Green Coffee Bean Extract: Coffee Benefits Without The Coffee?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Coffee is, on balance, very good for the health in moderation. We wrote about it here:
The Bitter Truth About Coffee (or is it?)
Some quick facts before moving on:
- Coffee is the world’s biggest source of antioxidants
- 65% reduced risk of Alzheimer’s for coffee-drinkers
- 67% reduced risk of type 2 diabetes for coffee-drinkers
- 43% reduced risk of liver cancer for coffee-drinkers
- 53% reduced suicide risk for coffee-drinkers
Those are some compelling statistics!
But what about the caffeine content?
Assuming one doesn’t have a caffeine sensitivity, caffeine is also healthy in moderation—but it is easy to accidentally become dependent on it, so it can be good to take a “tolerance break” once in a while, and then reintroduce it with more modest moderation:
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
We also, for that matter, have discussed its impact on the gut:
Coffee & Your Gut ← surprise, it’s a positive impact
What if I don’t like coffee?
We suspect that, having seen the title of this article, you know what the answer’s going to be here:
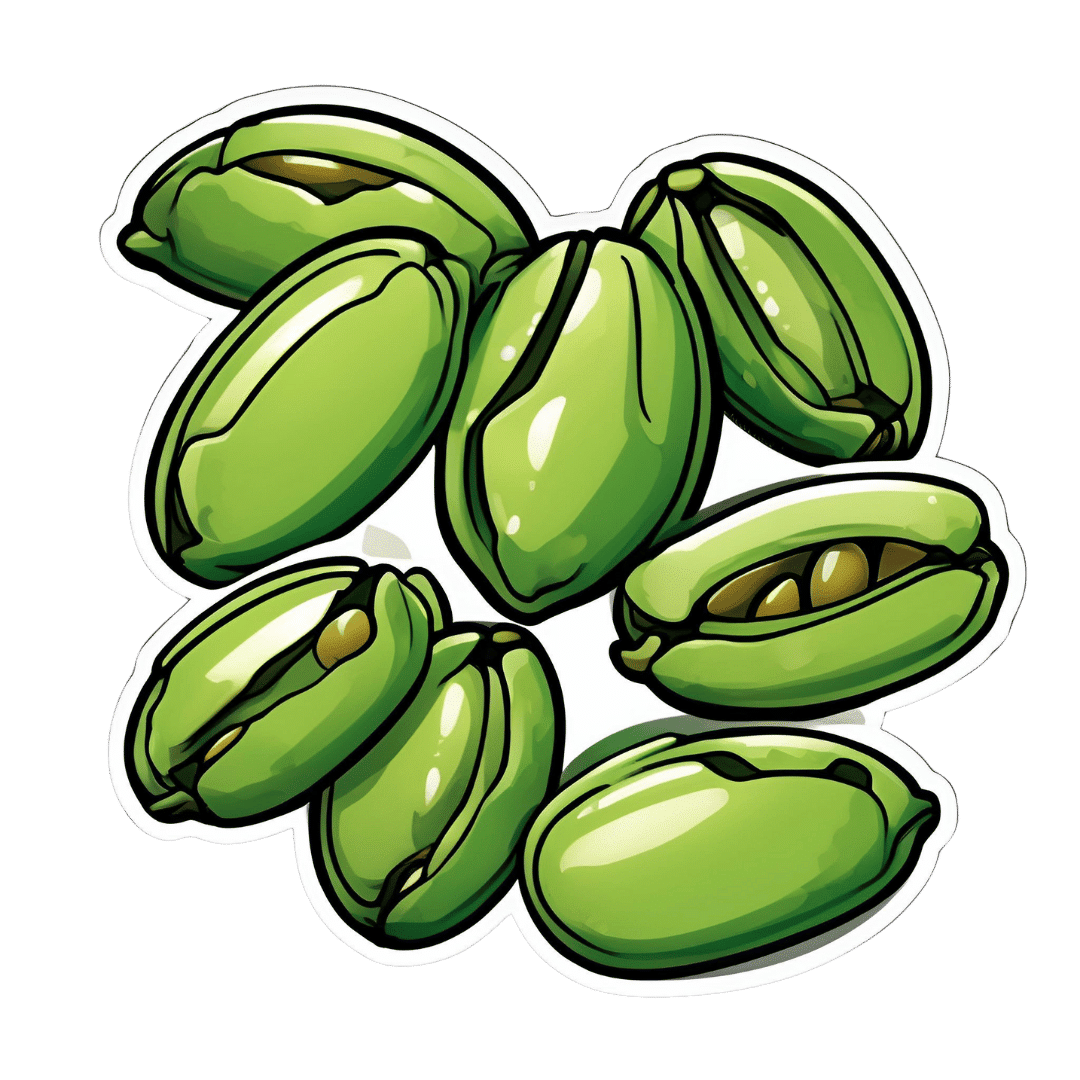
Green coffee bean extract is the extract from green (i.e. unroasted) coffee beans. It has one or two advantages over drinking coffee:
- For those who do not like drinking coffee, this supplement sidesteps that neatly
- Roasting coffee beans destroys a lot (sometimes almost all; it depends on the temperature and duration) of their chlorogenic acid, a highly beneficial polyphenol; using unroasted (i.e. green) coffee beans avoids that
See: Role of roasting conditions in the level of chlorogenic acid content in coffee beans
All about GCE and CGA
That’s “green coffee extract” and “chlorogenic acid”, respectively, bearing in mind that the latter is found generously in the former.
As to what it does:
❝CGA is an important and biologically active dietary polyphenol, playing several important and therapeutic roles such as antioxidant activity, antibacterial, hepatoprotective, cardioprotective, anti-inflammatory, antipyretic, neuroprotective, anti-obesity, antiviral, anti-microbial, anti-hypertension, free radicals scavenger and a central nervous system (CNS) stimulator. Furthermore, CGA causes hepatoprotective effects.❞
👆 Those are the things we know for sure that it does. And it may do even more things:
❝In addition, it has been found that CGA could modulate lipid metabolism and glucose in both genetically and healthy metabolic related disorders. It is speculated that CGA can perform crucial roles in lipid and glucose metabolism regulation and thus help to treat many disorders such as hepatic steatosis, cardiovascular disease, diabetes, and obesity as well.❞
Read in full: Chlorogenic acid (CGA): A pharmacological review and call for further research
About lipid metabolism…
- Green coffee extract supplementation significantly reduces serum total cholesterol levels.
- Green coffee extract supplementation significantly reduces serum LDL (“bad” cholesterol) levels.
- Increases in HDL (“good” cholesterol) after green coffee bean extract consumption are significant in green coffee bean extract dosages ≥400mg/day.
About blood glucose and insulin…
- Green coffee extract supplementation significantly improved fasting blood sugar levels
- Green coffee extract supplementation at ≥400 mg/day significantly lowered postprandial insulin levels (that’s good)
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Passion Fruit vs Persimmon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing passion fruit to persimmon, we picked the passion fruit.
Why?
You may be wondering: “what is this fruit passionate about?” and the answer is: delivering nutrients of many kinds!
Looking at the macros first, passion fruit has a little more protein and a lot more fiber, while persimmon has more carbs. This means that while persimmon’s glycemic index isn’t bad, passion fruit’s glycemic index is a lot lower.
In terms of vitamins, passion fruit has a lot more of vitamins A, B2, B3, B6, B9, E, K, and choline, while persimmon has more vitamin C. For the record passion fruit is also a good source of vitamin C, with a cup of passion fruit already giving a day’s daily dose of vitamin C, but persimmon gives twice that. Still, that’s a 8:1 win for passion fruit.
When it comes to minerals, passion fruit has more copper, magnesium, phosphorus, potassium, selenium, and zinc, while persimmon has more calcium and iron, meaning a 6:2 win for passion fruit.
Adding up the three convincing individual victories shows a clear overall win for passion fruit.
Enjoy (passionately, even)!
Want to learn more?
You might like to read:
- Glycemic Index vs Glycemic Load vs Insulin Index
- Which Sugars Are Healthier, And Which Are Just The Same?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Take care!
Share This Post
-
Just One Thing – by Dr. Michael Mosley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a collection of easy-to-implement changes that have good science behind them to show how they can benefit us. Some things are obvious (e.g: drink water); others, less so (e.g: sing, to reduce inflammation).
The book is divided thematically into times of the day, though in many cases it’s not a hard rule that a thing needs to be done at a certain time. Others are, like a cold shower in the morning and hot bath before bed—you might not want to switch those around!
The style is very pop-science, and does not have in-line citations for claims, but it does have a bibliography in the bag organized by each “one thing”, e.g. it might say “get some houseplants” and then list a number of references supporting that, with links to the studies showing how that helps. For those with the paper version, don’t worry, you can copy the URL from the book into your browser and see it that way. In any case, there are 2–6 scientific references for each claim, which is very respectable for a pop-sci book.
Bottom line: if you’re looking for evidence-based “one little thing” changes that can make a big difference, this book has lots!
Click here to check out Just One Thing, and improve your life!
Share This Post
-
Brain Food? The Eyes Have It!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Brain Food? The Eyes Have It!
This is Dr. Michael Greger, M.D. FACLM, of “Dr. Greger’s Daily Dozen” and “How Not To Die” fame, and he wants us to protect our brains (and while we’re at it, our eyesight).
And the secret is…
Lutein.
This is a carotenoid, which is super important for the eyes and brain. Not to be confused with carrots, which despite the name are usually not a good source of carotenoids!
They do however contain lots of beta-carotene, a form of vitamin A, but that (and the famous WW2-era myth born of deliberate disinformation by the British government) isn’t what we’re covering today.
We say “eyes and brain” but really, the eyes are just an extension of the brain in any case.
Pedantry aside, what Dr. Greger wants you to know about lutein is how important it is for the protection of your brain/eyes, both against cognitive decline and against age-related macular degeneration (the most common cause of eyesight loss in old age).
Important take-away info:
- Two things that hasten brain aging are inflammation and oxidative stress. Antioxidant and anti-inflammatory foods mitigate those.
- Researchers investigated eight different dietary antioxidants, including vitamins A and E. Only lutein was “significantly related to better cognition”.
- The macula in the middle of our retina is packed with lutein, and levels in the retina correspond to levels in the rest of our brain.
- Alzheimer’s patients have significantly less lutein in their eyes and in their blood, and a higher occurrence of macular degeneration.
- Dark green leafy vegetables are lutein superstars. A half cup of kale has 50 times more lutein than an egg.
Want to know more about the Dr. Greger’s Daily Dozen approach to health?
See the Website / Get the App (Android & iOS) / Get the Science Book / Get the Cookbook!
Share This Post
Related Posts
-
What’s the difference between a heart attack and cardiac arrest? One’s about plumbing, the other wiring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In July 2023, rising US basketball star Bronny James collapsed on the court during practice and was sent to hospital. The 18-year-old athlete, son of famous LA Lakers’ veteran LeBron James, had experienced a cardiac arrest.
Many media outlets incorrectly referred to the event as a “heart attack” or used the terms interchangeably.
A cardiac arrest and a heart attack are distinct yet overlapping concepts associated with the heart.
With some background in how the heart works, we can see how they differ and how they’re related.
Explode/Shutterstock Understanding the heart
The heart is a muscle that contracts to work as a pump. When it contracts it pushes blood – containing oxygen and nutrients – to all the tissues of our body.
For the heart muscle to work effectively as a pump, it needs to be fed its own blood supply, delivered by the coronary arteries. If these arteries are blocked, the heart muscle doesn’t get the blood it needs.
This can cause the heart muscle to become injured or die, and results in the heart not pumping properly.
Heart attack or cardiac arrest?
Simply put, a heart attack, technically known as a myocardial infarction, describes injury to, or death of, the heart muscle.
A cardiac arrest, sometimes called a sudden cardiac arrest, is when the heart stops beating, or put another way, stops working as an effective pump.
In other words, both relate to the heart not working as it should, but for different reasons. As we’ll see later, one can lead to the other.
Why do they happen? Who’s at risk?
Heart attacks typically result from blockages in the coronary arteries. Sometimes this is called coronary artery disease, but in Australia, we tend to refer to it as ischaemic heart disease.
The underlying cause in about 75% of people is a process called atherosclerosis. This is where fatty and fibrous tissue build up in the walls of the coronary arteries, forming a plaque. The plaque can block the blood vessel or, in some instances, lead to the formation of a blood clot.
Atherosclerosis is a long-term, stealthy process, with a number of risk factors that can sneak up on anyone. High blood pressure, high cholesterol, diet, diabetes, stress, and your genes have all been implicated in this plaque-building process.
Other causes of heart attacks include spasms of the coronary arteries (causing them to constrict), chest trauma, or anything else that reduces blood flow to the heart muscle.
Regardless of the cause, blocking or reducing the flow of blood through these pipes can result in the heart muscle not receiving enough oxygen and nutrients. So cells in the heart muscle can be injured or die.
Here’s a simple way to remember the difference. Author provided But a cardiac arrest is the result of heartbeat irregularities, making it harder for the heart to pump blood effectively around the body. These heartbeat irregularities are generally due to electrical malfunctions in the heart. There are four distinct types:
- ventricular tachycardia: a rapid and abnormal heart rhythm in which the heartbeat is more than 100 beats per minute (normal adult, resting heart rate is generally 60-90 beats per minute). This fast heart rate prevents the heart from filling with blood and thus pumping adequately
- ventricular fibrillation: instead of regular beats, the heart quivers or “fibrillates”, resembling a bag of worms, resulting in an irregular heartbeat greater than 300 beats per minute
- pulseless electrical activity: arises when the heart muscle fails to generate sufficient pumping force after electrical stimulation, resulting in no pulse
- asystole: the classic flat-line heart rhythm you see in movies, indicating no electrical activity in the heart.
Remember this flat-line rhythm from the movies? It’s asystole, when there’s no electrical activity in the heart. Kateryna Kon/Shutterstock Cardiac arrest can arise from numerous underlying conditions, both heart-related and not, such as drowning, trauma, asphyxia, electrical shock and drug overdose. James’ cardiac arrest was attributed to a congenital heart defect, a heart condition he was born with.
But among the many causes of a cardiac arrest, ischaemic heart disease, such as a heart attack, stands out as the most common cause, accounting for 70% of all cases.
So how can a heart attack cause a cardiac arrest? You’ll remember that during a heart attack, heart muscle can be damaged or parts of it may die. This damaged or dead tissue can disrupt the heart’s ability to conduct electrical signals, increasing the risk of developing arrhythmias, possibly causing a cardiac arrest.
So while a heart attack is a common cause of cardiac arrest, a cardiac arrest generally does not cause a heart attack.
What do they look like?
Because a cardiac arrest results in the sudden loss of effective heart pumping, the most common signs and symptoms are a sudden loss of consciousness, absence of pulse or heartbeat, stopping of breathing, and pale or blue-tinged skin.
But the common signs and symptoms of a heart attack include chest pain or discomfort, which can show up in other regions of the body such as the arms, back, neck, jaw, or stomach. Also frequent are shortness of breath, nausea, light-headedness, looking pale, and sweating.
What’s the take-home message?
While both heart attack and cardiac arrest are disorders related to the heart, they differ in their mechanisms and outcomes.
A heart attack is like a blockage in the plumbing supplying water to a house. But a cardiac arrest is like an electrical malfunction in the house’s wiring.
Despite their different nature both conditions can have severe consequences and require immediate medical attention.
Michael Todorovic, Associate Professor of Medicine, Bond University and Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Two Things You Can Do To Improve Stroke Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
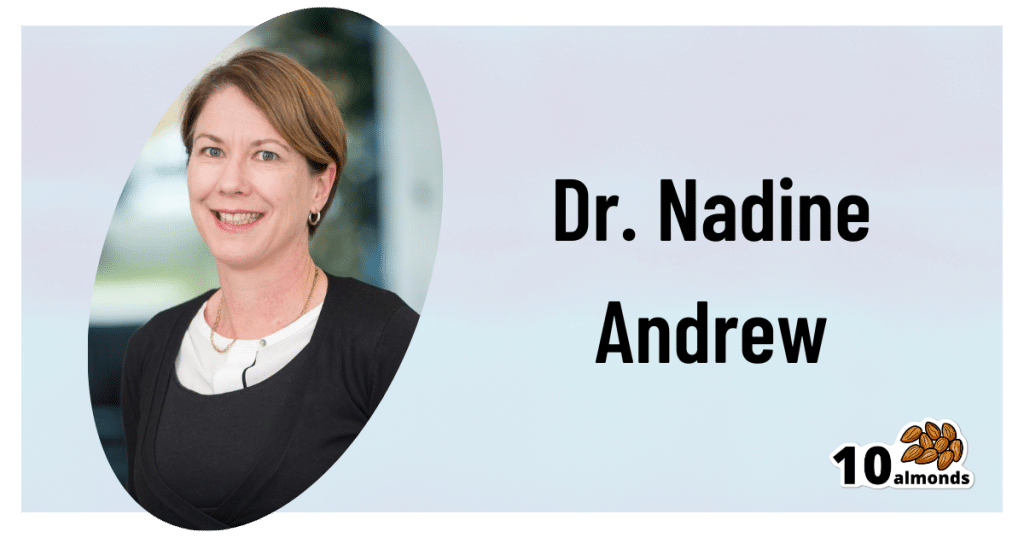
Dr. Andrew’s Stroke Survival Guide
This is Dr. Nadine Andrew. She’s a Senior Research Fellow in the Department of Medicine at Monash University. She’s the Research Data Lead for the National Center of Healthy Aging. She is lead investigator on the NHMRC-funded PRECISE project… The most comprehensive stroke data linkage study to date! In short, she knows her stuff.
We’ve talked before about how sample size is important when it comes to scientific studies. It’s frustrating; sometimes we see what looks like a great study until we notice it has a sample size of 17 or something.
Dr. Andrew didn’t mess around in this regard, and the 12,386 participants in her Australian study of stroke patients provided a huge amount of data!
With a 95% confidence interval because of the huge dataset, she found that there was one factor that reduced mortality by 26%.
And the difference was…
Whether or not patients had a chronic disease management plan set up with their GP (General Practitioner, or “family doctor”, in US terms), after their initial stroke treatment.
45% of patients had this; the other 55% did not, so again the sample size was big for both groups.
Why this is important:
After a stroke, often a patient is discharged as early as it seems safe to do so, and there’s a common view that “it just takes time” and “now we wait”. After all, no medical technology we currently have can outright repair that damage—the body must repair itself! Medications—while critical*—can only support that and help avoid recurrence.
*How critical? VERY critical. Critical critical. Dr. Andrew found, some years previously, that greater levels of medication adherence (ie, taking the correct dose on time and not missing any) significantly improved survival outcomes. No surprise, right? But what may surprise is that this held true even for patients with near-perfect adherence. In other words: miss a dose at your peril. It’s that important.
But, as Dr. Andrew’s critical research shows, that’s no reason to simply prescribe ongoing meds and otherwise cut a patient loose… or, if you or a loved one are the patient, to allow yourself/them to be left without a doctor’s ongoing active support in the form of a chronic disease management plan.
What does a chronic disease management plan look like?
First, what it’s not:
- “Yes yes, I’m here if you need me, just make an appointment if something changes”
- “Let’s pencil in a check-up in three months”
- Etc
What it actually looks like:
It looks like a plan. A personal care plan, built around that person’s individual needs, risks, liabilities… and potential complications.
Because who amongst us, especially at the age where strokes are more likely, has an uncomplicated medical record? There will always be comorbidities and confounding factors, so a one-size-fits-all plan will not do.
Dr. Andrew’s work took place in Australia, so she had the Australian healthcare system in mind… We know many of our subscribers are from North America and other places. But read this, and you’ll see how this could go just as much for the US or Canada:
❝The evidence shows the importance of Medicare financially supporting primary care physicians to provide structured chronic disease management after a stroke.
We also provide a strong case for the ongoing provision of these plans within a universal healthcare system. Strategies to improve uptake at the GP level could include greater financial incentives and mandates, education for patients and healthcare professionals.❞
See her groundbreaking study for yourself here!
The Bottom Line:
If you or a loved one has a stroke, be prepared to make sure you get a chronic health management plan in place. Note that if it’s you who has the stroke, you might forget this or be unable to advocate for yourself. So, we recommend to discuss this with a partner or close friend sooner rather than later!
“But I’m quite young and healthy and a stroke is very unlikely for me”
Good for you! And the median age of Dr. Andrew’s gargantuan study was 70 years. But:
- do you have older relatives? Be aware for them, too.
- strokes can happen earlier in life too! You don’t want to be an interesting statistic.
Some stroke-related quick facts:
Stroke is the No. 5 cause of death and a leading cause of disability in the U.S.
Stroke can happen to anyone—any age, any time—and everyone needs to know the warning signs.
On average, 1.9 million brain cells die every minute that a stroke goes untreated.
Stroke is an EMERGENCY. Call 911 immediately.
Early treatment leads to higher survival rates and lower disability rates. Calling 911 lets first responders start treatment on someone experiencing stroke symptoms before arriving at the hospital.
Source: https://www.stroke.org/en/about-stroke
What are the warning signs for stroke?
Use the letters F.A.S.T. to spot a stroke and act quickly:
- F = Face Drooping—does one side of the face droop or is it numb? Ask the person to smile. Is the person’s smile uneven?
- A = Arm Weakness—is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
- S = Speech Difficulty—is speech slurred?
- T = Time to call 911
Source: https://www.stroke.org/en/about-stroke/stroke-symptoms
Last but not least, while we’re sharing resources:
Download the PDF Checklist: 8 Ways To Help Prevent a Second Stroke
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Say That Again: Using Hearing Aids Can Be Frustrating for Older Adults, but Necessary
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It was an every-other-day routine, full of frustration.
Every time my husband called his father, who was 94 when he died in 2022, he’d wait for his dad to find his hearing aids and put them in before they started talking.
Even then, my father-in-law could barely hear what my husband was saying. “What?” he’d ask over and over.
Then, there were the problems my father-in-law had replacing the devices’ batteries. And the times he’d end up in the hospital, unable to understand what people were saying because his hearing aids didn’t seem to be functioning. And the times he’d drop one of the devices and be unable to find it.
How many older adults have problems of this kind?
There’s no good data about this topic, according to Nicholas Reed, an assistant professor of epidemiology at Johns Hopkins Bloomberg School of Public Health who studies hearing loss. He did a literature search when I posed the question and came up empty.
Reed co-authored the most definitive study to date of hearing issues in older Americans, published in JAMA Open Network last year. Previous studies excluded people 80 and older. But data became available when a 2021 survey by the National Health and Aging Trends Study included hearing assessments conducted at people’s homes.
The results, based on a nationally representative sample of 2,803 people 71 and older, are eye-opening. Hearing problems become pervasive with advancing age, exceeding 90% in people 85 and older, compared with 53% of 71- to 74-year-olds. Also, hearing worsens over time, with more people experiencing moderate or severe deficits once they reach or exceed age 80, compared with people in their 70s.
However, only 29% of those with hearing loss used hearing aids. Multiple studies have documented barriers that inhibit use. Such devices, which Medicare doesn’t cover, are pricey, from nearly $1,000 for a good over-the-counter set (OTC hearing aids became available in 2022) to more than $6,000 for some prescription models. In some communities, hearing evaluation services are difficult to find. Also, people often associate hearing aids with being old and feel self-conscious about wearing them. And they tend to underestimate hearing problems that develop gradually.
Barbara Weinstein, a professor of audiology at the City University of New York Graduate Center and author of the textbook “Geriatric Audiology,” added another concern to this list when I reached out to her: usability.
“Hearing aids aren’t really designed for the population that most needs to use them,” she told me. “The move to make devices smaller and more sophisticated technologically isn’t right for many people who are older.”
That’s problematic because hearing loss raises the risk of cognitive decline, dementia, falls, depression, and social isolation.
What advice do specialists in hearing health have for older adults who have a hard time using their hearing aids? Here are some thoughts they shared.
Consider larger, customized devices. Many older people, especially those with arthritis, poor fine motor skills, compromised vision, and some degree of cognitive impairment, have a hard time manipulating small hearing aids and using them properly.
Lindsay Creed, associate director of audiology practices at the American Speech-Language-Hearing Association, said about half of her older clients have “some sort of dexterity issue, whether numbness or reduced movement or tremor or a lack of coordination.” Shekinah Mast, owner of Mast Audiology Services in Seaford, Delaware, estimates nearly half of her clients have vision issues.
For clients with dexterity challenges, Creed often recommends “behind-the-ear hearing aids,” with a loop over the ear, and customized molds that fit snugly in the ear. Customized earpieces are larger than standardized models.
“The more dexterity challenges you have, the better you’ll do with a larger device and with lots of practice picking it up, orienting it, and putting it in your ear,” said Marquitta Merkison, associate director of audiology practices at ASHA.
For older people with vision issues, Mast sometimes orders hearing aids in different colors for different ears. Also, she’ll help clients set up stands at home for storing devices, chargers, and accessories so they can readily find them each time they need them.
Opt for ease of use. Instead of buying devices that require replacing tiny batteries, select a device that can be charged overnight and operate for at least a day before being recharged, recommended Thomas Powers, a consultant to the Hearing Industries Association. These are now widely available.
People who are comfortable using a smartphone should consider using a phone app to change volume and other device settings. Dave Fabry, chief hearing health officer at Starkey, a major hearing aid manufacturer, said he has patients in their 80s and 90s “who’ve found that being able to hold a phone and use larger visible controls is easier than manipulating the hearing aid.”
If that’s too difficult, try a remote control. GN ReSound, another major manufacturer, has designed one with two large buttons that activate the volume control and programming for its hearing aids, said Megan Quilter, the company’s lead audiologist for research and development.
Check out accessories. Say you’re having trouble hearing other people in restaurants. You can ask the person across the table to clip a microphone to his shirt or put the mike in the center of the table. (The hearing aids will need to be programmed to allow the sound to be streamed to your ears.)
Another low-tech option: a hearing aid clip that connects to a piece of clothing to prevent a device from falling to the floor if it becomes dislodged from the ear.
Wear your hearing aids all day. “The No. 1 thing I hear from older adults is they think they don’t need to put on their hearing aids when they’re at home in a quiet environment,” said Erika Shakespeare, who owns Audiology and Hearing Aid Associates in La Grande, Oregon.
That’s based on a misunderstanding. Our brains need regular, not occasional, stimulation from our environments to optimize hearing, Shakespeare explained. This includes noises in seemingly quiet environments, such as the whoosh of a fan, the creak of a floor, or the wind’s wail outside a window.
“If the only time you wear hearing aids is when you think you need them, your brain doesn’t know how to process all those sounds,” she told me. Her rule of thumb: “Wear hearing aids all your waking hours.”
Consult a hearing professional. Everyone’s needs are different, so it’s a good idea to seek out an audiologist or hearing specialist who, for a fee, can provide guidance.
“Most older people are not going to know what they need” and what options exist without professional assistance, said Virginia Ramachandran, the head of audiology at Oticon, a major hearing aid manufacturer, and a past president of the American Academy of Audiology.
Her advice to older adults: Be “really open” about your challenges.
If you can’t afford hearing aids, ask a hearing professional for an appointment to go over features you should look for in over-the-counter devices. Make it clear you want the appointment to be about your needs, not a sales pitch, Reed said. Audiology practices don’t routinely offer this kind of service, but there’s good reason to ask since Medicare started covering once-a-year audiologist consultations last year.
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: