Human Connection In An All-Too-Busy World
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us, in many ways, have more discretionary time than ever… On paper.
But rather than the 8-hour block of work of yesteryear, nowadays the things that take our time often come in a series of short bursts that punctuate our day.
This means that while in theory, we have n hours of “free” time per day, we actually have 9 minutes here, 23 minutes there, 1 hour 6 minutes somewhere else, and so on.
Social commitments, meanwhile, tend to require not only that we have time in a block, but also, that the time around that block also be sufficiently free, for travelling, preparation, etc.
The result? “We must do this again, and not leave it so long next time!” we say, sincerely, to the friend whom we will next see again in approximately 17 months’ time.
The problem is how our many theoretically-small obligations reduce the rest of our time to “time confetti”, and that happens on the large scale like we saw above, as well as on the small scale of “Ah, I have an hour to relax between these two things” and then suddenly the time is gone, once again reduced to time confetti:
Time Confetti and the Broken Promise of Leisure
So, how to maintain human connection with people beyond those with whom we live?
Some is infinitely better than none
Let’s say you want to call a friend or relative. There may be generational differences in how much one is expected to arrange this by text first, vs just calling, but either way, you don’t have to have an open-ended block of time, and sometimes, it’s better if you don’t.
Establish, at the start of the call, “Before we get into catching up, how are we for time, by the way? For my part, I’ll have to go by such-and-such a time”, and then work with that.
The benefit of doing this is that you’ll both know enough about the time constraints to use the time appropriately; you won’t run out the clock on smalltalk before getting to something big, and you’ll both come away feeling satisfied that you shared and were shared-with in a meaningful fashion.
In contrast, guessing at time constraints can leave big things clipped off, or else result in someone “looking for a way to politely end this conversation that stopped being interesting a while ago but it’ll seem rude if I say I have to go now”, of the kind that results in someone not being so open to a call next time.
Don’t rush to dismiss texts as a medium for meaningful connection
When text messages were first a thing, you’ll remember how we were all working within a very short character limit and a cost-per-message. It was telegrams for the modern age, basically.
Nowadays, that isn’t so; we can write as much or as little as we like, and this has two benefits:
- We can have longer, meaningful conversations around the other stuff in our life. We can reply in seconds, or after making a cup of tea and thinking about it, or after our grocery-chopping trip, or whenever suits us. Suddenly, time confetti isn’t such a barrier to human connection. Writer’s example: my prime social time in this manner is when I’m cooking dinner (which is often about an hour). There’s no way I could have a phonecall while doing that; my bad hearing notwithstanding, I just have my hands full too often with much else going on. But texting? I can do that in the several-minute gaps between assorted culinary tasks, while I’m waiting for the kettle to boil or the onions to brown or whatever.
- Sometimes, the brevity makes it easier. A quick text saying “Hey, just to let you know I’m thinking of you, and hope your day is going well!”, or “Unrelated to anything: I was just thinking about how I’m glad to have you in my life; you’re a good friend, and I appreciate that more than I often remember to say. Anyway, that’s all; it was just on my mind. I hope your day is going well!”
(The cheery closing words in those last two text message examples help signify: “don’t worry, I’m fine and am not looking for anything from you”, which will help the recipient to relax, and counterintuitively, more likely to reply with some kind words of their own, knowing that they’re not signing up for a potentially deep talk when they also have time confetti issues going on)
Seize the moment (and also let it go)
You probably have many small interactions with strangers, most days. In the store, walking the dog, at the doctor’s office, etc. So, two things:
- Make smalltalk. And if you’re not one for traditional smalltalk topics (weather etc), or even if you are, a level-up is:
- Compliment sincerely. Straight out of “How To Win Friends And Influence People”, of course, but it creates a moment of genuine connection; you say a thing, their day is improved, they smile, you complete your business with a smile of your own and go about your day.
(of course, do steer clear of anything that could be interpreted as flirting, if that is not your intent, and really it should never be your intent when it comes to the captive audience of someone who will get fired if they’re not nice to you)
But, with a little practice, these little moments add up to a lot more human connection than if we treat the strangers with whom we interact as though they were merely part of the scenery.
Want more than that?
Check out:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Exercises That Fix 95% Of Your Problems
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well, your musculoskeletal problems, anyway! The exercises won’t, for example, do your taxes or deal with your loud neighbor for you. But, they will help your body be strong, supple, and pain-free:
20 minutes total
The exercises & what they do:
- Dead hang: improves shoulder health, decompresses the spine, and strengthens grip. Hang from a bar for 20–30 seconds, progressing to 1–2 minutes.
- Glute bridge: builds glute strength, improves core stability, and reduces lower back tension. Perform 2 sets of 10–15 reps, with variations like single-leg bridges or added weight.
- Farmer’s walk: a full-body workout that strengthens the shoulders, core, and grip while improving posture. Walk with weights for 30–60 seconds, 3 rounds, increasing weight or duration over time.
- Resting squat: enhances ankle, hip, and knee mobility, restoring natural functionality. Hold a deep squat for 20–30 seconds, progressing to 1–2 minutes. Use support for balance if necessary.
- Thread the needle: improves flexibility, reduces tension, and enhances rotational mobility. Perform slow, controlled rotations from an all-fours position, 2 sets of 10 reps per side.
Suggested 20-minute workout plan:
- Dead hang: 3 sets of 30 seconds
- Glute bridge: 2 sets of 10–15 reps
- Farmer’s walk: 30–60 seconds, 3 rounds
- Resting squat: hold for 20–30 seconds, 2–3 rounds
- Thread the needle: 2 sets of 10 reps per side
It is recommended to perform this routine 3 times per week with 1-minute rests between sets.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Share This Post
-
Beetroot vs Red Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to red cabbage, we picked the red cabbage.
Why?
Both are great, and both have their strengths!
In terms of macros, beetroot has very slightly more protein, carbs, and fiber, but the margins of difference are very small in each case. However, in terms of glycemic index, red cabbage has the considerably lower glycemic index, of 32 (low) as opposed to beetroot’s GI of 64 (medium). On the strength of this GI difference, we call this category a win for red cabbage.
In the category of vitamins, beetroot has more of vitamin B9, while red cabbage has a lot more of vitamins A, B1, B2, B3, B6, C, E, K, and choline. By strength of numbers and also by having very large margins of difference on most of those, red cabbage is the clear winner here.
When it comes to minerals, beetroot has more copper, magnesium, manganese, phosphorus, and potassium, while red cabbage has more calcium (and about ⅓ of the sodium). By the numbers, this is a win for beetroot, though it’s worth noting that the margins of difference were small, i.e. red cabbage was right behind beetroot on each of those.
Adding up the sections makes for an overall red cabbage win, but as we say, beetroot is great too, especially when it comes to minerals!
As ever, enjoy either or both; diversity is good.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do!
Enjoy!
Share This Post
-
“The Longevity Vitamin” (That’s Not A Vitamin)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Magic of Mushrooms
“The Longevity Vitamin that’s not a vitamin” is a great tagline for what’s actually an antioxidant amino acid nutraceutical, but in this case, we’re not the ones spearheading its PR, but rather, the Journal of Nutritional Science:
Is ergothioneine a “longevity vitamin” limited in the American diet?
It can be found in all foods, to some extent, but usually in much tinier amounts than would be useful. The reason for this is that it’s synthesized by a variety of microbes (mostly fungi and actinobacteria), and enters the food chain via vegetables that are grown in soil that contain such (which is basically all soil, unless you were to go out of your way to sterilize it, or something really unusually happened).
About those fungi? That includes common popular edible fungi, where it is found quite generously. An 85g (3oz) portion of (most) mushrooms contains about 5mg of ergothioneine, the consumption of which is associated with a 16% reduced all-cause mortality:
However… Most Americans don’t eat that many mushrooms, and those polled averaged 1.1mg/day ergothioneine (in contrast with, for example, Italians’ 4.6mg/day average).
Antioxidant properties
While its antioxidant properties aren’t the most exciting quality, they are worth a mention, on account of their potency:
The biology of ergothioneine, an antioxidant nutraceutical
This is also part of its potential bid to get classified as a vitamin, because…
❝Decreased blood and/or plasma levels of ergothioneine have been observed in some diseases, suggesting that a deficiency could be relevant to the disease onset or progression❞
Source: Ergothioneine: a diet-derived antioxidant with therapeutic potential
Healthy aging
Building on from the above, ergothioneine has been specifically identified as being associated with healthy aging and the prevention of cardiometabolic diseases:
❝An increasing body of evidence suggests ergothioneine may be an important dietary nutrient for the prevention of a variety of inflammatory and cardiometabolic diseases and ergothioneine has alternately been suggested as a vitamin, “longevity vitamin”, and nutraceutical❞
~ Dr. Bernadette Moore et al., citing more references every few words there
Source: Ergothioneine: an underrecognised dietary micronutrient required for healthy ageing?
Good for the heart = good for the brain
As a general rule of thumb, “what’s good for the heart is good for the brain” is almost always true, and it appears to be so in this case, too:
❝Ergothioneine crosses the blood–brain barrier and has been reported to have beneficial effects in the brain. In this study, we discuss the cytoprotective and neuroprotective properties of ergotheioneine, which may be harnessed for combating neurodegeneration and decline during aging.❞
Source: Ergothioneine: A Stress Vitamin with Antiaging, Vascular, and Neuroprotective Roles?
Want to get some?
You can just eat a portion of mushrooms per day! But if you don’t fancy that, it is available as a supplement in convenient 1/day capsule form too.
We don’t sell it, but for your convenience, here is an example product on Amazon
Enjoy!
Share This Post
Related Posts
-
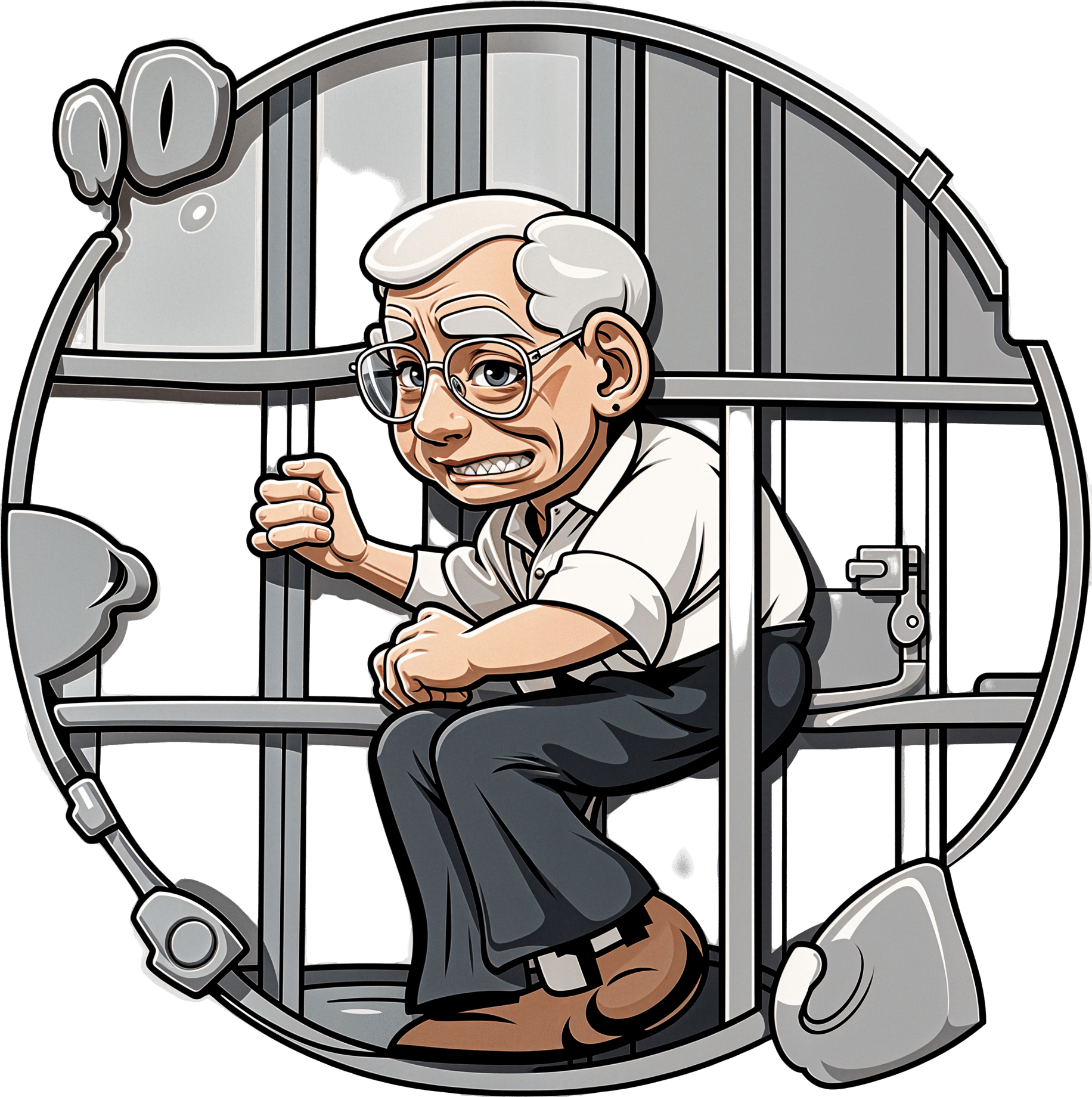
Older Americans Say They Feel Trapped in Medicare Advantage Plans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2016, Richard Timmins went to a free informational seminar to learn more about Medicare coverage.
“I listened to the insurance agent and, basically, he really promoted Medicare Advantage,” Timmins said. The agent described less expensive and broader coverage offered by the plans, which are funded largely by the government but administered by private insurance companies.
For Timmins, who is now 76, it made economic sense then to sign up. And his decision was great, for a while.
Then, three years ago, he noticed a lesion on his right earlobe.
“I have a family history of melanoma. And so, I was kind of tuned in to that and thinking about that,” Timmins said of the growth, which doctors later diagnosed as malignant melanoma. “It started to grow and started to become rather painful.”
Timmins, though, discovered that his enrollment in a Premera Blue Cross Medicare Advantage plan would mean a limited network of doctors and the potential need for preapproval, or prior authorization, from the insurer before getting care. The experience, he said, made getting care more difficult, and now he wants to switch back to traditional, government-administered Medicare.
But he can’t. And he’s not alone.
“I have very little control over my actual medical care,” he said, adding that he now advises friends not to sign up for the private plans. “I think that people are not understanding what Medicare Advantage is all about.”
Enrollment in Medicare Advantage plans has grown substantially in the past few decades, enticing more than half of all eligible people, primarily those 65 or older, with low premium costs and perks like dental and vision insurance. And as the private plans’ share of the Medicare patient pie has ballooned to 30.8 million people, so too have concerns about the insurers’ aggressive sales tactics and misleading coverage claims.
Enrollees, like Timmins, who sign on when they are healthy can find themselves trapped as they grow older and sicker.
“It’s one of those things that people might like them on the front end because of their low to zero premiums and if they are getting a couple of these extra benefits — the vision, dental, that kind of thing,” said Christine Huberty, a lead benefit specialist supervising attorney for the Greater Wisconsin Agency on Aging Resources.
“But it’s when they actually need to use it for these bigger issues,” Huberty said, “that’s when people realize, ‘Oh no, this isn’t going to help me at all.’”
Medicare pays private insurers a fixed amount per Medicare Advantage enrollee and in many cases also pays out bonuses, which the insurers can use to provide supplemental benefits. Huberty said those extra benefits work as an incentive to “get people to join the plan” but that the plans then “restrict the access to so many services and coverage for the bigger stuff.”
David Meyers, assistant professor of health services, policy, and practice at the Brown University School of Public Health, analyzed a decade of Medicare Advantage enrollment and found that about 50% of beneficiaries — rural and urban — left their contract by the end of five years. Most of those enrollees switched to another Medicare Advantage plan rather than traditional Medicare.
In the study, Meyers and his co-authors muse that switching plans could be a positive sign of a free marketplace but that it could also signal “unmeasured discontent” with Medicare Advantage.
“The problem is that once you get into Medicare Advantage, if you have a couple of chronic conditions and you want to leave Medicare Advantage, even if Medicare Advantage isn’t meeting your needs, you might not have any ability to switch back to traditional Medicare,” Meyers said.
Traditional Medicare can be too expensive for beneficiaries switching back from Medicare Advantage, he said. In traditional Medicare, enrollees pay a monthly premium and, after reaching a deductible, in most cases are expected to pay 20% of the cost of each nonhospital service or item they use. And there is no limit on how much an enrollee may have to pay as part of that 20% coinsurance if they end up using a lot of care, Meyers said.
To limit what they spend out-of-pocket, traditional Medicare enrollees typically sign up for supplemental insurance, such as employer coverage or a private Medigap policy. If they are low-income, Medicaid may provide that supplemental coverage.
But, Meyers said, there’s a catch: While beneficiaries who enrolled first in traditional Medicare are guaranteed to qualify for a Medigap policy without pricing based on their medical history, Medigap insurers can deny coverage to beneficiaries transferring from Medicare Advantage plans or base their prices on medical underwriting.
Only four states — Connecticut, Maine, Massachusetts, and New York — prohibit insurers from denying a Medigap policy if the enrollee has preexisting conditions such as diabetes or heart disease.
Paul Ginsburg is a former commissioner on the Medicare Payment Advisory Commission, also known as MedPAC. It’s a legislative branch agency that advises Congress on the Medicare program. He said the inability of enrollees to easily switch between Medicare Advantage and traditional Medicare during open enrollment periods is “a real concern in our system; it shouldn’t be that way.”
The federal government offers specific enrollment periods every year for switching plans. During Medicare’s open enrollment period, from Oct. 15 to Dec. 7, enrollees can switch out of their private plans to traditional, government-administered Medicare.
Medicare Advantage enrollees can also switch plans or transfer to traditional Medicare during another open enrollment period, from Jan. 1 to March 31.
“There are a lot of people that say, ‘Hey, I’d love to come back, but I can’t get Medigap anymore, or I’ll have to just pay a lot more,’” said Ginsburg, who is now a professor of health policy at the University of Southern California.
Timmins is one of those people. The retired veterinarian lives in a rural community on Whidbey Island just north of Seattle. It’s a rugged, idyllic landscape and a popular place for second homes, hiking, and the arts. But it’s also a bit remote.
While it’s typically harder to find doctors in rural areas, Timmins said he believes his Premera Blue Cross plan made it more challenging to get care for a variety of reasons, including the difficulty of finding and getting in to see specialists.
Nearly half of Medicare Advantage plan directories contained inaccurate information on what providers were available, according to the most recent federal review. Beginning in 2024, new or expanding Medicare Advantage plans must demonstrate compliance with federal network expectations or their applications could be denied.
Amanda Lansford, a Premera Blue Cross spokesperson, declined to comment on Timmins’ case. She said the plan meets federal network adequacy requirements as well as travel time and distance standards “to ensure members are not experiencing undue burdens when seeking care.”
Traditional Medicare allows beneficiaries to go to nearly any doctor or hospital in the U.S., and in most cases enrollees do not need approval to get services.
Timmins, who recently finished immunotherapy, said he doesn’t think he would be approved for a Medigap policy, “because of my health issue.” And if he were to get into one, Timmins said, it would likely be too expensive.
For now, Timmins said, he is staying with his Medicare Advantage plan.
“I’m getting older. More stuff is going to happen.”
There is also a chance, Timmins said, that his cancer could resurface: “I’m very aware of my mortality.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is “Extra Virgin” Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering, is the health difference important between extra virgin olive oil and regular?❞
Assuming that by “regular” you mean “virgin and still sold as a food product”, then there are health differences, but they’re not huge. Or at least: not nearly so big as the differences between those and other oils.
Virgin olive oil (sometimes simply sold as “olive oil”, with no claims of virginity) has been extracted by the same means as extra virgin olive oil, that is to say: purely mechanical.
The difference is that extra virgin olive oil comes from the first pressing*, so the free fatty acid content is slightly lower (later checked and validated and having to score under a 0.8% limit for “extra virgin” instead of 2% limit for a mere “virgin”).
*Fun fact: in Arabic, extra virgin is called “البكر الممتاز“, literally “the amazing first-born”, because of this feature!
It’s also slightly higher in mono-unsaturated fatty acids, which is a commensurately slight health improvement.
It’s very slightly lower in saturated fats, which is an especially slight health improvement, as the saturated fats in olive oil are amongst the healthiest saturated fats one can consume.
On which fats are which:
The truth about fats: the good, the bad, and the in-between
And our own previous discussion of saturated fats in particular:
Can Saturated Fats Be Healthy?
Probably the strongest extra health-benefit of extra virgin is that while that first pressing squeezes out oil with the lowest free fatty acid content, it squeezes out oil with the highest polyphenol content, along with other phytonutrients:
If you enjoy olive oil, then springing for extra virgin is worth it if that’s not financially onerous, both for health reasons and taste.
However, if mere “virgin” is what’s available, it’s no big deal to have that instead; it still has a very similar nutritional profile, and most of the same benefits.
Don’t settle for less than “virgin”, though.
While some virgin olive oils aren’t marked as such, if it says “refined” or “blended”, then skip it. These will have been extracted by chemical means and/or blended with completely different oils (e.g. canola, which has a very different nutritional profile), and sometimes with a dash of virgin or extra virgin, for the taste and/or so that they can claim in big writing on the label something like:
a blend of
EXTRA VIRGIN OLIVE OIL
and other oils…despite having only a tiny amount of extra virgin olive oil in it.
Different places have different regulations about what labels can claim.
The main countries that produce olives (and the EU, which contains and/or directly trades with those) have this set of rules:
International Olive Council: Designations and definitions of Olive Oils
…which must be abided by or marketers face heavy fines and sanctions.
In the US, the USDA has its own set of rules based on the above:
USDA | Olive Oil and Olive-Pomace Oil Grades and Standards
…which are voluntary (not protected by law), and marketers can pay to have their goods certified if they want.
So if you’re in the US, look for the USDA certification or it really could be:
- What the USDA calls “US virgin olive oil not fit for human consumption”, which in the IOC is called “lamp oil”*
- crude pomace-oil (oil made from the last bit of olive paste and then chemically treated)
- canola oil with a dash of olive oil
- anything yellow and oily, really
*This technically is virgin olive oil insofar as it was mechanically extracted, but with defects that prevent it from being sold as such, such as having a free fatty acid content above the cut-off, or just a bad taste/smell, or some sort of contamination.
See also: Potential Health Benefits of Olive Oil and Plant Polyphenols
(the above paper has a handy infographic if you scroll down just a little)
Where can I get some?
Your local supermarket, probably, but if you’d like to get some online, here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Curcumin (Turmeric) is worth its weight in gold
Not financially! But, this inexpensive golden spice has an impressive list of well-studied health benefits, for something so freely available in any supermarket, and there’s a reason it gets a place in “Dr. Greger’s Daily Dozen”, right up there with things like “leafy greens” and “berries” when it comes to superfoods.
Let’s do a quick run-down:
- It fights inflammation, and thus helps fight many diseases where inflammation is a factor (ranging from atherosclerosis to arthritis to Alzheimer’s and more)
- It has powerful antioxidant effects too
- It boosts brain-derived neurotropic factor (BDNF) and thus improves memory and attention
- It helps protect against heart disease…
- …and can give a 65% decreased risk of experiencing a heart attack
- It can help prevent cancer, and reduce cancerous lesions by 40%
- It’s also good against depression
- It even slows aging
In short, it’s—like we said—worth its weight in gold.
Quick advice though before we move on…
If you take curcumin with black pepper, it allows your body to use the curcumin around 2,000% better. This goes whether you’re cooking with both, or take them as a supplement (they’re commonly sold as a combo-capsule for this reason).
Want to get some?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: