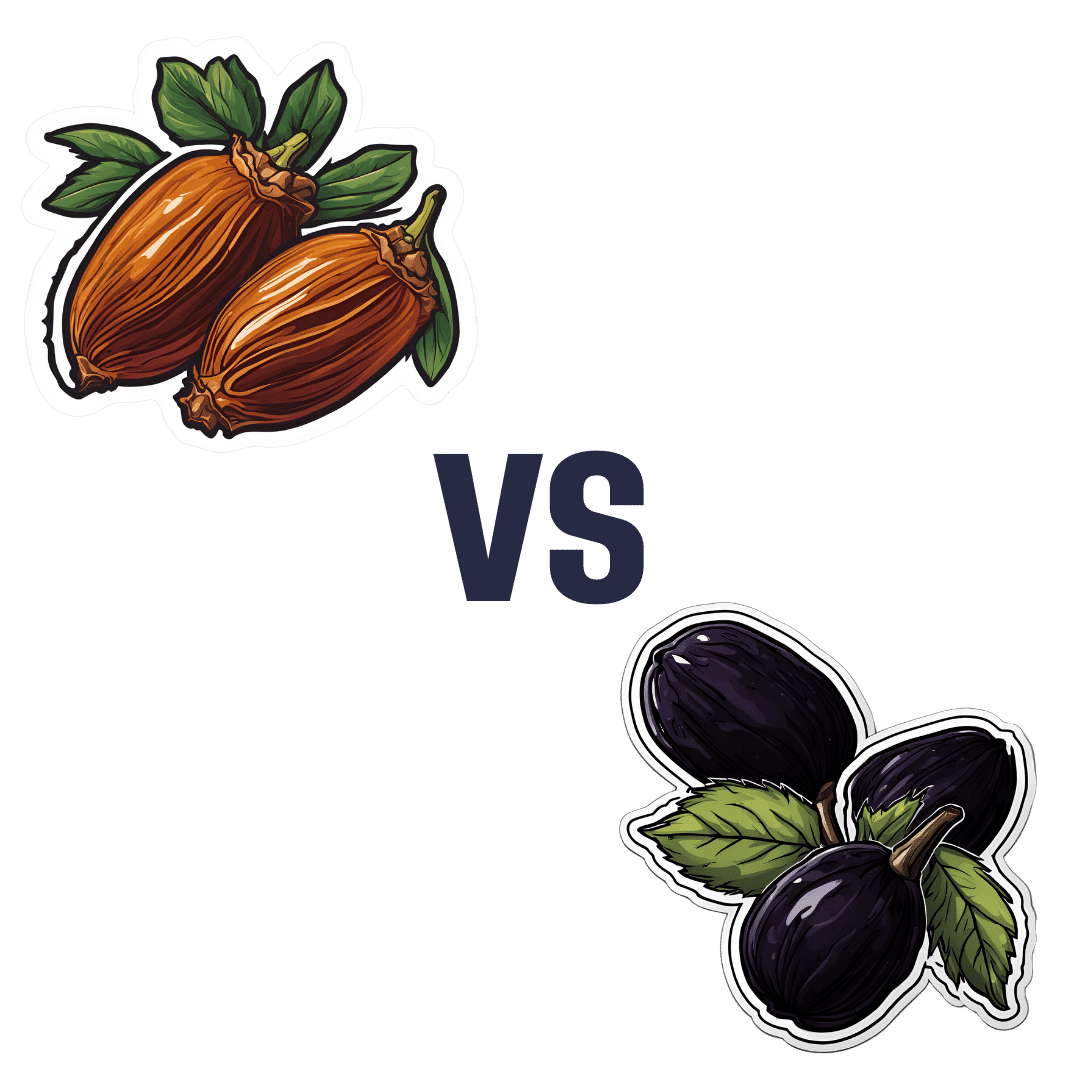
Dates vs Prunes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to prunes, we picked the prunes.
Why?
First let’s note: we’re listing the second fruit here as “prunes” rather than “plums”, since prunes are dehydrated plums, and it makes more sense to compare the dried fruit to dates which are invariably dried too. Otherwise, the water weight of plums would unfairly throw out the nutrient proportions per 100g (indeed, upon looking up numbers, dates would overwhelmingly beat plums easily in the category of pretty much every nutrient).
So let’s look at the fairer comparison:
In terms of macros, dates have a little more protein, carbohydrate, and fiber. This is because while both are dried, prunes are usually sold with more water remaining than dates; indeed, per 100g prunes still have 30g water weight to dates’ 20g water weight. This makes everything close, but we are going to call this category a nominal win for dates. Mind you, hydration is still good, but please do not rely on dried fruit for your hydration!
When it comes to vitamins, dates have more of vitamins B5 and B9, while prunes have more of vitamins A, B2, B3, B6, C, E, K, and choline. A clear win for prunes here.
In the category of minerals, it’s a similar story: dates have more iron, magnesium, and selenium, while prunes have more calcium, copper, manganese, phosphorus, potassium, and zinc. Another win for prunes.
In short, enjoy either or both, but prunes win on overall nutritional density!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Choco-Banoffee Ice Cream
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chocolate, banana, and coffee—quite a threesome, whether for breakfast or dessert, and this is healthy enough for breakfast while being decadent enough for dessert! With no dairy or added sugar, and lots of antioxidants, this is a healthy way to start or end your day.
You will need
- 3 bananas
- 2 tbsp cocoa powder, no additives
- 2 shots espresso, chilled
- 1 tsp vanilla extract
- On standby: milk of your choice—we recommend almond or hazelnut
Method
(we suggest you read everything at least once before doing anything)
1) Peel, slice, and freeze the bananas (let them freeze for at least 2–3 hours)
2) Blend the ingredients, except the milk. Add milk as necessary if the mixture is too thick to blend. Be careful not to add too much at once though, or it will become less of an ice cream and more of a milkshake!
3) Scoop into a sundae glass to serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Plant Milk?
- The Bitter Truth About Coffee (or is it?)
- Cacao vs Carob – Which is Healthier?
- Apples vs Bananas – Which is Healthier?
- Which Sugars Are Healthier, And Which Are Just The Same?
- Tasty Polyphenols
Take care!
Share This Post
-
Forget Ringing the Button for the Nurse. Patients Now Stay Connected by Wearing One.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HOUSTON — Patients admitted to Houston Methodist Hospital get a monitoring device about the size of a half-dollar affixed to their chest — and an unwitting role in the expanding use of artificial intelligence in health care.
The slender, battery-powered gadget, called a BioButton, records vital signs including heart and breathing rates, then wirelessly sends the readings to nurses sitting in a 24-hour control room elsewhere in the hospital or in their homes. The device’s software uses AI to analyze the voluminous data and detect signs a patient’s condition is deteriorating.
Hospital officials say the BioButton has improved care and reduced the workload of bedside nurses since its rollout last year.
“Because we catch things earlier, patients are doing better, as we don’t have to wait for the bedside team to notice if something is going wrong,” said Sarah Pletcher, system vice president at Houston Methodist.
But some nurses fear the technology could wind up replacing them rather than supporting them — and harming patients. Houston Methodist, one of dozens of U.S. hospitals to employ the device, is the first to use the BioButton to monitor all patients except those in intensive care, Pletcher said.
“The hype around a lot of these devices is they provide care at scale for less labor costs,” said Michelle Mahon, a registered nurse and an assistant director of National Nurses United, the profession’s largest U.S. union. “This is a trend that we find disturbing,” she said.
The rollout of BioButton is among the latest examples of hospitals deploying technology to improve efficiency and address a decades-old nursing shortage. But that transition has raised its own concerns, including about the device’s use of AI; polls show the public is wary of health providers relying on it for patient care.
In December 2022 the FDA cleared the BioButton for use in adult patients who are not in critical care. It is one of many AI tools now used by hospitals for tasks like reading diagnostic imaging results.
In 2023, President Joe Biden directed the Department of Health and Human Services to develop a plan to regulate AI in hospitals, including by collecting reports of patients harmed by its use.
The leader of BioIntelliSense, which developed the BioButton, said its device is a huge advance compared with nurses walking into a room every few hours to measure vital signs. “With AI, you now move from ‘I wonder why this patient crashed’ to ‘I can see this crash coming before it happens and intervene appropriately,’” said James Mault, CEO of the Golden, Colorado-based company.
The BioButton stays on the skin with an adhesive, is waterproof, and has up to a 30-day battery life. The company says the device — which allows providers to quickly notice deteriorating health by recording more than 1,000 measurements a day per patient — has been used on more than 80,000 hospital patients nationwide in the past year.
Hospitals pay BioIntelliSense an annual subscription fee for the devices and software.
Houston Methodist officials would not reveal how much the hospital pays for the technology, though Pletcher said it equates to less than a cup of coffee a day per patient.
For a hospital system that treats thousands of patients at a time — Houston Methodist has 2,653 non-ICU beds at its eight Houston-area hospitals — such an investment could still translate to millions of dollars a year.
Hospital officials say they have not made any changes in nurse staffing and have no plans to because of implementing the BioButton.
Inside the hospital’s control center for virtual monitoring on a recent morning, about 15 nurses and technicians dressed in scrubs sat in front of large monitors showing the health status of hundreds of patients they were assigned to monitor.
A red checkmark next to a patient’s name signaled the AI software had found readings trending outside normal. Staff members could click into a patient’s medical record, showing patients’ vital signs over time and other medical history. These virtual nurses, if you will, could contact nurses on the floor by phone or email, or even dial directly into the patient’s room via video call.
Nutanben Gandhi, a technician who was watching 446 patients on her monitor that morning, said that when she gets an alert, she looks at the patient’s health record to see if the anomaly can be easily explained by something in the patient’s condition or if she needs to contact nurses on the patient’s floor.
Oftentimes an alert can be easily dismissed. But identifying signs of deteriorating health can be tough, said Steve Klahn, Houston Methodist’s clinical director of virtual medicine.
“We are looking for a needle in a haystack,” he said.
Donald Eustes, 65, was admitted to Houston Methodist in March for prostate cancer treatment and has since been treated for a stroke. He is happy to wear the BioButton.
“You never know what can happen here, and having an extra set of eyes looking at you is a good thing,” he said from his hospital bed. After being told the device uses AI, the Montgomery, Texas, man said he has no problem with its helping his clinical team. “This sounds like a good use of artificial intelligence.”
Patients and nurses alike benefit from remote monitoring like the BioButton, said Pletcher of Houston Methodist.
The hospital has placed small cameras and microphones inside all patient rooms enabling nurses outside to communicate with patients and perform tasks such as helping with patient admissions and discharge instructions. Patients can include family members on the remote calls with nurses or a doctor, she said.
Virtual technology frees up on-duty nurses to provide more hands-on help, such as starting an intravenous line, Pletcher said. With the BioButton, nurses can wait to take routine vital signs every eight hours instead of every four, she said.
Pletcher said the device reduces nurses’ stress in monitoring patients and allows some to work more flexible hours because virtual care can be done from home rather than coming to the hospital. Ultimately it helps retain nurses, not drive them away, she said.
Sheeba Roy, a nurse manager at Houston Methodist, said some members of the nursing staff were nervous about relying on the device and not checking patients’ vital signs as often themselves. But testing has shown the device provides accurate information.
“After we implemented it, the staff loves it,” Roy said.
Serena Bumpus, chief executive officer of the Texas Nurses Association, said her concern with any technology is that it can be more burdensome on nurses and take away time with patients.
“We have to be hypervigilant in ensuring that we are not leaning on this to replace the ability of nurses to critically think and assess patients and validate what this device is telling us is true,” Bumpus said.
Houston Methodist this year plans to send the BioButton home with patients so the hospital can better track their progress in the weeks after discharge, measuring the quality of their sleep and checking their gait.
“We are not going to need less nurses in health care, but we have limited resources and we have to use those as thoughtfully as we can,” Pletcher said. “Looking at projected demand and seeing the supply we have coming, we will not have enough to meet demand, so anything we can do to give time back to nurses is a good thing.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Breast Milk’s Benefits That Are (So Far) Not Replicable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Simply The Breast 🎶
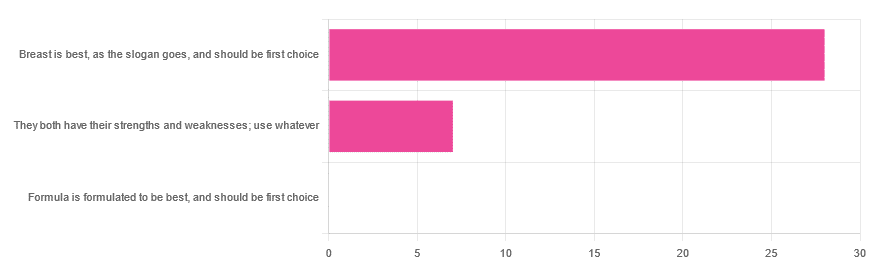
In Wednesday’s newsletter, we asked you for your opinion on breast vs formula milk (for babies!), and got the above-depicted, below-described, set of responses:
- 80% said “Breast is best, as the slogan goes, and should be first choice”
- 20% said “They both have their strengths and weaknesses; use whatever”
- 0% said “Formula is formulated to be best, and should be first choice”
That’s the first time we’ve ever had a possible poll option come back with zero votes whatsoever! It seems this topic is relatively uncontentious amongst our readership, so we’ll keep things brief today, but there is still a little mythbusting to be done.
So, what does the science say?
[Breast milk should be the first choice] at least for the few few weeks and months for the benefit of baby’s health as breast milk has protective factors formula does not: True or False?
True! The wording here was taken from one of our readers’ responses, by the way (thank you, Robin). There are a good number of those protective factors, the most well-known of which is passing on immune cells and cell-like things; in other words, immune-related information being passed from parent* to child.
*usually the mother, though in principle it could be someone else and in practice sometimes it is; the only real requirements are that the other person be healthy, lactating, and willing.
As for immune benefits, see for example:
Perspectives on Immunoglobulins in Colostrum and Milk
And for that matter, also:
(Colostrum is simply the milk that is produced for a short period after giving birth; the composition of milk will tend to change later)
In any case, immunoglobulin A is a very important component in breast milk (colostrum and later), as well as lactoferrin (has an important antimicrobial effect and is good for the newborn’s gut), and a plethora of cytokines:
As for that about the gut, lactoferrin isn’t the only breast milk component that benefits this, by far, and there’s a lot that can’t be replicated yet:
Human Breast Milk and the Gastrointestinal Innate Immune System
As long as your infant/child is nutritiously fed, it shouldn’t matter if it comes from breast or formula: True or False?
False! Formula milk will not convey those immune benefits.
This doesn’t mean that formula-feeding is neglectful; as several people who commented mentioned*, there are many reasons a person may not be able to breastfeed, and they certainly should not be shamed for that.
*(including the reader whose words we borrowed for this True/False item; the words we quoted above were prefaced with: “Not everyone is able to breastfeed for many different reasons”)
But, while formula milk is a very good second choice, and absolutely a respectable choice if breast milk isn’t an option (or an acceptable option) for whatever reason, it still does not convey all the health benefits of breast milk—yet! The day may come when they’ll find a way to replicate the immune benefits, but today is not that day.
They both have their strengths and weaknesses: True or False?
True! But formula’s strengths are only in the category of convenience and sometimes necessity—formula conveys no health benefits that breast milk could not do better, if available.
For many babies, formula means they get to eat, when without it they would starve due to non-availability of breast milk. That’s a pretty important role!
Note also: this is a health science publication, not a philosophical publication, but we’d be remiss not to mention one thing; let’s bring it in under the umbrella of sociology:
The right to bodily autonomy continues to be the right to bodily autonomy even if somebody else wants/needs something from your body.
Therefore, while there are indeed many good reasons for not being able to breastfeed, or even just not being safely* able to breastfeed, it is at the very least this writer’s opinion that nobody should be pressed to give their reason for not breastfeeding; “no” is already a sufficient answer.
*Writer’s example re safety: when I was born, my mother was on such drugs that it would have been a very bad idea for her to breastfeed me. There are plenty of other possible reasons why it might be unsafe for someone one way or another, but “on drugs that have a clear ‘do not take while pregnant or nursing’ warning” is a relatively common one.
All that said, for those who are willing and safely able, the science is clear: breast is best.
Want to read more?
The World Health Organization has a wealth of information (including explanations of its recommendations of, where possible, exclusive breastfeeding for the first 6 months, ideally continuing some breastfeeding for the first 2 years), here:
World Health Organization | Breastfeeding
Take care!
Share This Post
Related Posts
-
An Unexpected Extra Threat Of Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If You Could Use Some Exotic Booze…
…then for health reasons, we’re going to have to say “nay”.
We’ve written about alcohol before, and needless to say, it’s not good:
(the answer is “no, we cannot”)
In fact, the WHO (which unlike government regulatory bodies setting “safe” limits on drinking, makes no profit from taxes on alcohol sales) has declared that “the only safe amount of alcohol is zero”:
WHO: No level of alcohol consumption is safe for our health
Up there, where the air is rarefied…
If you’re flying somewhere this summer (Sinatra-style flying honeymoon or otherwise), you might want to skip the alcohol even if you normally do imbibe, because:
❝…even in young and healthy individuals, the combination of alcohol intake with sleeping under hypobaric conditions poses a considerable strain on the cardiac system and might lead to exacerbation of symptoms in patients with cardiac or pulmonary diseases.
These effects might be even greater in older people; cardiovascular symptoms have a prevalence of 7% of inflight medical emergencies, with cardiac arrest causing 58% of aircraft diversions.❞
Source: Alcohol plus cabin pressure at higher altitude may threaten sleeping plane passengers’ heart health
The experiment divided subjects into a control group and a study group; the study group were placed in simulated cabin pressure as though at altitude, which found, when giving some of them two small(we’re talking the kind given on flights) alcoholic drinks:
❝The combination of alcohol and simulated cabin pressure at cruising altitude prompted a fall in SpO2 to an average of just over 85% and a compensatory increase in heart rate to an average of nearly 88 beats/minute during sleep.❞
In contrast, that was 77 beats/minute for those who had alcohol but weren’t at altitude pressure, or 64 beats/minute for those who neither drank nor were at altitude pressure.
Lots more metrics were recorded and the study is interesting to read; if you’ve ever slept on a plane and thought “that sleep was not restful at all”, then know: it wasn’t just the seat’s fault, nor the engine, nor the recycled nature of the air—it was the reduced pressure causing hypoxia (defined as having oxygen levels lower than the healthy clinical norm of 90%) and almost halving your sleep’s effectiveness for a less than 10% drop in available oxygen in the blood (the sleepers not at altitude pressure averaged 96% SpO2, compared to the 85% at altitude).
We say “almost halving” because the deep sleep phase of sleep was reduced from 84 minutes (control) to 67.5 minutes at altitude without alcohol, or 46.5 minutes at altitude with alcohol.
Again, this was a pressure cabin in a lab—so this wasn’t about the other conditions of an airplane (seats, engine hundreds of other people, etc).
Which means: in an actual airplane it’s probably even worse.
Oh, and the study participants? All healthy individuals aged 18–40, so again probably worse for those older (or younger) than that range, or with existing health conditions!
Want to know more?
You can read the study in full here:
Want to drop the drink at any altitude? Check out:
Want to get that vacation feel without alcohol? You’re going to love:
Mocktails – by Moira Clark (book)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dreams: Relevance, Meanings, Interpretations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I have a question or a suggestion for coverage in your “Psychology Sunday”. Dreams: their relevance, meanings ( if any) interpretations? I just wondered what the modern psychological opinions are about dreams in general.❞
We’ll indeed do that one of these Psychology Sundays! Thanks for suggesting it.
What we can say in advance is that there’s certainly not a single unified scientific consensus yet, but there are two or three prevailing views definitely worth covering, e.g. randomly generated, a by-product of reorganizing information in the brain, or expressions of subconscious thoughts/feelings.
There are also differences between a top-down/bottom-up approach to understanding dreaming, and efforts to tie those two together.
Watch this space!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Zuranolone: What to know about the pill for postpartum depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the year after giving birth, about one in eight people who give birth in the U.S. experience the debilitating symptoms of postpartum depression (PPD), including lack of energy and feeling sad, anxious, hopeless, and overwhelmed.
Postpartum depression is a serious, potentially life-threatening condition that can affect a person’s bond with their baby. Although it’s frequently confused with the so-called “baby blues,” it’s not the same.
The baby blues include similar, temporary symptoms that affect up to 80 percent of people who have recently given birth and usually go away within the first few weeks. PPD usually begins within the first month after giving birth and can last for months and interfere with a person’s daily life if left untreated. Thankfully, PPD is treatable and there is help available.
On August 4, the FDA approved zuranolone, branded as Zurzuvae, the first-ever oral medication to treat PPD. Until now, besides other common antidepressants, the only medication available to treat PPD specifically was the IV injection brexanolone, which is difficult to access and expensive and can only be administered in a hospital or health care setting.
Read on to find out more about zuranolone: what it is, how it works, how much it costs, and more.
What is zuranolone?
Zurzuvae is the brand name for zuranolone, an oral medication to treat postpartum depression. Developed by Sage Therapeutics in partnership with Biogen, it’s now available in the U.S. Zurzuvae is typically prescribed as two 25 mg capsules a day for 14 days. In clinical trials, the medication showed to be fast-acting, improving PPD symptoms in just three days.
How does zuranolone work?
Zuranolone is a neuroactive steroid, a type of medication that helps the neurotransmitter GABA’s receptors, which affect how the body reacts to anxiety, stress, and fear, function better.
“Zuranolone can be thought of as a synthetic version of [the neuroactive steroid] allopregnanolone,” says Dr. Katrina Furey, a reproductive psychiatrist, clinical instructor at Yale University, and co-host of the Analyze Scripts podcast. “Women with PPD have lower levels of allopregnenolone compared to women without PPD.”
How is it different from other antidepressants?
“What differentiates zuranolone from other previously available oral antidepressants is that it has a much more rapid response and a shorter course of treatment,” says Dr. Asima Ahmad, an OB-GYN, reproductive endocrinologist, and founder of Carrot Fertility.
“It can take effect as early as on day three of treatment, versus other oral antidepressants that can take up to six to 12 weeks to take full effect.”
What are Zurzuvae’s side effects?
According to the FDA, the most common side effects of Zurzuvae include dizziness, drowsiness, diarrhea, fatigue, the common cold, and urinary tract infection. Similar to other antidepressants, the medication may increase the risk of suicidal thoughts and actions in people 24 and younger. However, NPR noted that this type of labeling is required for all antidepressants, and researchers didn’t see any reports of suicidal thoughts in their trials.
“Drug trials also noted that the side effects for zuranolone were not as severe,” says Ahmad. “[There was] no sudden loss of consciousness as seen with brexanolone or weight gain and sexual dysfunction, which can be seen with other oral antidepressants.”
She adds: “Given the lower incidence of side effects and more rapid-acting onset, zuranolone could be a viable option for many,” including those looking for a treatment that offers faster symptom relief.
Can someone breastfeed while taking zuranolone?
It’s complicated. In clinical trials, participants were asked to stop breastfeeding (which, according to Furey, is common in early clinical trials).
A small study of people who were nursing while taking zuranolone found that 0.3 percent of the medication dose was passed on to breast milk, which, Furey says, is a pretty low amount of exposure for the baby. Ahmad says that “though some data suggests that the risk of harm to the baby may be low, there is still overall limited data.”
Overall, people should talk to their health care provider about the risks and benefits of breastfeeding while on the medication.
“A lot of factors will need to be weighed, such as overall health of the infant, age of the infant, etc., when making this decision,” Furey says.
How much does Zurzuvae cost?
Zurzuvae’s price before insurance coverage is $15,900 for the 14-day treatment. However, the Policy Center for Maternal Mental Health says insurance companies and Medicaid are expected to cover it because it’s the only drug of its kind.
Less than 1 percent of U.S. insurers have issued coverage guidelines so far, so it’s still unknown how much it will cost patients after insurance. Some insurers require patients to try another antidepressant first (like the more common SSRIs) before covering Zurzuvae. For uninsured and underinsured people, Sage Therapeutics said it will offer copay assistance.
The hefty price tag and potential issues with coverage may widen existing health disparities, says Ahmad. “We need to ensure that we are seeking out solutions to enable wide-scale access to all PPD treatments so that people have access to whatever treatment may work best for them.”
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: