Calculate (And Enjoy) The Perfect Night’s Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

This is Dr. Michael Breus, a clinical psychologist and sleep specialist, and he wants you to get a good night’s sleep, every night.
First, let’s assume you know a lot of good advice about how to do that already in terms of environment and preparation, etc. If you want a recap before proceeding, then we recommend:
Get Better Sleep: Beyond The Basics
Now, what does he want to add?
Wake up refreshed
Of course, how obtainable this is will depend on the previous night’s sleep, but there is something important we can do here regardless, and it’s: beat sleep inertia.
Sleep inertia is what happens when we wake up groggy (for reasons other than being ill, drugged, etc) rather than refreshed. It’s not actually related to how much sleep we have, though!
Rather, it pertains to whether we woke up during a sleep cycle, or between cycles:
- If we wake up between sleep cycles, we’ll avoid sleep inertia.
- If we wake up during a sleep cycle, we’ll be groggy.
Deep sleep generally occurs in 90-minute blocks, albeit secretly that is generally 3× 20 minute blocks in a trenchcoat, with transition periods between, during which the brainwaves change frequency.
REM sleep generally occurs in 20 minute blocks, and will usually arrive in series towards the end of our natural sleep period, to fit neatly into the last 90-minute cycle.
Sometimes these will appear a little out of order, because we are complicated organic beings, but those are the general trends.
In any case, the take-away here is: interrupt them at your peril. You need to wake up between cycles. There are two ways you can do this:
- Carefully calculate everything, and set a very precise alarm clock (this will work so long as you are correct in guessing how long it will take you to fall asleep)
- Use a “sunrise” lamp alarm clock, that in the hour approaching your set alarm time, will gradually increase the light. Because the body will not naturally wake up during a cycle unless a threat is perceived (loud noise, physical rousing, etc), the sunrise lamp method means that you will wake up between sleep cycles at some point during that hour (towards the beginning or end, depending on what your sleep balance/debt is like).
Do not sleep in (even if you have a sleep debt); it will throw everything out.
Caffeine will not help much in the morning
Assuming you got a reasonable night’s sleep, your brain has been cleansed of adenosine (a sleepy chemical), and if you are suffering from sleep inertia, the grogginess is due to melatonin (a different sleepy chemical).
Caffeine is an adenosine receptor blocker, so that will do nothing to mitigate the effects of melatonin in your brain that doesn’t have any meaningful quantity of adenosine in it in the morning.
Adenosine gradually accumulates in the brain over the course of the day (and then gets washed out while we sleep), so if you’re sleepy in the afternoon (for reasons other than: you just had a nap and now have sleep inertia again), then caffeine can block that adenosine in the afternoon.
Of course, caffeine is also a stimulant (it increases adrenaline levels and promotes vasoconstriction), but its effects at healthily small doses are modest for most people, and you’d do better by splashing cold water on your face and/or listening to some upbeat music.
Learn more: The Two Sides Of Caffeine
Time your naps correctly (if you take naps)
Dr. Breus has a lot to say about this, based on a lot of clinical research, but as it’s entirely consistent with what we’ve written before (based on the exact same research), to save space we’ll link to that here:
How To Be An Expert Nap-Artist (With No “Sleep-Hangovers”)
Calculate your bedtime correctly
Remember what we said about sleep cycles? This means that that famous “7–9 hours sleep” is actually “either 7½ or 9 hours sleep”—because those are multiples of 90 minutes, whereas 8 hours (for example) is not.
So, consider the time you want to get up (ideally, this should be relatively early, and the same time every day), and then count backwards either 7½ or 9 hours sleep (you choose), add 20–30 minutes to fall asleep, and that’s your bedtime.
So for example: if you want to have 7½ hours sleep and get up at 6am, then your bedtime is anywhere between 10pm and 10:10pm.
Remember how we said not to sleep in, even if you have a sleep debt? Now is the time to pay it off, if you have one. If you normally sleep 7½ hours, then make tonight a 9-hour sleep (plus 20–30 minutes to fall asleep). This means you’ll still get up at 6am, but your bedtime is now anywhere between 8:30pm and 8:40pm.
Want to know more from Dr. Breus?
You might like this excellent book of his that we reviewed a while back:
The Power of When – by Dr. Michael Breus
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can You Step Backwards Without Your Foot Or Torso Turning Out?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Walking backwards is often overlooked, but research shows it can enhance forward walking, especially in stroke patients; it has other benefits for everyone else, too. The physiotherapists at Fitness4Life Physical Therapy explain:
…and one step back
How it works: walking backwards heightens proprioception and stimulates muscles, improving balance and posture. Additionally, our daily lives tend to involve forward-leaning postures, causing upper back bending, and walking backwards helps counterbalance this.
Extra benefits: training to walk backwards can reduce the risk of falls, as stepping back is a common movement that is often untrained.
Exercise: try doing backwards lunges, to assess your skill and balance while moving backward. If foot rotation or torso rotation occurs during the exercise, then there’s room for improvement. Correcting these movements is then simply a matter of practicing backward lunges without turning.
10almonds tip: any exercise is only as good as your will to actually do it. For this reason, dancing is a great exercise in this case, as almost all forms of dance involve stepping backwards (in order to have steps without travelling somewhere, forwards steps are usually balanced with backwards ones)
For more on all this, plus a visual demonstration of the exercise, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special ← About how to avoid falling, and how to avoid (and failing that, at least minimize) injury if you do fall. If you think this only happens to other/older people, remember, there’s a first time for everything, so it is better to be prepared in advance!
Take care!
Share This Post
-
The Compass of Pleasure – by Dr. David Linden
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of books about addiction, so what sets this one apart?
Mostly, it’s that this one maintains that addiction is neither good nor bad per se—just, some behaviors and circumstances are. Behaviors and circumstances caused, directly or indirectly, by addiction.
But, Dr. Linden argues, not every addiction has to be so. Especially behavioral addictions; the rush of dopamine one gets from a good session at the gym or learning a new language, that’s not a bad thing, even if they can fundamentally be addictions too.
Similarly, we wouldn’t be here as a species without some things that rely on some of the same biochemistry as addictions; orgasms and eating food, for example. Yet, those very same urges can also inconvenience us, and in the case of foods and other substances, can harm our health.
In this book, the case is made for shifting our addictive tendencies to healthier addictions, and enough information is given to help us do so.
Bottom line: if you’d like to understand what is going on when you get waylaid by some temptation, and how to be tempted to better things, this book can give the understanding to do just that.
Click here to check out The Compass of Pleasure, and make yours work in your favor!
Share This Post
-
Jamaican Coconut Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a great dish that can be enjoyed hot or cold, as a main or as a side. It has carbs, proteins, healthy fats, fiber, as well as an array of healthy phytochemicals. Not to mention, a great taste!
You will need
- 1 cup wholegrain basmati rice (it may also be called “brown basmati rice“; this is the same) (traditional recipe calls for pudding rice, but we’re going with the healthier option here)
- 2 cans (each 12 z / 400g) coconut milk
- 2 cups (or 2 cans, of which the drained weight is comparable to a cup each) cooked black beans. If you cook them yourself, this is better, as you will be able to cook them more al dente than you can get from a can, and this firmness is desirable. But canned is fine if that’s what’s available.
- 1 large red onion, finely chopped
- ½ cup low-sodium vegetable stock (ideally you made this yourself from vegetable offcuts you saved in the freezer for this purpose, but failing that, low-sodium stock cubes can be bought at any large supermarket)
- 2 serrano chilis, finely chopped
- 1 Scotch bonnet chili, without doing anything to it
- 1 tbsp black pepper, coarse ground
- 1 tbsp chia seeds
- 1 tbsp coconut oil
- Garnish: parsley, chopped
Note: we have erred on the side of low-heat when it comes to the chilis. If you know that you and (if applicable) everyone else eating would enjoy more heat, add more heat. If not, let extra heat be added at the table via your hot sauce of choice. Sounds heretical, but it ensures everyone gets the right amount! It’s easy to add heat than to take it out, after all.
However: if you do end up with too much heat in this or any other dish, adding acid will usually help to neutralize that. In the case of this dish, we’d recommend lime juice as a complementary flavor.
Method
(we suggest you read everything at least once before doing anything)
1) In a big sauté pan, add the coconut oil, melt it if not already melted, and add the chopped onion and the chopped chilis, at a temperature sufficient to sizzle. Keep them all moving. Once the coconut oil is absorbed into the onion (this will happen before the onion is fully cooked), add the vegetable stock, followed by the coconut milk; mix it all gently to create a smooth consistency.
2) Add the rice, chia seeds, and black pepper; mix it all gently but thoroughly; turn the temperature to a simmer, and add the Scotch bonnet chili, without cutting it at all.
3) Cover and keep on low for about 20–30 minutes until the rice is looking done. Check on it periodically to make sure it’s not running out of liquid, but resist the urge to stir it; it shouldn’t be burning but paradoxically, once you start stirring you can’t stop or it will definitely burn.
4) Take out the Scotch bonnet chili, and discard*. Add the black beans.
*its job was to add flavor without adding the high-level heat of that particular chili. If you’re a regular heat-fiend, feel free to experiment with using sliced Scotch bonnet chilis instead of serrano chilis; just be aware that there’s a big difference in heat. Only do this if you really like heat. Using it the way we described in the main recipe is what’s traditional in the Caribbean, by the way.
5) Now you can (and in fact must) stir, to mix in the black beans and bring them back to temperature within the dish. Be aware that once you start stirring, you need to keep stirring until you’re ready to take it off the heat.
6) Serve, adding the parsley garnish.
(this example went light on the beans; our recipe includes more for a heartier dish)
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Should You Go Light Or Heavy On Carbs?
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Burn! How To Boost Your Metabolism
- Capsaicin For Weight Loss And Against Inflammation
Take care!
Share This Post
Related Posts
-
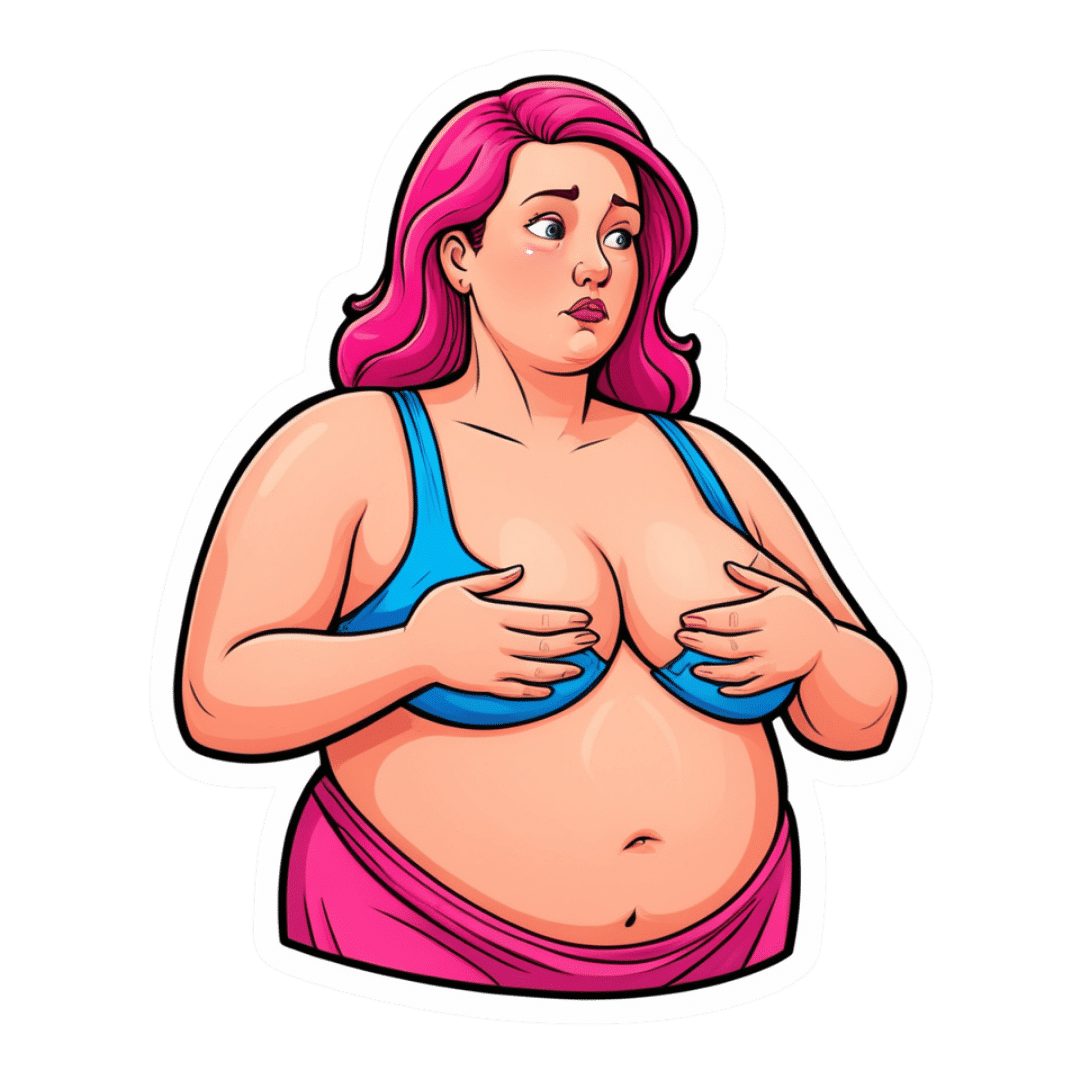
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll get straight to it:
More than 120 million Americans have diabetes or pre-diabetes, and Triple-Negative Breast Cancer (TNBC)* is the most aggressive breast cancer form.
These may seem like unrelated statements, until we consider that patients with obesity-driven** diabetes have much worse TNBC outcomes.
*The “triple-negative” refers to:
- the cancer cells don’t have estrogen receptors
- the cancer cells don’t have progesterone receptors
- the cancer cells don’t make the protein HER2, or at least not in clinically relevant amounts.
**with regard to “obesity-driven”, that is what it is called, and the presence of excess fat does play an important role as we will see, but the fundamental culprit is insulin resistance, as we will also see.
The connection
Superficially, the connection between obesity-driven diabetes and worse TNBC outcomes could be put down to “a person who is already unhealthy will generally fare worse in most health things than an otherwise healthy person”. And, in and of itself, that’s a fair point. Comorbidities certainly do tend to flock together and make each other worse.
On the flipside, this does also mean that the more points of good health we have in our favor, the greater our chances of faring better if something (such as a cancer) does strike us regardless. So, there’s a fair motivation to always keep on top of all aspects of health, so far as reasonably possible.
However, there’s more to it than that.
Dr. Naomi Ko et al., a team of researchers at Boston University, found that diabetes alters breast cancer biology, making TNBC more aggressive and increasing the risk of brain metastasis (i.e., the cancer spreading to the brain).
Specifically, exosomes from fat cells carry microRNAs that worsen TNBC behavior, enhancing the cancer’s:
- cell growth
- movement
- survival under stress
- brain colonization
This also means that certain microRNA patterns predict breast cancer progression and/or survival.
You can find the paper itself here:
Insulin Resistance Increases TNBC Aggressiveness and Brain Metastasis via Adipocyte-derived Exosomes
Why this matters
The researchers argue that their findings suggest the need for special monitoring and treatment for TNBC patients with metabolic disorders like diabetes, and that treating underlying conditions (such as diabetes) alongside cancer is likely to improve outcomes.
On an individual level rather than systemic (assuming you, dear reader, to be a private individual who is not, for example, in charge of health policy for a region, or something like that), what this means is:
We must avoid carrying too much excess fat yes, and/but we must also particularly focus on avoiding/reversing insulin resistance, which can be a silent killer even without excess adiposity, because the noticeable signs and symptoms (including blood sugar irregularities) occur only well into insulin resistance, when the poor overworked pancreas can no longer crank out enough insulin to keep things ticking over.
With that in mind, do check out in particular the two following articles:
How To Lose Weight (Healthily!) ← if applicable. If on the other hand you’re already in the “healthy” body fat percentage range of 20–25% for women or 15–20% for men, then losing what fat you have will not be beneficial, and may even be harmful, depending on other factors.
How To Avoid & Reverse Insulin Resistance ← this one’s super-important!
And of course:
How To Triple Your Breast Cancer Survival Chances
And if you want to get really well-informed, then we highly recommend checking out:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Critical Signs Of Blood Clots That You Shouldn’t Ignore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Blood clots can form as part of deep vein thrombosis or for other reasons; wherever they form (unless they are just doing their job healing a wound) they can cause problems. But how to know what’s going on inside our body?
Telltale signs
Our usual medical/legal disclaimer applies here, and we are not doctors, let alone your doctors, and even if we were we couldn’t diagnose from afar… But for educational purposes, here are the eight signs from the video:
- Swelling: especially if only on one leg (assuming you have no injury to account for it), which may feel tight and uncomfortable
- Warmness: does the area warmer to the touch? This may be because of the body’s inflammatory response trying to deal with a blood clot
- Tenderness: again, caused by the inflammation in response to the clot
- Discolored skin: it could be reddish, or bruise-like. This could be patchy or spread over a larger area, because of a clot blocking the flow of blood
- Shortness of breath: if a clot makes it to the lungs, it can cause extra problems there (pulmonary embolism), and shortness of breath is the first sign of this
- Coughing up blood: less common than the above but a much more serious sign; get thee to a hospital
- Chest pain: a sharp or stabbing pain, in particular. The pain may worsen with deep breaths or coughing. Again, seek medical attention.
For more on recognizing these signs (including helpful visuals), and more on what to do about them and how to avoid them in the first place, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might like to read:
Dietary Changes for Artery Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cognitive Enhancement Without Drugs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cognitive Enhancement Without Drugs
This is Elizabeth Ricker. She’s a Harvard-and-MIT-trained neuroscientist and researcher, who now runs the “Citizen Science” DIY-neurohacking organization, NeuroEducate.
Sounds fun! What’s it about?
The philosophy that spurs on her research and practice can be summed up as follows:
❝I’m not going to leave my brain up to my doctor or [anyone else]… My brain is my own responsibility, and I’m going to do the best that I can to optimize it❞
Her goal is not just to optimize her own brain though; she wants to make the science accessible to everyone.
What’s this about Citizen Science?
“Citizen Science” is the idea that while there’s definitely an important role in society for career academics, science itself should be accessible to all. And, not just the conclusions, but the process too.
This can take the form of huge experiments, often facilitated these days by apps where we opt-in to allow our health metrics (for example) to be collated with many thousands of others, for science. It can also involve such things as we talked about recently, getting our own raw genetic data and “running the numbers” at home to get far more comprehensive and direct information than the genetic testing company would ever provide us.
For Ricker, her focus is on the neuroscience side of biohacking, thus, neurohacking.
I’m ready to hack my brain! Do I need a drill?
Happily not! Although… Bone drills for the skull are very convenient instruments that make it quite hard to go wrong even with minimal training. The drill bit has a little step/ledge partway down, which means you can only drill through the thickness of the skull itself, before the bone meeting the wider part of the bit stops you from accidentally drilling into the brain. Still, please don’t do this at home.
What you can do at home is a different kind of self-experimentation…
If you want to consider which things are genuinely resulting in cognitive enhancement and which things are not, you need to approach the matter like a scientist. That means going about it in an organized fashion, and recording results.
There are several ways cognitive enhancement can be measured, including:
- Learning and memory
- Executive function
- Emotional regulation
- Creative intelligence
Let’s look at each of them, and what can be done. We don’t have a lot of room here; we’re a newsletter not a book, but we’ll cover one of Ricker’s approaches for each:
Learning and memory
This one’s easy. We’re going to leverage neuroplasticity (neurons that fire together, wire together!) by simple practice, and introduce an extra element to go alongside your recall. Perhaps a scent, or a certain item of clothing. Tell yourself that clinical studies have shown that this will boost your recall. It’s true, but that’s not what’s important; what’s important is that you believe it, and bring the placebo effect to bear on your endeavors.
You can test your memory with word lists, generated randomly by AI, such as this one:
You’ll soon find your memory improving—but don’t take our word for it!
Executive function
Executive function is the aspect of your brain that tells the other parts how to work, when to work, and when to stop working. If you’ve ever spent 30 minutes thinking “I need to get up” but you were stuck in scrolling social media, that was executive dysfunction.
This can be trained using the Stroop Color and Word Test, which shows you words, specifically the names of colors, which will themselves be colored, but not necessarily in the color the word pertains to. So for example, you might be shown the word “red”, colored green. Your task is to declare either the color of the word only, ignoring the word itself, or the meaning of the word only, ignoring its appearance. It can be quite challenging, but you’ll get better quite quickly:
The Stroop Test: Online Version
Emotional Regulation
This is the ability to not blow up angrily at the person with whom you need to be diplomatic, or to refrain from laughing when you thought of something funny in a sombre situation.
It’s an important part of cognitive function, and success or failure can have quite far-reaching consequences in life. And, it can be trained too.
There’s no online widget for this one, but: when and if you’re in a position to safely* do so, think about something that normally triggers a strong unwanted emotional reaction. It doesn’t have to be something life-shattering, but just something that you feel in some way bad about. Hold this in your mind, sit with it, and practice mindfulness. The idea is to be able to hold the unpleasant idea in your mind, without becoming reactive to it, or escaping to more pleasant distractions. Build this up.
*if you perchance have PTSD, C-PTSD, or an emotional regulation disorder, you might want to talk this one through with a qualified professional first.
Creative Intelligence
Another important cognitive skill, and again, one that can be cultivated and grown.
The trick here is volume. A good, repeatable test is to think of a common object (e.g. a rock, a towel, a banana) and, within a time constraint (such as 15 minutes) list how many uses you can think of for that item.
Writer’s storytime: once upon a time, I was sorting through an inventory of medical equipment with a colleague, and suggested throwing out our old arterial clamps, as we had newer, better ones—in abundance. My colleague didn’t want to part with them, so I challenged him “Give me one use for these, something we could in some possible world use them for that the new clamps don’t do better, and we’ll keep them”. He said “Thumbscrews”, and I threw my hands up in defeat, saying “Fine!”, as he had technically fulfilled my condition.
What’s the hack to improve this one? Just more volume. Creativity, as it turns out, isn’t something we can expend—like a muscle, it grows the more we use it. And because the above test is repeatable (with different objects), you can track your progress.
And if you feel like using your grown creative muscle to write/paint/compose/etc your magnum opus, great! Or if you just want to apply it to the problem-solving of everyday life, also great!
In summary…
Our brain is a wonderful organ with many functions. Society expects us to lose these as we get older, but the simple, scientific truth is that we can not only maintain our cognitive function, but also enhance and grow it as we go.
Want to know more from today’s featured expert?
You might enjoy her book, “Smarter Tomorrow”, which we reviewed back in March
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: