What’s Missing from Medicine – by Dr. Saray Stancic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”, Dr. Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the treatments presented.
Taking an evidence-based lifestyle medicine approach, she was able to not only manage her illness sufficiently to resume her normal activities, but even when so far as to run a marathon, and today boasts a symptom-free, active life.
The subtitular six lifestyle changes are not too shocking, and include a plants-centric diet, good exercise, good sleep, stress management, avoidance of substance abuses, and a fostering of social connections, but the value here is in what she has to say about each, especially the ones that aren’t so self-explanatory and/or can even cause harm if done incorrectly (such as exercise, for example).
The style is on the academic end of pop-science, of the kind that has frequent data tables, lots of statistics, and an extensive bibliography, but is still very readable.
Bottom line: if you are faced with a chronic disease, or even just an increased risk of some chronic disease, or simply like to not take chances, then this is a high-value book for you.
Click here to check out What’s Missing From Medicine, and enjoy chronic good health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
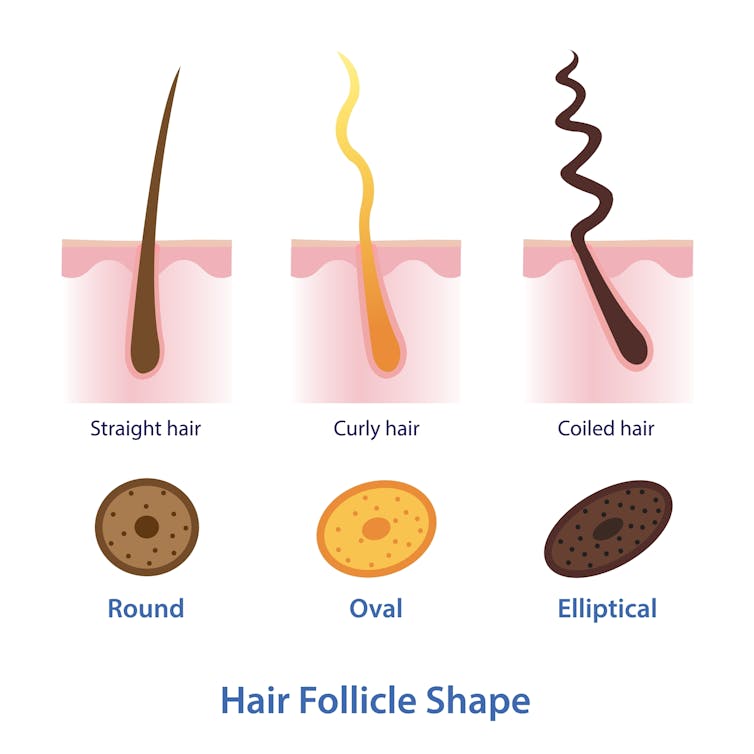
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.
Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.
Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.
Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Glutathione: More Than An Antioxidant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Glutathione’s Benefits: The Usual And The Unique
Glutathione is a powerful antioxidant that does all the things we might reasonably expect an antioxidant to do, plus some beneficial quirks of its own.
We do make glutathione in our bodies, but we can also get it from our diet, and of course, we can also supplement it.
What foods is it in?
It’s in a lot of foods, but some top examples include:
- turmeric
- avocado
- asparagus
- almonds
- cruciferous vegetables
- watermelon
- garlic
For a fuller list and discussion, see:
What does it do?
Let’s start with the obvious; as with most things that are antioxidant, it is also anti-inflammatory. Increasing or decreasing glutathione levels is associated with decreased or increased inflammation, respectively. For example:
It being anti-inflammatory also means it can be beneficial in calming autoimmune disorders:
Glutathione: a key player in autoimmunity
And to complete the triad of “those three things that generally go together”, yes, this means it also has anticancer potential, but watch out!
❝Although in healthy cells [glutathione] is crucial for the removal and detoxification of carcinogens, elevated [glutathione] levels in tumor cells are associated with tumor progression and increased resistance to chemotherapeutic drugs❞
~ Dr. Miroslava Cuperlovic-Culf et al.
Read in full: Role of Glutathione in Cancer: From Mechanisms to Therapies
So in other words, when it comes to cancer risk management, glutathione is a great preventative, but the opposite of a cure.
What were those “beneficial quirks of its own”?
They are mainly twofold, and the first is that it improves insulin sensitivity. There are many studies showing this, but here’s a recent one from earlier this year:
The Role of Glutathione and Its Precursors in Type 2 Diabetes
The other main “beneficial quirk of its own” is that it helps prevent and/or reverse non-alcoholic fatty liver disease, as in this study from last year:
Because of glutathione’s presence in nuts, fruits, and vegetables, this makes it a great thing to work in tandem with a dietary approach to preventing/reversing NAFLD, by the way:
Anything else?
It’s being investigated as a potential treatment for Parkinson’s disease symptoms, but the science is young for this one, so there is no definitive recommendation yet in this case. If you’re interested in that, though, do check out the current state of the science at:
Potential use of glutathione as a treatment for Parkinson’s disease
Is it safe?
While there is no 100% blanket statement of safety that can ever be made about anything (even water can kill people, and oxygen ultimately kills everyone that something else doesn’t get first), glutathione has one of the safest general safety profiles possible, with the exception we noted earlier (if you have cancer, it is probably better to skip this one unless an oncologist or similar advises you otherwise).
As ever, do speak with your doctor/pharmacist to be sure in any case, though!
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Eggs: Nutritional Powerhouse or Heart-Health Timebomb?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eggs: All Things In Moderation?
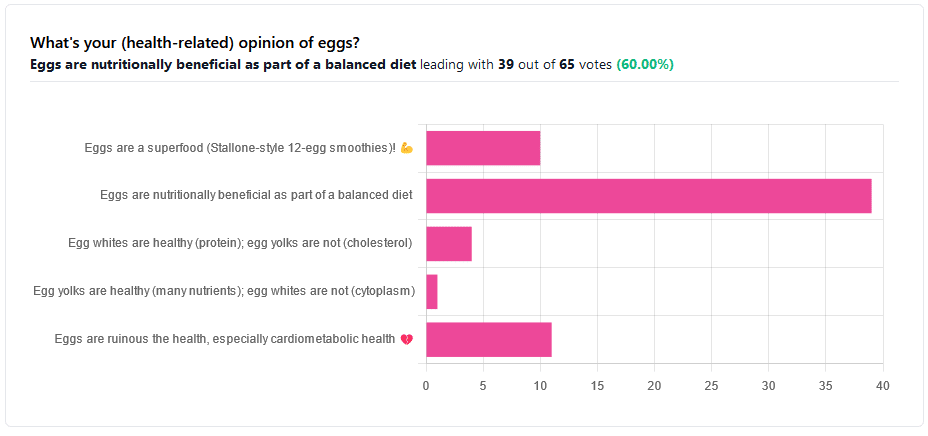
We asked you for your (health-related) opinion on eggs. We specified that, for the sake of simplicity, let’s say that they are from happy healthy backyard hens who enjoy a good diet.
Apparently this one wasn’t as controversial as it might have been! We (for myth-busting purposes) try to pick something polarizing and sometimes even contentious for our Friday editions, and pick apart what science lies underneath public perceptions.
However, more than half (in fact, 60%) of the subscribers who voted in the poll voted for “Eggs are nutritionally beneficial as part of a balanced diet”, which very moderate statement is indeed pretty much the global scientific consensus.
Still, we’ve a main feature to write, so let’s look at the science, and what the other 40% had in mind:
Eggs are ruinous to health, especially cardiometabolic health: True or False?
False, per best current science, anyway!
Scientific consensus has changed over the years. We learned about cholesterol, then we learned about different types of cholesterol, and now we’ve even learned about in some instances even elevated levels of “bad” cholesterol aren’t necessarily a cause of cardiometabolic disorders so much as a symptom—especially in women.
Not to derail this main feature about eggs (rather than just cholesterol), but for those who missed it, this is actually really interesting: basically, research (pertaining to the use of statins) has found that in women, higher LDL levels aren’t anywhere near the same kind of risk factor as they are for men, and thus may mean that statins (whose main job is reducing LDL) may be much less helpful for women than for men, and more likely to cause unwanted serious side effects in women.
Check out our previous main feature about this: Statins: His & Hers?
But, for back on topic, several large studies (totalling 177,000 people in long-term studies in 50 countries) found:
❝Results from the three cohorts and from the updated meta-analysis show that moderate egg consumption (up to one egg per day) is not associated with cardiovascular disease risk overall, and is associated with potentially lower cardiovascular disease risk in Asian populations.❞
Egg whites are healthy (protein); egg yolks are not (cholesterol): True or False?
True and False, respectively. That is to say, egg whites are healthy (protein), and egg yolks are also healthy (many nutrients).
We talked a bit already about cholesterol, so we’ll not rehash that here. As to the rest:
Eggs are one of the most nutritionally dense foods around. After all, they have everything required to allow a cluster of cells to become a whole baby chick. That’s a lot of body-building!
They’re even more nutritionally heavy-hitters if you get omega-3 enriched eggs, which means the hens were fed extra omega-3, usually in the form of flax seeds.
Also, free-range is better healthwise than others. Do bear in mind that unless they really are from your backyard, or a neighbor’s, chances are that the reality is not what the advertising depicts, though. There are industry minimum standards to be able to advertise as “free-range”, and those standards are a) quite low b) often ignored, because an occasional fine is cheaper than maintaining good conditions.
So if you can look after your own hens, or get them from somewhere that you can see for yourself how they are looked after, so much the better!
Check out the differences side-by-side, though:
Pastured vs Omega-3 vs “Conventional” Eggs: What’s the Difference?
Stallone-style 12-egg smoothies are healthy: True or False?
False, at least if taken with any regularity. One can indeed have too much of a good thing.
So, what’s the “right amount” to eat?
It may vary depending on individual factors (including age and ethnicity), but a good average, according to science, is to keep it to 3 eggs or fewer per day. There are a lot of studies, but we only have so much room here, so we’ll pick one. Its findings are representative of (and in keeping with) the many other studies we looked at, so this seems uncontroversial scientifically:
❝Intake of 1 egg/d was sufficient to increase HDL function and large-LDL particle concentration; however, intake of 2-3 eggs/d supported greater improvements in HDL function as well as increased plasma carotenoids. Overall, intake of ≤3 eggs/d favored a less atherogenic LDL particle profile, improved HDL function, and increased plasma antioxidants in young, healthy adults.❞
Enjoy!
Share This Post
Related Posts
-
Artichoke vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to broccoli, we picked the artichoke.
Why?
Both have their strengths, and it was close! But…
In terms of macros, artichoke has about 2x the fiber (which is lots, because broccoli is already good for this) and more protein, for only slightly more carbs, making it the nutrient dense choice in all respects, and especially in the case of fiber.
In the category of vitamins, artichoke has more of vitamins B3, B9, and choline, while broccoli has more of vitamins A, B2, B5, B6, C, E, and K, thus winning this round.
When it comes to minerals, artichoke has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while broccoli has more calcium and selenium, handing artichoke the win again here.
Looking at polyphenols, both have an abundance; artichoke has more by total mass (in terms of mg/100g) and is especially rich in luteolin and phenolic acids, but broccoli has some that artichoke doesn’t have (such as quercetin and kaempferol). We could reasonably call this a tie or a win for artichoke on strength of numbers; either way, it doesn’t change the end result:
Adding up the sections makes for an overall win for artichoke, but of course, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Soy Beans vs Kidney Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soy beans to kidney beans, we picked the soy.
Why?
In terms of macros, soy has 2x the protein, while kidney beans have nearly 3x the carbs and very slightly more fiber. Ratio-wise, the “very slightly more fiber” does not offset the “nearly 3x the carbs” when it comes to glycemic index (though both are still good, really, but this is a head-to-head so the comparison is relevant), and 2x the protein is also quite a bonus, so this category’s an easy win for soy.
In the category of vitamins, soy beans have more of vitamins A, B2, B6, C, E, K, and choline, while kidney beans have more of vitamins B3, B5, and B9, thus making for a 7:3 win for soy.
When it comes to minerals, soy beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while kidney beans are not higher in any mineral. Another clear win for soy.
Adding up the three strong wins for soy, makes for an overall easy win for soy. Still, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Plant vs Animal Protein: Head to Head
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health & Happiness From Outside & In
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A friend in need…
In a recent large (n=3,486) poll across the US:
- 90% of people aged 50 and older say they have at least one close friend
- 75% say they have enough close friends
- 70% of those with a close friend say they can definitely count on them to provide health-related support
However, those numbers shrink by half when it comes to people whose physical and/or mental health is not so great, resulting in a negative feedback loop of fewer close friends whom one sees less often, and progressively worse physical and/or mental health. In other words, the healthier you are, the more likely you are to have a friend who’ll support you in your health:
Read in full: Friendships promote healthier living in older adults, says new survey
Related: How To Beat Loneliness & Isolation
Kindness makes a difference to healthcare outcomes
Defining kindness as action-oriented, positively focused, and purposeful in nature, this sets kindness apart from compassion and empathy, when it’s otherwise often been conflated with those, and thus overlooked. This also means that kindness can still be effected when clinicians are too burned-out to be compassionate, and/or when patients are not in a state of mind where empathy is useful.
Furthermore, unkindness (again, as defined by this review) was found in large studies to be the root cause of ¾ of patient harm events in hospital settings. This means that far from being a wishy-washy abstraction, kindness/unkindness can be a very serious factor when it comes to healthcare outcomes:
Read in full: Review suggests kindness could make for better health care
Related: The Human Touch vs AI, The Doctor That Never Tires
The gift of health?
🎵 Last Christmas, I gave you my heart
Which turned out to be a silly idea
This year, to save me from tears
I’ll just get you a Fitbit or something🎵Health & happiness go hand in hand, so does that make health stuff a good gift? It can do! But there are also plenty of opportunities for misfires.
For example, getting someone a gym membership when they don’t have time for that may not help them at all, and sports equipment that they’ll use once and then leave to gather dust might not be great either. In contrast, the American Heart Association recommends to first consider what they enjoy doing, and work with that, and ideally make it something versatile and/or portable. Wearable gadgets are a fine option for many, but a gift doesn’t have to be fancy to be good—with a blood pressure monitoring cuff being a suggestion from Dr. Sperling (a professor of preventative cardiology):
Read in full: Oh, there’s no gift like health for the holidays
Related: Here’s Where Activity Trackers Help (And Also Where They Don’t)
How you use social media matters more than how much
A study commissioned by the European Commission’s Joint Research Centre found that while the quantity of time one spends on social media is not associated (positively or negatively) with loneliness, they did find a correlation between passive (as opposed to engaged) use of social media, and loneliness. In other words, people who were chatting with friends less, were more lonely! Shocking news.
While the findings may seem obvious, it does present a call-to-action for anyone who is feeling lonely: to use social media not just to see what everyone else is up to, but also, to reach out to people.
Read in full: Unpacking the link between social media and loneliness
Related: Make Social Media Work For Your Mental Health Rather Than Against It
Gut-only antidepressants
Many antidepressants work by increasing serotonin levels in the brain; a new study suggests that targeting antidepressants to work only in the gut (which is where serotonin is made, not the brain) could not only be an effective treatment for mood disorders, but also cause fewer adverse side-effects:
Read in full: Antidepressants may act in gut to reduce depression and anxiety
Related: Antidepressants: Personalization Is Key!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: