessary treatment is always going to be out there,” Cochran said. “The opioid piece just gives you a universe of compliant people who are not going to question what you are doing.”
“It was only opioids that made those folks come back,” he said.
The allegations against Pain MD became public in 2018 when Cochran and the Department of Justice filed a civil lawsuit against the company, Kestner, and several associated clinics, alleging that Pain MD defrauded taxpayers and government insurance programs by billing for “tendon origin injections” that were “not actually injections into tendons at all.”
Kestner, Pain MD, and several associated clinics have each denied all allegations in that lawsuit, which is ongoing.Scott Kreiner, an expert on spine care and pain medicine who testified at Kestner’s criminal trial, said that true tendon origin injections (or TOIs) typically are used to treat inflamed joints, like the condition known as “tennis elbow,” by injecting steroids or platelet-rich plasma into a tendon. Kreiner said most patients need only one shot at a time, according to the transcript.
But Pain MD made repeated injections into patients’ backs that contained only lidocaine or Marcaine, which are anesthetic medications that cause numbness for mere hours, Kreiner testified. Pain MD also used needles that were often too short to reach back tendons, Kreiner said, and there was no imaging technology used to aim the needle anyway. Kreiner said he didn’t find any injections in Pain MD’s records that appeared medically necessary, and even if they had been, no one could need so many.
“I simply cannot fathom a scenario where the sheer quantity of TOIs that I observed in the patient records would ever be medically necessary,” Kreiner said, according to the trial transcript. “This is not even a close call.”
Jonathan White, a physician assistant who administered injections at Pain MD and trained other employees to do so, then later testified against Kestner as part of a plea deal, said at trial that he believed Pain MD’s injection technique was based on a “cadaveric investigation.”
According to the trial transcript, White said that while working at Pain MD he realized he could find no medical research that supported performing tendon origin injections on patients’ backs instead of their joints. When he asked if Pain MD had any such research, White said, an employee responded with a two-paragraph letter from a Tennessee anatomy professor — not a medical doctor — that said it was possible to reach the region of back tendons in a cadaver by injecting “within two fingerbreadths” of the spine. This process was “exactly the procedure” that was taught at Pain MD, White said.
During his own testimony, Kreiner said it was “potentially dangerous” to inject a patient as described in the letter, which should not have been used to justify medical care.
“This was done on a dead person,” Kreiner said, according to the trial transcript. “So the letter says nothing about how effective the treatment is.”
Over-Injecting ‘Killed My Hand’
Pain MD collapsed into bankruptcy in 2019, leaving some patients unable to get new prescriptions because their medical records were stuck in locked storage units, according to federal court records.
At the time, Pain MD defended the injections and its practice of discharging patients who declined the shots. When a former patient publicly accused the company of treating his back “like a dartboard,” Pain MD filed a defamation lawsuit, then dropped the suit about a month later.
“These are interventional clinics, so that’s what they offer,” Jay Bowen, a then-attorney for Pain MD, told The Tennessean newspaper in 2019. “If you don’t want to consider acupuncture, don’t go to an acupuncture clinic. If you don’t want to buy shoes, don’t go to a shoe store.”
Kestner’s trial told another story. According to the trial transcript, eight former Pain MD medical providers testified that the driving force behind Pain MD’s injections was Kestner himself, who is not a medical professional and yet regularly pressured employees to give more shots.
One nurse practitioner testified that she received emails “every single workday” pushing for more injections. Others said Kestner openly ranked employees by their injection rates, and implied that those who ranked low might be fired.
“He told me that if I had to feed my family based on my productivity, that they would starve,” testified Amanda Fryer, a nurse practitioner who was not charged with any crime.
Brian Richey, a former Pain MD nurse practitioner who at times led the company’s injection rankings, and has since taken a plea deal that required him to testify in court, said at the trial that he “performed so many injections” that his hand became chronically inflamed and required surgery.
“‘Over injecting killed my hand,’” Richey said on the witness stand, reading a text message he sent to another Pain MD employee in 2017, according to the trial transcript. “‘I was in so much pain Injecting people that didnt want it but took it to stay a patient.’”
“Why would they want to stay there?” a prosecutor asked.
“To keep getting their narcotics,” Richey responded, according to the trial transcript.
Throughout the trial, defense attorney Peter Strianse argued that Pain MD’s focus on injections was a result of Kestner’s “obsession” with ensuring that the company “would never be called a pill mill.”
Strianse said that Kestner “stayed up at night worrying” about patients coming to clinics only to get opioid prescriptions, so he pushed his employees to administer injections, too.
“Employers motivating employees is not a crime,” Strianse said at closing arguments, according to the court transcript. “We get pushed every day to perform. It’s not fraud; it’s a fact of life.”
Prosecutors insisted that this defense rang hollow. During the trial, former employees had testified that most patients’ opioid dosages remained steady or increased while at Pain MD, and that the clinics did not taper off the painkillers no matter how many injections were given.
“Giving them injections does not fix the pill mill problem,” federal prosecutor Katherine Payerle said during closing arguments, according to the trial transcript. “The way to fix being a pill mill is to stop giving the drugs or taper the drugs.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: